INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is spinal dysraphism?
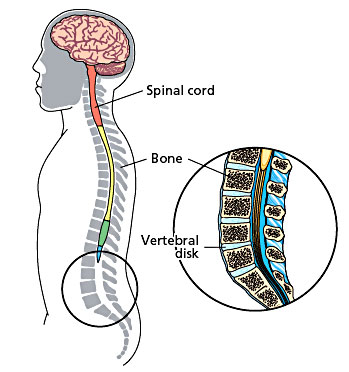
In early development, the brain and spinal cord start as a tube-like structure called the ‘neural tube’ that is open at either end. These openings close within the first weeks of pregnancy, and the neural tube continues to grow and fold, eventually forming the brain and spinal cord.
If the tube fails to close properly, this results in a group of problems called ‘neural tube defects’. Spinal dysphraism is the term used to describe what happens when the spinal column (backbone) fails to form properly. This happens very early in pregnancy, before the end of the fourth week. There are two types of spinal dysphraism: open, also called spina bifida aperta or myelomeningocele, or closed, also called spina bifida occulta.
The open myelomeningocele type accounts for 75 per cent of all cases of spina bifida. In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
Open Neural Tube Defects
In closed spinal dysphraism, the spinal cord (a tube-like structure containing nerves) and its coverings do not protrude through the back unlike in the open type. On its own, closed spinal dysphraism is unlikely to cause any problems, and many people have the condition without ever knowing it. However, it can be associated with other conditions that could lead to problems with movement and bladder control.
Closed Neural Tube Defect
Many children have a ‘tethered cord’, which is the term used when the lower end of the spinal cord is attached to the lower bones of the spinal column rather than hanging freely as it should. Normally the spinal column grows more quickly than the spinal cord, so that by the time the baby is born, the spinal cord has moved higher up the spinal column. If the cord is tethered, the spinal cord and nerves are stretched, reducing their ability to carry messages to and from the brain and causing pain. Growth spurts can stretch the spinal cord and nerves, causing problems with leg movement and bladder and bowel control.
What are the symptoms of closed spinal dysphraism?
In many people, there may be no symptoms at all. However, a birthmark, hairy patch or dermal sinus in the lower back area may lead doctors to suspect that a child has closed spinal dysphraism. Other children may develop repeated bouts of meningitis for which no cause can be found or may have problems keeping dry (urinary incontinence) that cannot be explained. If it not diagnosed until early childhood, the first sign might be weakness or unevenness of the legs or talipes (clubfeet) affecting one of both limbs. Back or leg pain might be a problem too. If these symptoms are due to a tethered cord they may get worse as the child grows. Treatment by surgery tends to be suggested only when a child shows signs that his or her condition is getting worse, for instance, movement becomes more problematic or urinary incontinence is making everyday life more difficult or painful.
How is closed spinal dysphraism diagnosed?
Initial suspicions may be raised through clinical examination but imaging scans are used to confirm the extent of the problem. Ultrasound or magnetic resonance imaging scans are the usual methods used.
How is closed spinal dysphraism treated?
If there are clinical symptoms that are getting worse, these may be reduced using surgery to release the tethered cord. This relieves pressure on the spinal cord and nerves and can improve leg symptoms in many cases. It is less successful in improving bladder and bowel problems but usually stops them getting any worse over time.
What does the operation involve?
At surgery, the surgeon will release the spinal cord from where it is tethered so that it can move as the child grows. If possible, the surgeon will reduce the size of a lipoma to relieve pressure on the spinal cord. After the operation, the incision on your child’s back will be closed and covered with a dressing.
Are there any risks?
The operation to detach a tethered cord is very specialized due to the complex arrangements of nerves in the area. There is always a risk that the nerves, or the spinal cord itself, could be damaged in the operation but if the surgeon believes that this may happen, he or she will stop the procedure.
The aim of the operation is to stop your child’s symptoms from them getting any worse. There is no guarantee that this operation will remove your child’s symptoms or even improve them. This operation tends to improve leg symptoms more frequently than bladder and bowel symptoms.
What is the outlook for children with closed spinal dysphraism?
Orthopaedic problems
In some cases, children may have developed leg and foot problems as a result of the closed spinal dysphraism. These can include clawing of the toes or very high arches, which in turn can lead to tightening of the Achilles tendon at the heel. This can affect one leg or both and if it is severe, we may refer your child to an orthopaedic surgeon for further treatment.
Where a child has scoliosis as a result of the closed spinal dysphraism, further treatment by an orthopaedic spinal surgeon may be required. Sometimes however, treatment of the dysphraism may reduce or even improve the progression of the spine curvature.
Bladder and bowel control
The nerves that control bladder and bowel function are contained in the lower portion of the spinal cord and so can be affected by closed spinal dysphraism. The degree to which bladder and bowel control is affected depends on the severity of the defect.
Problems associated with the bladder are largely due to incomplete emptying, which is caused by the messages from the bladder not being transmitted to the brain well enough. Incomplete emptying of the bladder can lead to urinary tract infections (UTIs) and backflow of urine towards the kidneys (reflux), sometimes severe enough to damage the kidney. Signs of bladder problems include: urinary incontinence or dribbling, recurrent infections, bedwetting at night, needing to urinate frequently or having difficulties potty training. Bowel incontinence (soiling) is a less common problem, and rarely occurs if there are no bladder control problems. Early diagnosis and treatment can help reduce these problems but rarely solve them completely.
Movement
Closed spinal dysphraism can lead to muscle wastage on one side, affecting the buttocks and calf. This is caused by the muscles on one side being used more and therefore becoming stronger than the other, due to the stretching of the nerves leading away from the spinal cord when the cord is tethered. This can result in numbness, unbalanced walking, painless skin lesions, stiffness and pain in the lower limbs and back, sometimes relieved with odd postures or lying down. The physiotherapist will advise you about strengthening these muscles and improving their function as much as possible.
What about future pregnancies?
There is now evidence that an adequate intake of folic acid can dramatically reduce the risk of neural tube defects occurring in future pregnancies. If you are planning a further pregnancy, we recommend that you take 4mg of folic acid each day for at least three months before conception and for the first three months of pregnancy. This dose is higher than the standard recommendation for women who have not previously had a child with spina bifida. If you have any concerns about future pregnancies, please feel free to contact us.
What is a myelomeningocele?
In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
How is myelomeningocele treated?
Without the protective covering of skin, the spinal cord will become further damaged, spinal fluid often leaks from the area and there is a very high risk of infection. Surgery is usually recommended within the first few days of life. The aim of surgery at this stage is to put the spinal cord back into the spinal canal and repair the defect in the back so that the area is covered with normal, healthy skin.
The physiotherapist will see your child after the operation. He or she will assess how much strength your child has in each muscle group and measure his or her sense of feel. When taken together, muscle strength, sensation and reflexes give us a picture of how well the messages are getting from the brain to the arms and legs via the spinal cord. The physiotherapist will also give advice on how to position and handle your child to stretch out tight muscles and to help with normal development.
Once your baby is recovering well, you will both be able to go home. We will need you to come back to the hospital between 10 and 14 days after the operation so that we can check the operation site, carry out an ultrasound scan of your baby’s head and measure his or her head circumference. The child is followed up on a regular basis.
What problems can myelomeningocele cause?
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Bladder function
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Hydrocephalus
The circulation of cerebrospinal fluid (CSF) is often disturbed in children with myelomeningocele. Either at birth or in the days and weeks following surgery, fluid may start to build up within the brain. This is called hydrocephalus and can result in increased pressure in the brain. If this occurs, an operation to place a shunt tube to divert the excess fluid from the brain to the abdomen is needed. This operation is needed in about 60 per cent of children with myelomeningocele.
Mobility
Myelomeningocele affects each child differently, and how each child moves around will vary too. Some children will need splints or walking aids, and others may move around more easily in a wheelchair. Your doctor will speak to you about how your child’s condition will affect their mobility.
What is the outlook for children with myelomeningocele?
The outlook for children with myelomeningocele has improved dramatically in recent decades. Intellectual prognosis is very good for the majority of children, most of whom will go on to full time education. Recreational and employment opportunities are better now than at any time in the past. However, this is a multidisciplinary approach and team work with parental support is a must for a good outcome.
GUJARATI
બરડા પરની ગાંઠ
સ્પાઇના બાઇફીડા કરોડરજ્જુની જન્મજાત ખોડ છે જેમાં કરોડનાં મણકાં ખુલ્લા રહી જાય છે. આ કારણે કરોડરજ્જુની નસો અને તેનાં પરનાં આવરણો કરોડનાં મણકાંની બહાર આવે છે. આ ખોડ નવજાત બાળકનાં બરડા પર ગાંઠના રૂપમાં આવે છે. સામાન્ય રીતે આવી ગાંઠ કરોડનાં મણકાંના કોઈપણ ભાગ-ગરદન, છાતી, કમર અને કમરનાં નીચેના ભાગમાં હોઈ શકે છે.
કરોડરજ્જુ અને તેની નસોનો વિકાસ ખામીયુક્ત હોવાનાં કારણે બાળકનાં બંને પગ ઓછા યા વધુ પ્રમાણમાં લકવાગ્રસ્ત હોઈ શકે છે અને ઘણી વાર પેશાબ-સંડાસ કંટ્રોલ કરતાં સ્નાયુ પણ નબળાં હોય છે. સ્નાયુઓની આ ખામી બરડાંની ગાંઠનું આૅપરેશન કરવાથી પણ સારી નથી કરી શકાતી અને બાળકને તેની સાથે જીવતાં શીખવું પડે છે.
સ્પાઇનાં બાઇફીડાવાળા ૫૦% થી ૬૦% બાળકોને માથામાં પાણી ભરાવાની શક્યતા પણ રહે છે. જેને હાઈડ્રોકેફલસ કહે છે. આને શંટ આૅપરેશન દ્વારા સા૨ું કરી શકાય છે. •
HINDI
पीठ पर गांठ (न्यूरल ट्यूब में दोष)
स्पाइना बाईफीडा रीड की हड्डी का जन्मजात दोष है, जिसमें रीड़ की हड्डी के मनकें खुले रह जाते हैं। इससे रीड की हड्डी की नसें और उसका ऊपरी भाग रीड की हड्डी के मनकों से बाहर निकल आता है। यह दोष नवजात शिशु की पीठ पर एक गांठ के रूप में उभर कर दिखाई देता है। सामान्य रूप से यह गांठ रीड़ की हड्डी के मनकें के किसी भी हिस्से – गरदन, छाती, कमर और कमर के नीचले हिस्से में हो सकती है।
रीड की हड्डी और उसकी नसों का विकास दोषपूर्ण होने के कारण बच्चे के पैरों की मांसपेशियाँ कमजोर हो सकती है, जिससे उसके शरीर का थोड़ा या अधिक हिस्सा लकवा ग्रस्त होता है। मल-मूत्र पर भी उसका नियंत्रण नहीं रहता। इस प्रकार का न्यूरोलोजिकल दोष पीठ की गांठ के ऑपरेशन से भी ठीक नहीं किया जा सकता और बच्चे को इस रोग के साथ जीना सीखना पड़ता है।
स्पाईना बाईफीड़ा रोग से ग्रस्त ५०% से ६०% बच्चों के सिर में पानी का भराव होने की संभावना होती है, जिसे हाइड्रोकेफेलस कहते हैं। शंट ऑपरेशन से इसे ठीक किया जा सकता है। •