Anorectal Malformation
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is an anorectal anomaly?
This is a disorder affecting the anus and the rectum, the last part of the digestive system. After food has been digested it passes through the small bowel into the large bowel. The faeces (stools) are stored in the rectum until the muscles receive a message from the brain to empty the bowel. The faeces then pass out through the anus.
There are two types of anorectal anomaly – low anorectal anomaly and high anorectal anomaly. A low anorectal anomaly is where the anus is closed over, in a slightly different position or narrower than usual. A high anorectal anomaly is where the bowel has a closed end and does not connect with the anus or it connects with another part of the body through a passage called a fistula.
An anorectal anomaly can be associated with other problems, but the doctor will examine your child closely to check if this is the case.
What are the symptoms of an anorectal anomaly?
Symptoms vary according to the type of anorectal anomaly. They are classified into two types (high and low) depending on where the bowel ends.
If your child has a low anorectal anomaly, faeces cannot be removed from the body as usual, and so builds up in the bowel. Your child will not be able to pass meconium – the dark faeces passed in the first few days of life. The build up of faeces in the bowel can cause a swollen abdomen and vomiting.
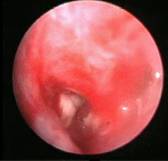
Low Anorectal Malformations
If your child has a high anorectal anomaly without a fistula, he or she will not be able to pass meconium and will develop similar symptoms.
Anorectal Malformation without fistula
If your child has a high anorectal anomaly with a fistula, the faeces will be able to pass out of the body, usually through the vagina in girls or through the urethra in boys.


Anorectal Malformation without fistula
How is an anorectal anomaly diagnosed?
An anorectal anomaly is usually diagnosed soon after birth, on examination, or when the baby fails to pass meconium. The doctor may suggest scans to give a clearer picture of the type of anorectal anomaly and whether there is a fistula.
What causes an anorectal anomaly and how common is it?
An anorectal anomaly happens when the bowel does not form properly while the baby is developing in the womb. We do not know exactly what caused this, but it was not due to anything that happened during pregnancy.
About one in 3,000 babies are born with an anorectal anomaly, with more boys than girls affected.
What treatments are available and are there any alternatives?
The treatment depends on the type of anorectal anomaly. All types of anorectal anomaly will need an operation under general anaesthetic – usually an ‘anoplasty’ if your child has a low anorectal anomaly or a series of operations if your child has a high anorectal anomaly.
The first operation is to create a loop stoma (an artificial way of disposing of waste matter) usually in the days after birth.
The second is a ‘pull-through’ operation to join the bowel to a newly created anus. This usually happens when your child is a few months old and has gained weight.
The final stage is to close up the stoma. This happens when your child’s bowel and anus is working well a few weeks after the second operation. The three operations are usually completed by the time your child is six months old. There are no alternatives to these operations, as your child needs to be able to pass faeces to prevent it building up in the bowel, which could lead to discomfort and infection.
What does the operation involve?
Anoplasty – the surgeon will open up the anus (if it was closed over), move the anus (if it was in a slightly different place to usual) or widen the anus (if it was narrower than usual).
Creation of loop stoma – the surgeon will bring the bowel to an artificial opening in your child’s abdomen (stoma).
‘Pull-through’ operation – the surgeon will create a new anus and then separate the bowel from the fistula (if there is one) and bring it down to join the newly created anus. He or she will then close up the fistula. Your child will continue to use the stoma so that the bowel and anus can rest and heal.
Closure of loop stoma – the surgeon will disconnect the the bowel from the stoma and close it to form a fully working bowel.
What happens afterwards?
Your child will come back to the ward to recover. We will keep your child as comfortable as possible, by giving regular pain relieving medications. For the first few days, the pain relief will usually be given through a ‘drip’ and then, when your child is more comfortable, in the form of medicines to be swallowed.
For the first few days, your child will need a ‘drip’ of fluids until he or she feels like eating and drinking again. This will also allow the bowel to rest and start to heal. After a while, you can start to feed your child again, starting with small amounts, and increasing the amount as he or she tolerates it.
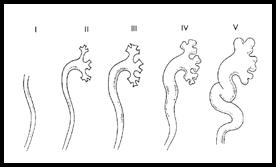
If your child has had a new anus created, you may be asked to stretch (dilate) it using a probe called a dilator. The doctor will show you how to do this before you go home. You will need to start with a small size dilator and gradually increase the size until the anus is the right size
If your child has had the stoma and mucous fistula created, the nurses will teach you how to look after them both. We will make sure you feel confident before you go home.
What is the outlook for children with anorectal anomaly?
The outlook for children with anorectal anomaly depends on the type of abnormality. Your child may need extra bowel training at a later stage to learn when and how to empty his or her bowels. He or she may also need some extra help in the form of enemas or washouts, but these will be explained to you if they are needed. However, some children continue to have bowel problems for many years after the operations, but this depends on the original severity of the anorectal anomaly.
Your child will need regular check ups with your doctor at the hospital. These happen regularly until your child is a teenager.
Some girls who have had an anorectal anomaly may be better having a caesarean section rather than normal childbirth. This will put less strain on the operation site and is less likely to cause problems in the future.
Publications on the subject : M.R.I. in A.R.M.
GUJARATI
સંડાસની જગ્યા ન હોવી – મળમાર્ગ ન હોવો
દર ૩૦૦૦ એ એક બાળક આ ખોડ સાથે જન્મ લેતું હોય છે. છોકરાંઓમાં આ ખોડ વધુ જાવામાં આવતી હોય છે. આ ખોડ થવાનું કોઈ ચોક્કસ કારણ જાણી શકાયું નથી અને તે ડિલિવરી પહેલાં માતાની સોનોગ્રાફી દ્વારા જાણી શકાતી નથી. આ ખોડ બે પ્રકારની હોય છે. ૧. હાઈ ૨. લો.
૧) ‘હાઈ’ વેરાઈટી : આ ખોડમાં બાળકનાં મળમાર્ગનું આંતરડું પેશાબના રસ્તા સાથે અને બેબીમાં યોનિમાર્ગ સાથે જાડાયેલું હોય છે. આ કેસમાં બાળકને જન્મ પછી તરત આૅપરેશન કરી પેટ પર મળ માટે ટેમ્પરરી રસ્તો કરવો પડે છે. આને કોલોસ્ટોમી કહેવાય છે. બાળક ૩-૫ માસનું થાય ત્યારે પેશાબ સાથેનું કનેક્શન દૂર કરી મળમાર્ગ યોગ્ય જગ્યાએ બનાવવાનું ઓપરેશન કરવામાં આવે છે. ત્યાર બાદ કોલોસ્ટોમીને બંધ કરી દેવામાં આવે છે. સીલેક્ટેડ કેસમાં આ ત્રણેય આૅપરેશન એક જ સ્ટેજમાં કરી શકાય છે.
૨) ‘લો’ વેરાઈટી : આ કેસમાં આંતરડાને પેશાબનાં રસ્તા સાથે કોઈ જાડાણ હોતું નથી. આ કેસમાં પેટે કોલોસ્ટોમી કરવાની જરૂર પડતી નથી અને એક જ આૅપરેશન દ્વારા બાળક સાજું થઈ જતું હોય છે. આ ખોડ સાથે બીજી ખોડ-ખાપણ નથી તે જાણવા માટે એક્ષરે, સોનોગ્રાફી અને ઈકોકાર્ડીયોગ્રાફીની તપાસ થાય છે.
સચોટ આૅપરેશન અને યોગ્ય કાળજી મળે તો આ બાળકો બીજા બાળકોની જેમ નોર્મલ જીવન જીવી શકે છે. •
HINDI
मल मार्ग का न होना
हर ३००० बच्चों में एक बच्चा इस विसंगति के साथ जन्म लेता है। प्रसूति से पूर्व सोनोग्ा्राफी के द्वारा भी इसका पता लगाना कठीन होता है। यह विसंगति दो प्रकार की होती है। (१) ‘लो’ (कम) विसंगति, (२) ‘हाई’ (उच्च) विसंगति।
‘लो’ (कम) प्रकार ः गुदा मार्ग अपने निर्धारित आकार या उचित स्थान पर स्थित नहीं होता है अथवा गुदा मार्ग पूर्णरूप से बंद होता है।
‘हाई’ (उच्च) प्रकार ः गुदा मार्ग पूर्णरूप से बंद होता है और वह शरीर के अन्य अंग के साथ एक मार्ग के द्वारा जुड़ा होता है जिसे फिस्च्युला कहा जाता है।
इसका पता जन्म के तुरंत बाद जांच के उपरांत अथवा जब बच्चा अपना प्रथम मलत्याग नहीं कर पाता तब चलता है। बच्चे में इस प्रकार की विसंगति के साथ किसी अन्य प्रकार की विसंगति तो नहीं है इसकी पुष्टि करने के लिए एक्स-रे, सोनोग्ा्राफी और इकोकार्डियोग्ा्राफी द्वारा जांच की आवश्यकता होती है।
‘लो’ विसंगतिः ऐसे में गुदासंधान (एनोप्लास्टी) की आवश्यकता होती है।
‘हाई’ विसंगतिः इसमें बच्चे पर त्रि-स्तरीय सर्जरी की आवश्यकता होती है। कुछ चुनिंदा मामलों में केवल एक-स्तरीय ऑपरेशन भी किया जा सकता है।
गुदा एवं मलाशय संबंधी विसंगति के संबंध में बच्चे का दृष्टिकोण विसंगति के प्रकार और उसकी तीव्रता पर निर्भर करता है। बाद में, बच्चे को अपने पेट को कब और कैसे साफ करना चाहिए इस बात के प्रशिक्षण की आवश्यकता हो सकती है। उसे अपने पेट को साफ करने के लिए जुलाब दिए जाने की आवश्यकता भी हो सकती है। यह विसंगति वाली लड़कियों में सामान्य प्रसूति के बजाय सीजेरियन सेक्शन अधिक उपयुक्त होता है। इससे उनके ऑपरेशन के स्थान पर कम तनाव पड़ेगा और भविष्य में किसी प्रकार की समस्या होने की संभावना कम होती है।•
After An Operation
My child is complaining of pain. What can I do?
It is quite normal for your child to feel some discomfort for the first 48 hours after his or her operation. Usually medicines are given to relieve any pain. If stronger medications are needed they would be given either intravenously by the nurses.
Pain relief medicines will be given at the time of discharge. If, when you get home, you feel that your child needs more powerful pain relief, you should call your doctor. You can also telephone the hospital for advice.
Always follow the instructions that have been given to you. Never give your child more than the recommended dose.
Is there anything else I can do to make my child feel better?
If the skin is sore about the site of the operation, wearing loose-fitting clothes will make your child feel more comfortable. As well as giving pain relief medicines, distracting your child by playing games, watching TV or reading together can also help to keep your child’s mind off the pain.
My child does not want to eat. Should I be worried?
After the anesthetic, your child may feel sick for 24 hours. You should encourage your child to drink but do not force him or her to do so. As long as your child is drinking, it does not matter if he or she does not feel like eating for the first couple of days.
Are there any activities my child should avoid?
You should keep your child away from school or nursery for a week after the operation. After certain types of operation, your child should not ride a bicycle or play contact sports for about a week to ten days. Doctors will give you relevant instructions regarding the same according to the type of operation your child had at the time of discharge.
Antegrade Continence Enema (ACE)
What are bowel washouts and why does my child need them?
Bowel washouts are a method of dealing with constipation or with soiling, which is the leakage of faeces (stools) other than during a bowel movement. There are many reasons why a child may soil including:
- Congenital (present at birth) abnormalities affecting the anus and rectum
- Neuropathies (nerve supply problems) as a result of spinal abnormalities like spina bifida.
- Overflow incontinence which is often seen in children with severe constipation.
- Other methods will usually be tried first, and may include bowel training, dietary changes, medications taken by mouth, and medications taken rectally (enemas or suppositories). If these methods fail, doctors may recommend bowel washouts using an antegrade colonic enema (ACE). This can also be called the Malone or MACE method.
What do they involve?
Before you can start doing bowel washouts, your child will need an operation under general anaesthetic. This operation creates a channel (usually using the appendix) into the large bowel at a point called the caecum. The fluid used to wash out the bowel can then be inserted easily. This fluid flushes the faeces out through the rectum in the usual way.
What does the operation involve?
ACE operations are carried out using keyhole surgery (laparoscopy) or open surgery. Depending on the surgical method used, the surgeon may disconnect the appendix from the caecum and then reconnect it. Alternatively, he may leave the appendix in its original position and bring the end up to the wall of the tummy. In both methods, the end of the appendix is opened up to form a channel from the tummy wall to your child’s large bowel. This is called a stoma (artificial opening).
If your child has already had his or her appendix removed or if it is not suitable, the surgeon may need to use a piece of the small bowel to create the passage.
Are there any risks?
All treatments carry an element of risk, but this must be balanced against the quality of life without treatment.
What happens afterwards?
Your child will come back to the ward to recover. For the first day or two, he or she will have a drip giving fluids and medication until the bowel starts to recover. The drip will be removed when your child starts eating and drinking again.
The surgeon will have inserted a catheter (thin, plastic tube) into the stoma to keep it open. This should stay in place for seven to fourteen days after the operation. In some cases, the catheter may need to stay in place for longer. This varies from child to child.
When your child has recovered from the operation, and eating and drinking again, the nurse will teach you how to do bowel washouts using the ACE. When you are confident, you and your child will be able to return home.
Looking after the stoma
You should insert a catheter into the stoma each day to keep it open, even if no washout is planned for that day. We will give you two sizes of catheter, the size you will be using to do the washout and one a size smaller. Alternatively, you can insert the small silicone plug into the stoma.
The stoma can shrink a little after the operation, but this usually settles down when you use the catheter. On rare occasions, the stoma may need stretching while your child is under a general anesthetic.
Starting washouts
Nurses will teach you how to do the bowel washouts when the stoma has settled down, usually between two and three days after the operation. If you and your child have returned home, you will need to come back to the hospital for teaching. You will have a lot to learn about bowel washouts and it may feel daunting at first, but will quickly become easier.
The washout solution varies from child to child, depending on his or her needs. The amount of fluid also varies and is worked out according to your child’s age and size. For the first few weeks, the make-up of the solution may need changing to get the best result.
It may take about six to eight weeks to get into a routine and for the washouts to work effectively. It can help to keep a daily diary of progress. You will also need to keep in contact with your doctor for the first few months until you and your child have settled into a regular washout pattern.
Accessory Digit / Additional Finger
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
The condition of having an additional little finger on one or both hands is very common, especially in certain ethnic groups.
Usually it is inherited, with a 50 per cent or one in two chance of it happening if the parents have it.
At other times, it happens spontaneously, without anyone else in the family being previously affected.
When your child has an additional little finger, there is a 50 per cent or one in two chance of his or her children also being born with one.
Can it cause any problems?
Sometimes the extra finger is well formed, but more commonly it has a narrow base or stalk and is dangling from the edge of the normal hand or leg. The place where the extra finger joins the hand might be bony or it could just be a soft stalk.
If the extra finger has a narrow stalk, it can twist, cutting off the blood supply so it turns blue or black. The extra finger has a nerve supply so it will be painful if this happens.
How can the extra little finger be corrected?
The extra little finger(s) can be removed in a short operation.
Are there any risks?
It is a relatively safe procedure with no major complications.
There will be a scar where the extra finger was removed, but this is quite small. It usually fades gradually with time, so that it is less noticeable but it will always be there.
What would happen if my child did not have the operation?
The extra little finger should not cause any problems if it is taped securely to the next finger. However, most parents ask for the extra finger to be removed, as it can lead to unwanted attention for their child as they grow older.
What does the operation involve?
Once the anaesthetic has started to work, the surgeon will remove the extra finger, stopping its blood supply. He will stitch the operation site closed and cover it with a dressing. The operation lasts around 15- 20 minutes to remove one extra finger and slightly longer if an extra finger needs to be removed from both hands.
When you get home
Keep the operation site dry and covered with the light dressing for one week.
All the stitches used are dissolvable and will begin to rub off in around two weeks. The light dressing can be gently peeled off after a week or so.
After two weeks, if the operation site has healed, you can massage the scar with coconut oil/ antiseptic ointment twice a day until the scar has faded.
GUJARATI
બાળકની આંગળીઓની ખોડ
બાળકનાં હાથ અને પગની આંગળીઓમાં ઘણી ખોડ જાવા મળે છે. જા એક-બે આંગળીઓની ખોડ હોય તો સર્જરીનાં રીઝલ્ટ સારા આવે છે પણ ઘણી વખત હાથ કે પગની આંગળીઓની સાથે તેમાં રહેલાં હાડકાં પણ ખોડ વાળા હોય તો બાળક આ ખોડ સાથે સારું કામ કરી શકે તેવી સર્જરી કરવામાં આવે છે. આમાં સંપૂર્ણ નોર્મલ દેખાય તેવાં હાથ નથી કરી શકાતા.
આ ખોડ ૧ ૧/૨ વર્ષની આસપાસ આૅપરેશન દ્વારા છૂટી કરી શકાય છે.
હાથ કે પગમાં પાંચ આંગળીઓ કરતાં વધુ હોય તો તેને પોલીડેક્ટલી કહેવામાં આવે છે. સામાન્ય રીતે એક્સ્ટ્રા આંગળીઓ કાઢવાની સર્જરી ૧ વર્ષ પછી કરાવવી, પણ જા એક્સ્ટ્રા આંગળી ફક્ત ચામડીથી જાડાયેલી હોય અને તેમાં વળ ખાઈ ગેંગરીન થાય છે તો તે માટે તાત્કાલિક આૅપરેશન કરાવવું પડે છે. •
HINDI
बच्चों की अंगुलियों की विसंगति
सींडेक्टली अर्थात ‘जुड़ी हुई अंगुलियाँ’ वह स्थिति है जब बच्चे के विकास के दौरान दो या दो से अधिक अंगुलिया पूरी तरह से अलग नहीं हो पाती है। कभी-कभी कुछ बच्चे बिना किसी उपचार के भी कार्य कर सकते है। पैर के अंगूठे के सिंडेक्टिली का उपचार आमतौर पर कार्यात्मक कारणों से अधिक कॉस्मेटिक कारणों से किया जाता है (ताकि बच्चा चप्पल/स्लीपर पहन सके)। सर्जरी के लिए कभी-कभी त्वचा निरोपन की आवश्यकता पड़ती है।
पॉलीडेक्टीलीमें बच्चे को अतिरिक्त अंगुलियाँ अथवा अंगूठे होते हैं। यह एक या दोनों हाथ अथवा पांव में हो सकती है। अधिकतर मामलों में ये अतिरिक्त अंगुलियाँ छोटे से डंठल पर नर्म मांस-तंतु के समान होती हैं। कभी-कभी इनमें बिना किसी जोड़ के हड्डी होती है; और यह शायद ही कभी पूर्णतया कार्यशील अंगुली के रूप में होती है। सींडेक्टली के लिए सर्जरी १भ वर्ष की आयु होने पर की जाती है। अतिरिक्त अंगुली केवल त्वचा से जुड़ी हो और इसमें मरोड़ उत्पन्न हो जाए तो यह एक आपात स्थिति पैदा कर सकती है। •
Anal Fissure
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Anal fissures are tiny tears in the skin around the anus and can be painful. They usually develop as a side effect of constipation. Constipation is the condition where a person passes stools less frequently than usual and the stool is harder, drier and painful to pass.
What causes anal fissures?
They usually develop when your child is constipated. The sphincter (ring of muscle) around the anus stretches to let the hard dry stool pass, and the tissue around the anus may tear as a result.
What are the signs and symptoms of anal fissures?
Anal fissures are usually small but can be painful, as the tissue around the anus is supplied with lots of nerve endings. The tears can bleed bright red blood, which will show while washing or on the toilet paper but soon stops. After passing stools, they start to heal but can re-open the next time. They usually heal completely in a week or two, but only after the stool has softened.
How are anal fissures diagnosed?
Initially, the doctor will diagnose constipation from your child’s history. They may look at your child’s anus to see if any anal fissures are visible. Occasionally, the doctors may suggest your child has an examination under anesthetic, to check the anus more closely and confirm that it is otherwise normal.
How are anal fissures treated?
Treatment aims to reduce the constipation, so that stool is easier to pass and the tissues around the anus are less likely to tear. This may involve a change in diet to include higher fiber foods, medicines to soften the stool so it is less painful to pass, and laxatives to stimulate passing stool.
As well as reducing constipation, there are various options for making the anal fissures less painful until they heal. A warm bath can soothe the area for a while, but it should be patted dry rather than rubbed. Creams or ointments can be soothing, but certain ones containing steroids or anesthetics should only be used for a few days at a time.
What happens next?
Children who have developed anal fissures once are likely to develop them again. The key to preventing anal fissures is to avoid becoming constipated. Try to make sure your child to has a balanced diet containing plenty of fiber and encourage them to drink plenty of fluids.
GUJARATI
કબજિયાત
કઠણ ઝાડો થવો અને તે કરવામાં બાળક ને દુઃખાવો થાય પેટ ફૂલી જાય, વધુ પડતો ગેસ થાય તો અચુક ડાક્ટરની સલાહ મુજબ તપાસ કરાવવી અને દવા લેવી. ઘરગથ્થુ દવાઓ ન કરવી. ઝાડો દરરોજ ન થતો હોય, પણ બાળક પોચો સંડાસ ૨-૩ દિવસે કરે તો તેને કબજિયાત ન ગણવી.
કબજિયાત લગભગ જન્મથી હોય અને બાળકનું પેટ ફૂલે, વારંવાર એનીમા અપાવવા પડે અને બાળકનું વજન ન વધે તો ચોક્કસ આ મોટા આંતરડાની જન્મજાત બીમારી હોઈ શકે. આને હર્ષસ્પૃન્ગ ડીઝીઝ કહે છે. આ માટે બાળકના સર્જનને બતાવી બાળકની વધુ તપાસ જેમ કે બેરિયમ એનીમા અથવા રેક્ટલ બાયપસી કરાવવી પડે છે. •
HINDI
कब्ज
मल सख्त हो और उसे करने में बच्चे को दर्द हो, पेट फूल जाए, अत्यधिक गैस हो जाए तो डॉक्टर से अवश्य परामर्श करें और निर्देश के अनुसार जाँच कराएं और दवाइयां लेनी चाहिए। घरेलू दवाइयाँ नहीं लेनी चाहिए। मल हर रोज न होता हो, लेकिन बच्चा भले ही २-३ दिन में नरम संडास करे तो इसे कब्ज नहीं समझा जाना चाहिए। कब्ज जन्म से हो और बच्चे का पेट फूल जाए, बार-बार जुलाब देने की आवश्यकता पड़ती हो, और बच्चे का वजन न बढ़ रहा हो तो निसंदेह यह बड़ी आंत सम्बंधी जन्मजात बीमारी हो सकती है। इसे हर्षस्प्रंग रोग कहते हैं। बच्चे को सर्जन के पास ले जा कर अधिक जांच करानी पड़ती है जैसाकि बेरीयम एनिमा अथवा रेक्टल बायोप्सी।•
Abdominal Wall Defects (Exomphalos)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Exomphalos is a type of abdominal wall defect. It occurs when a child’s abdomen does not develop fully while in the womb.
Early in all pregnancies, the intestine develops inside the umbilical cord and then usually moves inside the abdomen a few weeks later. In exomphalos, the intestines and sometimes other organs such as the liver, remain inside the umbilical cord but outside the abdomen.
What causes exomphalos?
We do not know what causes exomphalos. It affects two in every 5,000 children born each year. Exomphalos can be associated with other problems, but the doctors will examine your child closely to check if this is the case.
What are the signs and symptoms of exomphalos?
Exomphalos is immediately recognizable because the child’s intestines are outside the body and covered in a membrane. The size of the bulging membrane containing the intestines and other organs varies from a small protrusion to quite a large lump.
There are two types of exompahlos:
Exomphalos minor where the opening is less than 4cm and only containing the intestine, and Exomphalos major where the opening is greater than 4cm and/or with the liver inside the cord.
How is exomphalos diagnosed?
In many cases, exomphalos is visible on pre-natal ultrasound scanning, which is useful because it gives time for discussions and planning for when and where to give birth.
How is exomphalos treated?
Exomphalos is a serious condition so needs prompt treatment soon after birth.
Depending on the size of the exomphalos, your child may need to have it repaired in one operation or in several stages. If the exomphalos is small and the child is stable, they may have an operation soon after admission to the hospital, where the surgeon replaces the contents back inside the abdomen and closes up the base of the umbilical cord.
If the exomphalos is larger, contains the liver and/or your child needs to be stabilised, doctors may place a silo or pouch over the intestines, which is closed over a period of days to weeks, to allow your child to grow so that there is room inside the abdomen.
What does the operation involve?
If your child is having a one-stage repair under general anaesthetic, the surgeons will replace your child’s entire intestine into the abdominal space and close up the hole at the base of the umbilical cord.
Sometimes, they may need to use a ‘patch’ of material if the hole is quite large. They will cover the area with a dressing to protect the wound while it heals.
In a staged repair, there is too much intestine outside of the abdomen to put back without causing further damage or the space inside the abdomen is too tight. While your child is under general anaesthetic, the surgeon will make a mesh sac and put it over the intestine which keeps it contained and protected.
This sac is then suspended above your child so that gravity gradually moves the intestines back inside the abdomen. It is tightened regularly until all the intestine is inside the abdomen, which usually takes a few days to a few weeks. Your child will then have an operation under general anaesthetic to close up the skin and muscles.
Are there any risks with the operation?
All surgery carries a small risk of bleeding during or after the operation. During the operation, the surgeon will minimise any bleeding by sealing off the blood vessels affected. There is a very small chance that nearby structures in the abdomen could be damaged during surgery but this is a very rare occurrence.
Every anaesthetic carries a risk of complications, but this is very small. Your child’s anaesthetist is a very experienced doctor who is trained to deal with any complications.
It can take a while after the operation for the intestine to start working properly so your child may need to be fed intravenously using total parenteral nutrition (TPN) for a while. Some babies with exomphalos have breathing problems which may require more support for a longer period.
Are there any alternatives to the operation?
In some scenarios, the child may be treated with particular chemicals / ointments in order to make the membrane covering the intestine hard. The surgery may hence be delayed by a few weeks. Ultimately, the condition needs to be treated to allow your child to grow and develop.
What happens after the operation?
Your baby will come back to recover either in the intensive care unit .All babies are closely monitored after the operation, and so your baby will be connected to monitors to check their breathing, heart rate and oxygen levels. If your child needs help with breathing, they will be connected to a ventilator. They will also be given pain relief through the intravenous infusion (drip).
What happens next?
The outlook for children born with exomphalos varies depending on the size of the defect and any other problems. Many children have grown up to live normal lives.
Children who have had aexomphalos repair may develop hernias in the years after the operation. This is because the abdomen has fewer muscles than usual.
GUJARATI
એક્ઝોમ્ફેલોસ
એક્ઝોમ્ફેલોસ ૫૦૦૦ એ ફક્ત ૨ બાળકોમાં જાવા મળતી એક ગંભીર જન્મજાત ખોડ છે.
સામાન્ય રીતે ગર્ભમાંના બાળકનાં આંતરડા તેના પેટની બહાર આકાર લઈને નાળના માર્ગેથી પેટની અંદર જતાં હોય છે. આ ખોડમાં બાળકના પેટની દીવાલ બરાબર ન બનતા તેના આંતરડા અને કોઈક વખતે બાળકનું લીવર પેટની બહાર નાળની અંદર ફસાયેલા રહેતા હોય છે.
આ ખોડ બાળકને જાતાં જ ખબર પડી જાય છે. બાળકના આંતરડા પેટની બહાર પારદર્શક પડથી ઢંકાયેલા દેખાય છે. બાળકને તાત્કાલિક સારવારની જરૂર પડે છે. સારવાર અર્થે મોકલતા પહેલાં બાળકનાં આંતરડાને ચોખ્ખા સલાઈનવાળા કાપડથી ઢાંકી દેવું જાઈએ. આ બાળકોમાં ઓપરેશનની જરૂર પડતી હોય છે. આૅપરેશન એક સ્ટેજ અથવા બે સ્ટેજમાં કરવામાં આવે છે. જા બાળક આૅપરેશન ખમી શકવાની Âસ્થતિમાં ન હોય તો અમુક કેમિકલ/દવાઓ લગાવી આંતરડાના ઉપરના પડને કડક કરવામાં આવે છે જેથી બાળકને ઇન્ફેક્શન ન લાગે. આ બાદ યોગ્ય સમયે આૅપરેશન કરી પેટની દીવાલ બનાવવામાં આવે છે. •
HINDI
एक्जोमफेलस (नाभि सम्बंधी जन्मनात हर्निया)
एक्ज़ोमफेलस पेट की दीवार का एक दोष है। हर ५००० में २ बच्चों को यह प्रभावित करता है। गर्भाधान के कुछ ही सप्ताह बाद, गर्भनाल के भीतर आंतों का विकास होता है। एक्ज़ोमफेलस में आंतें और कभी-कभी अन्य अंग जैसाकि जीगर गर्भनाल के भीतर परंतु उदर के बाहर रह जाते हैं। एक्ज़ोमफेलस के बारे में तुरंत पता लग जाता है क्योंकि बच्चे की आंते शरीर के बाहर होती है और इनपर एक आवरण होता है। जन्म से पहले ही अल्ट्रासाउंड के द्वारा एक्ज़ोमफेलस का पता चल जाता है। एक्ज़ोमफेलस एक गंभीर परिस्थिति है और जन्म के तुरंत बाद इसका उपचार किया जाना आवश्यक होता है।
प्रसूति करानेवाले फिजीशीयन को सावधानीपूर्वक इन्हें (आंतो को) पानी में भीगोए जंतुरहित कपड़े से ढंक देना चाहिए और बच्चे को बालविशेषज्ञ के पास स्थानांतरित करना चाहिए।
एक्ज़ोमफेलस के आकार के आधार पर, एक ऑपरेशन अथवा अनेक स्तरीय ऑपरेशन के द्वारा इसे ठीक करने की आवश्यकता हो सकती है। यदि एक्ज़ोमफेलस अधिक बड़ा है, उसमें जीगर शामिल है और/अथवा बच्चे को स्थायीकरण की आवश्यकता हो, तो सर्जन को आंतों के ऊपर कुशूल अथवा थैली रख देनी चाहिए, ताकि बच्चा बढ़ सके और उदर के भीतर अधिक जगह बन सके। कुछ मामलों में, उपचार विशेष रसायनों/मलमों के द्वारा किया जाना चाहिए जिससे कि आंतों के ऊपर का आवरण सख्त हो जाए। तदनुसार, सर्जरी को कुछ हफ्तों के लिए विलम्बित किया जाना चाहिए। एक्ज़ोमफेलस के साथ जन्मे बच्चे का दृष्टिकोण विसंगति के आकर और अन्य समस्याओं के अनुसार भिन्न हो सकता है। कई बच्चे बड़े होकर सामान्य जीवन व्यतीत करते हैं। •
Atresia of Small bowel
The intestines form early in pregnancy as a long straight tube. Before the tenth week of pregnancy, they develop into the separate organs making up the digestive system. Occasionally, the intestines are not completely connected or blocked (atresia). Sometimes there is a partial blockage (web) inside the intestine.
Any part of the intestines can be affected by atresia or stenosis. Duodenal Atresia is one type. This occurs in around one in 6,000 births where the duodenum is closed off rather than being a tube. If the jejunum or ileum are affected, this is called ‘small bowel atresia’.
Small bowel atresia is more common than duodenal atresia. We do not know how exactly how many babies are born with small bowel atresia each year but we do know that it affects boys and girls equally. It is more common in twins or multiple births and babies born prematurely or with low birthweight.
Colonic atresia, affecting the large bowel, is very rare.
Small bowel atresia affects two areas of the small bowel – the jejunum and the ileum. The jejunum is the section of small bowel after the duodenum and is where the majority of nutrients are absorbed. The ileum is the main part of the small bowel, making up over half of its entire length, and connects to the large bowel. The blockage can affect any part of the ileum or jejunum.
What causes small bowel atresia?
More research is needed into the causes of small bowel atresia but currently doctors think that it is caused by reduced blood supply to sections of the bowel as the baby is developing in the womb. It is unlikely that it is caused by anything you did or did not do during pregnancy.
What are the signs and symptoms of small bowel atresia?
Many babies born with small bowel atresia appear well at birth but when they start to feed, they start to have nausea and vomiting and their vomit may be green. Their abdomen may appear swollen but soft and their skin may develop a yellow tinge (jaundice).
All newborn babies have meconium in their bowel. This is the dark green stool passed in the first day of life. Babies born with small bowel atresia may not pass any meconium at all or only a small amount. Not passing meconium does not prove that a baby has small bowel atresia but it may suggest it. Some babies with small bowel atresia pass meconium as expected.
How is small bowel atresia diagnosed?
When a baby with small bowel atresia is developing in the womb, they are may be surrounded by much more amniotic fluid than usual (polyhydramnios). Small bowel atresia can sometimes be suggested during pregnancy using an ultrasound scan.
After the baby is born, small bowel atresia is usually diagnosed when there are signs of an obstruction, such as vomiting, green bile and a swollen abdomen. An x-ray scan may show a blockage. Occasionally, doctors may suggest using a contrast scan and/or enema instead or as well as an x-ray.
Contrast scans and enemas use a thick, white liquid called barium or a clear liquid (contrast), both of which show up well on x-rays. The contrast cannot pass through the atresia suggests that atresia can be a cause.
How can small bowel atresia be treated?
Small bowel atresia is repaired in an operation under general anaesthetic. The operation to repair the atresia can is usually carried out using open surgery. Sometimes a laparoscopic surgery (key hole procedure) may help diagnose the problem so that it can be repaired using open surgery.
Are there any alternatives?
No. Small bowel atresia always requires surgical treatment to allow your baby to feed.
What happens before the operation?
Your baby will be transferred to the hospital soon after birth.
If your child is dehydrated, they will need a ‘drip’ of fluids for a while before the operation. Your child will also need a nasogastric tube, which is passed up the nose, down the foodpipe and into the stomach. This will drain off the stomach and bowel contents and ‘vent’ any air that has built up, which will make your child more comfortable.
When your child is stable, the surgeon will explain about the operation in more detail. Sometimes the atresia is suspected but may not be the only possible cause of the blockage. The surgeon will explain this to you.
What does the operation involve?
The surgeon will look at the bowel to determine the level of the blockage. If it is an atresia, this section is removed and the cut ends are joined together (anastomosis). This provides a clear passage for food and fluid to travel through your child’s intestine. The remainder of the small intestine will be checked for further atresias and treated if identified.
If it is not possible or safe to join the two ends together during the same procedure, the surgeon may bring the end of the intestine to an artificial opening (stoma) in the abdomen to form an ileostomy.
Are there any risks?
All surgery carries a small risk of bleeding during or after the operation. There is a chance that the area where the two ends of bowel were joined could start to leak, allowing bowel contents to escape into the abdomen. This is usually treated with antibiotics, but a second operation may be needed to check the leaking portion.
All abdominal surgery carries the risk of strictures forming. These are areas of scar tissue that can narrow the intestines, leading to obstruction. If your child vomits green bile and has a swollen abdomen, they should be reviewed urgently by a doctor.
It can take a while after the operation for the bowel to start working properly so your child may need to be fed intravenously using total parenteral nutrition (TPN) for a while. This affects many children.
What happens after the operation?
While your child’s intestines recover and start to work, they may be fed through a tube into their veins (total parenteral nutrition or TPN). This will gradually be replaced by breast or bottled milk, given through the naso-gastric tube when your child is able to tolerate this. As your baby recovers, you will be able to feed them from the breast or bottle. Over time, the drips and monitors will be removed one by one.Most children stay in hospital for one to two weeks, but occasionally a longer stay is needed.
What happens next?
The outlook depends on the amount of damage to the bowel. Adhesions can form after any abdominal surgery and can cause further problems such as blockage or pain. This however is quite rare and may sometimes require another operation to separate the adhesions.
Adenoids and Tonsils
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
The tonsils are areas of tissue on both sides of the throat, at the back of the mouth. Your child’s tonsils help them to build up immunity and fight infection. In many children, the tonsils become repeatedly infected with bacteria and viruses, which make them swell and become painful. This is called tonsillitis.
What causes tonsillitis?
Tonsillitis is the word used when the tonsils are infected so swell and become painful. Both bacteria and viruses can cause an infection – these are usually picked up as part of everyday life so there is little you can do to prevent them although good hygiene including hand washing is important.
What are the signs and symptoms of tonsillitis?
The main symptom of tonsillitis is a sore throat, which is particularly painful when swallowing. Your child may complain of earache as well.
The tonsils may also have a white covering or spots, which are a sign that the body is fighting off the infection. Your child’s neck may look a little swollen as well, and they may have a temperature.
How is tonsillitis diagnosed?
Tonsillitis can be diagnosed by looking closely in the mouth, sometimes using a small torch to look at the back of the mouth.
How is tonsillitis treated?
Pain relief medicines, such as paracetamol and ibuprofen can help reduce the pain and also bring down a temperature. If the infection was caused by a bacteria, the child will require antibiotics. Most cases of tonsillitis disappear within a few days.
If your child has repeated bouts of tonsillitis, we may suggest an operation to remove the tonsils.
SURGERY FOR TONSILLS AND ADENOIDS
The tonsils and adenoids are areas of tissue at the back of the throat. The tonsils are on both sides of the throat, at the back of the mouth, and are clearly visible. Adenoids are not visible, as they are high in the throat behind the nose.
Your child’s tonsils and adenoids help him or her to build up immunity and fight infection. Adenoids and tonsils seem to grow during childhood and then shrink around the age of four. By the time your child reaches adulthood, his or her adenoids and tonsils will have disappeared almost completely. This is because they are no longer needed, as your child’s body will have other defence mechanisms to fight against infection.
Why do tonsils have to be removed?
In many children, the tonsils become repeatedly infected with bacteria and viruses, which make them swell and become painful. Removing your child’s tonsils and adenoids will solve these problems.
Your child may have larger than average tonsils and adenoids, which partially block his or her airway. This can make it difficult for them to breathe through their nose. As a result, your child may breathe through their mouth and snore loudly when asleep. This can lead to a condition called sleep apnoea, where your child stops breathing for a couple of seconds while asleep and then starts again. This can severely disturb their sleep.
There is also a link between large tonsils and adenoids and a condition called glue ear. This happens when the middle ear becomes blocked by a sticky substance which affects your child’s hearing.
What are the risks of this operation?
Every operation carries some risk of infection but we will often give your child antibiotics as a precaution.
The risk of bleeding is usually greatest in the first few days after this operation. It is rarely serious.
Are there any alternatives to this operation?
If your child is having difficulties in breathing or has developed glue ear, it is probably better to have his or her tonsils and adenoids removed.
When your child gets home
Your child will probably feel uncomfortable for a week after the operation and may find swallowing difficult. They may also be reluctant to eat certain foods or brush their teeth.
GUJARATI
ટોન્સીલ :
ગળામાં જીભની પાછળ ડાબી અને જમણી બાજુ ટોન્સીલ(કાકડાં) આવેલાં હોય છે. બાળકોમાં ટોન્સીલનું ઇન્ફેક્શન સામાન્ય છે અને યોગ્ય એÂન્ટબાયોટીકથી મટાડી શકાય છે. વારંવાર ટોન્સીલમાં ઇન્ફેક્શનથી બાળકોની તંદુરસ્તી જાખમાતી હોય તો આૅપરેશન કરવાવું જરૂરી થાય છે, જે સામાન્ય રીતે બાળક ૪ વર્ષનું થાય પછી કરાવવું.
એડીનોઇડસ :
એડીનોઇડસ(નાકની પાછળના મસા) પણ નાના-નાના ટોન્સીલ જ છે જે નાકની પાછળમાં થતા હોય છે. તેમાં વારંવાર ઇન્ફેક્શન થવાથી તે મોટા થાય છે, જેથી બાળકને નાકથી શ્વાસ લેવાતો નથી. બાળક મોઢું ખુલ્લું રાખી શ્વાસ લે છે અને રાત્રે ઊંઘમાં નસકોરાં બોલાવે છે. આથી બાળકને મોઢાંમાંથી વાસ પણ આવે. એડીનોઇડ્સનું આૅપરેશન ૨ વર્ષ પછી કરાવી શકાય. ઘણીવાર આ આૅપરેશન કાકડા સાથે પણ કરવામાં આવે છે. •
HINDI
टॉन्सिल और एडीनोइड्स
टॉन्सिल, गले के भीतर जीभ के पीछे दाई और बाई ओर होता हैं। बच्चों में टॉन्सिल का संक्रमण एक आम बात है और उचित एंटीबायोटिक से इसे ठीक किया जा सकता है। लेकिन बार-बार टॉन्सिल के संक्रमण के कारण यदि बच्चे के स्वास्थ में जोखिम हो तो ऑपरेशन कराना आवश्यक हो जाता है। सामान्यतः यह ऑपरेशन बच्चे के ४ वर्ष का हो जाने के बाद किया जाना चाहिए।
एडीनोइड्स – नाक के पीछे छोटे-छोटे टॉन्सिल या एक प्रकार का मसा है। इनमें बार-बार संक्रमण होने पर यह बड़े हो जाते है। इस कारण बच्चा नाक के द्वारा श्वास नहीं ले सकता है। बच्चा मुँह खोलकर श्वास लेता है और रात में नींद में खर्राटें भरता है। इस कारण बच्चे के मुँह से दुर्गंध भी आती है। एडीनोइड्स का ऑपरेशन २ वर्ष की आयु के बाद किया जा सकता है। कई बार यह ऑपरेशन टॉन्सिल के साथ किया जाता है। •
Abdominal Wall Defects – Gastroschisis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
GASTROSCHISIS
Gastroschisis is a type of abdominal wall defect which occurs when the child’s abdomen does not develop fully while inside the womb. It affects 1 in every 3000 children. In gastroschisis, the intestines are open to the air when the child is born.
The umbilical cord is visible but pushed to the side by the exposed intestines.
Gastroschisis is a serious condition and needs prompt treatment soon after birth. Immediately after birth, the exposed intestines need to be wrapped in a sterile saline soaked cloth which reduces the amount of fluids and body heat lost and protects the intestines from further damage.
Once the child is stable, it will have an operation to put the intestines back inside the abdomen. Occasionally a ready made plastic bag / mesh is placed over the intestines and they are gradually moved back into the abdomen which may take a few days. ●
ગેસ્ટ્રોસ્ચેસીસ
દર ૩૦૦૦ એ ૧ બાળકમાં જાવામાં આવતી આ ખોડમાં પેટની દીવાલનાં વિકાસના અભાવે બાળકના જન્મ સમયે તેના પેટનાં આંતરડા પેટની બહાર રહેલા હોય છે.
બાળકનો જન્મ થતાં જ આ ખોડ જાઈ શકાય છે. આંતરડા દૂંટીની નાળની જમણી બાજુએથી બહાર નીકળતા હોય છે. આ ખોડમાં બાળકને તાત્કાલિક સારવારની જરૂર પડે છે. સારવાર અર્થે મોકલતાં પહેલા બાળકનાં આંતરડાને ચોખ્ખા સલાઈનવાળા કપડાંથી ઢાંકી દેવા જાઈએ. બાળકની સ્થતિને સ્ટેબીલાઈઝ કર્યા બાદ ઓપરેશન દ્વારા આંતરડાને પેટમાં પાછા મૂકીને પેટની દીવાલ બંધ કરવી પડે છે. અમુક કેસમાં આંતરડાને પ્લાસ્ટીકની બેગમાં મૂકી ધીરે ધીરે પેટમાં પાછા મુકાય છે. •
गेस्ट्रोस्काईसीस
गेस्ट्रोस्काईसीस पेट की दीवार का एक प्रकार का दोष है। हर ३००० में १ बच्चा इस दोष से प्रभावित होता है। गेस्ट्रोस्काईसीस की स्थिति में, उदर की दीवार पूर्णरूप से निर्मित नहीं हो सकने के कारण आंतें बाहर विकसित होती हैं और बच्चे के जन्म के समय शरीर से बाहर खुले में रह जाती है।
गेस्ट्रोस्काईसीस की पहचान तुरंत ही हो जाती है। गर्भनाल दिखाई देती है परंतु वह खुले आंतों के कारण एक ओर धकेली सी दिखाई देती है। गेस्ट्रोस्काईसीस एक गंभीर परिस्थिति है। जन्म के तुरंत बाद इसका उपचार किया जाना आवश्यक होता है। जन्म के तुरंत बाद, बच्चे को पानी में भीगोए जंतुरहित कपड़े में लपेट लेना चाहिए। इससे बच्चे के शरीर से पानी तथा ऊष्मा का नाश कम होगा और आंतों को नुकसान से सुरक्षित रखेगा। बच्चे के स्थिरता प्राप्त कर लेने के उपरांत, आंतों को उदर में पुनःस्थापित करने हेतु एक ऑपरेशन किया जाता है। कभी-कभार एक प्लास्टिक की तैयार थैली/जाली खुली आंतों पर रख दी जाती है, तत्पश्चात, आंतों को क्रम से उदर में स्थापित कर दिया जाता है। इसमें कुछ दिनों का समय लग सकता है। •
Ambiguous Genitalia / Disorders of Sexual Differentiation / Intersex
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
INTERSEX / DISORDERS OF SEXUAL DIFFERENTIATION / AMBIGUOUS GENITALIA
At conception, a fetus’s gender is already determined based on the 23rd pair of chromosomes it inherits from the parents. Females have two X chromosomes and males have an X and a Y chromosome. The sexual organs of males and females develop from the same fetal tissue. The main factor controlling the next step is male hormones. The presence of male sex hormones causes male organs to develop and the absence of male hormones causes female organs to develop. Without enough male hormones, a genetic male will develop ambiguous genitalia. Likewise, a genetic female will develop ambiguous genitalia if male hormones are present.
Characteristics of ambiguous genitalia in genetic females:
- An enlarged clitoris which appears to be a small penis
- A concealed vagina
Characteristics of ambiguous genitalia in genetic males:
- Microphallus
- Severe degree of hypospadias
- Bilateral undescended testes
What is the long-term outlook for a child with ambiguous genitalia?
Intersex is a major social challenge also. A complete and thorough investigation with in-depth counselling of the family is mandatory to manage these children. ●
GUJARATI
ઇન્ટરસેક્સ
બાળકનું લીંગ માતા-પિતામાંથી મળેલ સેક્સ ક્રોમોઝોમ્સ પર નિર્ભર છે. સ્ત્રીઓ માં XX ક્રોમોઝોમ્સ અને પુરૂષોમાં XY ક્રોમોઝોમ્સ હોય છે. બાળકની જનેન્દ્રિયો નો વિકાસ ગર્ભ દરમ્યાન થયેલ હોરમોન્સની અસરથી જ થાય છે. હોરમોન્સની થોડી પણ ચૂક/ વધુ અસર/ઓછી અસરના કારણે ઇન્ટરસેક્સના પ્રોબ્લેમ ઉભા થાય છે.
ઇન્ટરસેક્સ એક મોટી મેડીકલ અને સોશીયલ ચેલેન્જ છે. બાળકના જન્મ સમયે જા નીચે જણાવેલ ચિન્હો દેખાય તો ડાક્ટરે તેને બાબો/બેબી જાહેર કરવાની ઉતાવળ કરવી ના જાઈએ. આવા બાળકોને બાળકોના સર્જન દ્વારા તપાસ અને રીપોર્ટ કરાવવા જરૂરી હોય છે. આજના જમાનામાં એન્ડોસ્કોપી અને લેપ્રોસ્કોપી આ બાળકોના લિંગના સચોટ નિદાન અને તેની યોગ્ય સારવાર માટે ખૂબ જ મદદરૂપ થાય છે.
ઇન્ટરસેક્સના ચિન્હો :
(૧) બાળકીઓ (XX) માં ઇન્ટરસેક્સના ચિન્હો :
– યોનિમાર્ગની ઉપર ભગ્નનો આકાર લિંગ જેવો હોવો
– યોનિમાર્ગ બંદ હોવો/ન હોવો
(૨) બાબાઓ (XY) માં ઇન્ટરસ્ક્સના ચિન્હો :
– બાળકી જેવી જનેન્દ્રિયો હોવી.
– પેશાબનો માર્ગ લિંગની નીચે/પાછળ હોવો.
– લિંગ નો ભાગ ખૂબ જ નાનો હોવો અને પેશાબનો રસ્તો ખોટી જગ્યાએ હોવો.
– વૃષણની બંન્ને ગોળી વૃષણ કોથળીમાં ન હોવી. •
HINDI
इंटरसैक्स/यौन भेदभाव का विकार/अस्पष्ट जननांगता
गर्भधारण के समय से ही, अपने माता-पिता से विरासत में प्राप्त २३वें गुणसूत्र के आधार पर भ्ा्रूण का लिंग निश्चित हो जाता है। कन्या में दो ङ्ग गुणसूत्र होते हैं और पुरूष बालक में एक ङ्ग और एक Y गुणसूत्र होता है। पुरूषों और महिलाओं के जनन अंगों का विकास एक ही भ्ा्रूण मांस-तंतु से होता है। अगले चरण को नियंत्रित करनेवाले मुख्य कारक पुरूष हार्मोन है। पुरूष अंगों के विकास का कारण पुरूष जनन हार्मोन की उपस्थिति है और इनकी अनुपस्थिति महिला जनन अंग विकसित करता है। अपर्याप्त पुरूष हार्मोन के कारण आनुवांशिक पुरूष में अस्पष्ट जननांगता का विकास होता है। इसी प्रकार, पुरूष हार्मोन की उपस्थिति के कारण आनुवांशिक महिला में अस्पष्ट जननांगता का विकास होता है।
आनुवांशिक महिलाओं में अस्पष्ट जननांगता के लक्षणः
१. बढ़ा हुआ भगशेफ (Clitoris), जो लघु शिश्न (Penis) सा प्रतीत होता है।
२. छुपा योनि।
आनुवांशिक पुरूषों में अस्पष्ट जननांगता के लक्षणः
१. गैर पहचान योग्य (अथवा अस्पष्ट) पुरूष गुप्तांग।
२. अनुपस्थित जननपिंड के साथ गंभीर अधोमूत्रमार्गता।
३. एक बहुत ही छोटा शिश्न जिसका मूत्रमार्ग अंडकोश की थैली के पास खुला हो।
४. दोनों ही अंडकोशों का अनुपस्थित होना और अंडकोश की थैली का अविकसित होना।
इंटरसैक्स एक प्रमुख सामाजिक चुनौती भी है। ऐसे बच्चों के उपचार के लिए परिवारवाले से बारीकी से परामर्श करने के साथ गहन जांच अनिवार्य है। कई बार, एक निश्चित निदान पर पहुंचने के लिए बहुविशिष्ट दृष्टिकोण आवश्यक होता है। अस्पष्ट जननांगता के साथ जन्मे कुछ बच्चों के जनन अंग सामान्य होते हैं जो उन्हें प्रजननक्षम जीवन व्यापन करने की अनुमति प्रदान करते हैं। अन्य कुछ प्रजननक्षम नहीं होते हैं अथवा वे गर्भधारण करने में कठिनाई का अनुभव करते हैं। कभी-कभार बाद के जीवनकाल में उनके जननअंग में गांठ हो जाने का खतरा होता है।•
Acute Scrotum / Torsion Testis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Acute Scrotum / Torsion Testis
Acute scrotum is sudden onset of redness and swelling over the scrotum. This is associated with severe pain over the scrotum and sometimes lower abdomen and may be accompanied with nausea and vomiting.
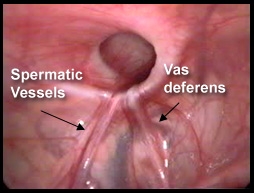
Of the many causes of acute scrotum, the most common and important is Torsion of Testis. The testis is supplied by a single blood vessel and any torsion on this vessel may impede the blood supply to the testis. If urgent medical attention and intervention is not done, this may result in testicular gangrene and orchidectomy ( removal of the dead testis) may be needed.
The commonly misleading history given by the parents is that the child may have had a trivial trauma or an insect bite. However, for the clinician the golden rule should be ‘Any acute scrotum is testicular torsion unless proved otherwise’. Investigations like ultrasound and color doppler may be done to help in the diagnosis. However, in the event of any doubt, it is safest to do a surgical exploration of the scrotum. The other uncommon causes of acute scrotum are acute epidydymo orchitis, scrotal abscess, idiopathic scrotal oedema and torsion of appendix of the testis. ●
 Acute Scrotum (Right scrotal Abscess)
Acute Scrotum (Right scrotal Abscess)

 Torsion of Left Undescended Testis (Pre operative and Operative Photo)
Torsion of Left Undescended Testis (Pre operative and Operative Photo)
 Acute Scrotum
Acute Scrotum

 Torsion Testis (Pre and Per operative photo)
Torsion Testis (Pre and Per operative photo)
GUJARATI
એક્યુટ સ્ક્રોટમ બાળકોમાં જાવામાં આવતી એક ગંભીર તકલીફ છે. આ બીમારી દર ચાર હજારે એક બાળકમાં જાવા મળે છે. નિદાનમાં મોડું થવાથી બાળક પોતાની વૃષણની ગોળી ખોઈ શકે છે. આ બીમારીમાં બાળકને વૃષણની કોથળી ઉપર લાલાશ અને સોજા જાવામાં આવે છે. આ સાથે બાળકને સખત દુઃખાવો અને ઉલટીઓ પણ થાય છે, જ્યારે બાળક ડાક્ટર પાસે લાવવામાં આવે ત્યારે તેના મા-બાપ અચૂક કહે છે કે, ‘બાળકને કદાચ સૂતી વખતે કોઈ જીવડું કરડી ગયું છે’ અથવા ‘કોઈ વસ્તુની ઍલર્જી થઈ છે’ અથવા તો ‘કંઈક વાગ્યું હશે’ તેના કારણે આ લાલાશ અને સોજા થયો છે. પરંતુ, આ વૃષણની ગોળી વળ ખાવાનાં કારણે થાય છે. જેને અંગ્રેજીમાં ‘ટોરઝન ટૅસ્ટીસ’ કહેવામાં આવે છે. વૃષણની ગોળી એક જ લોહીની નળી ઉપર લટકતી હોય છે. ગોળી વળ ખાઈ જવાથી તેને લોહી મળતું બંધ થઈ જાય છે. આ તકલીફનાં છ થી આઠ કલાકમાં આૅપરેશન કરવામાં ન આવે તો લોહી નહીં મળવાનાં કારણે ગોળી મરી જાય છે. આવા કેસમાં બાળકની વૃષણની ગોળી કાઢી નાખવી પડે છે. આથી જ્યારે પણ બાળકને ગોળી ઉપર લાલાશ કે સોજા હોય અને તેની સાથે દુખાવો પણ હોય તો તાત્કાલિક બાળકોના સર્જન ડાક્ટરનો સંપર્ક કરવો જાઈએ. •
HINDI
टॉर्शन वृषण/तीव्र अन्तग्ा्र्रथन (एक्यूट स्क्रोटम)
एक्यूट स्क्रोटम में वृषण पर अचानक लवण की शुरुआत होती है और सूजन होती है। इसके साथ ही अंडकोश की थैली में और कभी-कभी पेट के नीचले हिस्से में असहनीय दर्द के साथ मतली और उलटी होती है। अक्यूट स्क्रोटम के कई कारणों में सबसे सामान्य और मुख्य कारण है टेस्टिस में मरोड़ होना। एक ही खून की नली से टेस्टिस की आपूर्ति की जाती है और इस नली में कोई मरोड़ होने पर टेस्टिस को खून पहुँचाने में बाधा उत्पन्न हो सकती है। यदि तत्काल चिकित्सा और बचाव नहीं किया गया तो परिणाम स्वरूप टेस्टीकुलर गैंग्ा्रीन हो सकता है और ऑर्किडेक्टोमी करने की आवश्यकता पड़ सकती है।
आमतौर पर माता-पिता द्वारा यह भ्रामक विवरण दिया जाता है कि बच्चे को कदाचित हल्की चोट लगी होगी या किसी कीड़े ने काटा होगा। हालांकि, चिकित्सक के लिए स्वर्णिम नियम यह होना चाहिए कि ‘कोई भी एक्यूट स्क्रोटम वृषण टॉर्शन है जब तक कि अन्यथा साबित नहीं हो जाता है’। निदान में सहायता हेतु अल्ट्रासाउण्ड तथा कलर डॉप्लर जैसी जांच की जानी चाहिए। हालांकि, किसी भी संदेह की स्थिति में, अंडकोश की शल्य चिकित्सीय जांच पड़ताल करना सबसे सुरक्षित होगा। तीव्र अन्तग्ा्र्रथन के अन्य असामान्य कारणों में तीव्र एपिडायडिमूरचाइटिस, अंडकोषीय फोड़ा, इडियोपैथिक स्क्रोटल एडिमा और वृषण की पुच्छ के मरोड़ होते हैं। •
Appendicitis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
APPENDICITIS
Appendicitis is commonly caused by consuming unhygienic food and water. This causes the child to have recurrent abdominal pain, poor appetite and school drop outs. Recurrent appendicitis can also cause glands around the intestines to enlarge (Mesenteric lymphadenitis).
Acute appendicitis can cause severe abdominal pain which commences around the umbilicus and then migrates to the right lower abdomen. This can be accompanied with nausea, vomiting and fever. This can be diagnosed by clinical examination and confirmed by ultrasound scan and blood investigations. Acute appendicitis in younger age has a higher chance of perforation which may cause a sudden deterioration in the child’s general condition.
Most of the children with acute appendicitis require surgery. Surgery is commonly done by laparoscopy and the child is able to go home the very next day. ●
 Acute Appendicitis
Acute Appendicitis
 Gangrenous Appendicitis
Gangrenous Appendicitis
 Chronic Appendicitis
Chronic Appendicitis
 Acute Suppurative Appendicitis
Acute Suppurative Appendicitis
 Appendicitis with perforatiom
Appendicitis with perforatiom
GUJARATI
એપેન્ડીસાઇટીસ (એપેન્ડીક્સનું ઇન્ફેક્શન)
વધુ પડતાં બહાર ખાવાની ટેવ અને ચોખ્ખું પાણી ન પીવાનાં કારણે બાળકોમાં એપેન્ડીક્સ પર સોજા અને તેના લીધે પેટમાં ગાંઠો ખૂબ જ સામાન્ય છે. આનાથી બાળક અવાર નવાર પેટનાં દુઃખાવાથી પીડાય છે અને ઘણી વાર બાળકની સ્કૂલમાં રજાઓ પડે છે.
એપેન્ડીક્સનો એકયુટ એટેક એટલે પેટમાં દુઃખાવા (જે દૂંટી અથવા પેટની જમણી બાજુમાં હોય છે) સાથે ઉલ્ટી થવી અને તાવ આવવો. ડાક્ટરી તપાસ અને સોનોગ્રાફી/લોહીની તપાસથી આનું ચોક્કસ નિદાન થાય છે. એપેન્ડીસાઇટીસ બાળકને નાની ઉંમરે પણ થાય છે અને આવી ઉંમરે એપેન્ડીક્સ ફાટી જતાં બાળક ઘણું સીરિયસ થઈ શકે છે.
લેપ્રોસ્કોપી (દૂરબીન)થી એપેન્ડીક્સનું આૅપરેશન કરાવી એક દિવસમાં બાળક હોસ્પિટલમાંથી સારું થઈ ઘરે જાય છે. •
HINDI
एपेंडीसाइटिस (एपेंडीक्स का संक्रमण)
बाहर का खाना खाने की आदत अथवा अशुद्ध पानी पीने के कारण बच्चे के एपेंडीक्स पर सूजन और उस कारण पेट में गांठ बनना सामान्य है। इस कारण बच्चे के पेट में रह-रह कर दर्द उठता है और कई बार स्कूल से छुट्टियां लेनी पड़ती है।
एपेंडीक्स का तीव्र घात आने पर पेट में दर्द के साथ (जो नाभि अथवा पेट के दाई ओर होता है) उल्टी, बुखार आता है। डॉक्टर से जांच और सोनोग्राफी /खून की जांच से ही इसका निदान हो सकता है। बच्चों में एपेंडीसाइटिस छोटी उम्र में भी होता है और तब यह फट भी जाता है और बच्चे की हालत गंभीर हो जाती है।
लेप्रोस्कोपी (दूरबीन से जांच) से एपेंडीक्स का ऑपरेशन किया जा सकता है और बच्चा एक दिन में अस्पताल से घर जा सकता है। •
Abdominal Pain / Recurrent Abdominal Pain
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
RECURRENT ABDOMINAL PAIN & MESENTERIC LYMPHADENOPATHY
Recurrent abdominal pain is a common and vexing problem in children especially between 2 and 10 years. Abdominal pain which causes disturbance in sleep, school drop outs and hindrance in day to day activities of the child needs medical attention. It is mandatory to get the child checked up by a doctor and get an ultrasound scan done if necessary.
Ultrasound scan is a common and non invasive investigation which does not have any radiation exposure. It can pick up pathologies that are not visible on the outside or may not be apparent on clinical examination. One of the most common things that is picked up on ultrasound scan is enlarged mesenteric lymph nodes. The most common cause of this is intestinal infections or appendicitis. Rarely they can be due to tuberculosis or malignancy. In a well child, the size of these glands may be monitored by ultrasound scan on a monthly basis. If the size of the glands persist to 1.5 cm or larger and if there are multiple glands in the abdomen, a laparoscopic biopsy of the mesenteric lymph nodes may be helpful to arrive at a scientific diagnosis. ●
GUJARATI
પેટનો દુઃખાવો અને પેટની ગાંઠો
બાળકોમાં (ખાસ કરીને ૨ થી ૧૦ વર્ષની ઉંમરનાં બાળકોમાં) પેટનો દુઃખાવો વારંવાર થવો તે એક સામાન્ય પણ જટિલ પ્રોબ્લેમ છે.
અવારનવાર પેટમાં દુઃખાવો જેનાથી બાળકની ઊંઘ બગડતી હોય, સ્કૂલમાંથી પાછા આવવું પડતું હોય અથવા તેની રોજિંદી પ્રવૃત્તિમાં અડચણ આવે તો તેવા સંજાગોમાં બાળકની ડાક્ટરી તપાસ અનિવાર્ય બને છે. સામાન્ય તપાસમાં ચિન્હો ન જણાતાં લેબોરેટરી તપાસ અને રેડિયોલોજી ટેસ્ટ કરાવવા પડે છે.
સોનોગ્રાફી એક સામાન્ય અને હાનિરહિત તપાસ છે. પેટમાં દુઃખાવાની તપાસ દરમ્યાન આંતરડાની આજુબાજુમાં ગાંઠો હોવાનું નિદાન સોનોગ્રાફીમાં થતું હોય છે. આ થવાનું મુખ્ય કારણ આંતરડાનું ઇન્ફેક્શન અથવા એપેન્ડીક્સનો સોજા છે. ઘણીવાર ટી.બી. અને કેન્સરની શરૂઆત પણ આ ગાંઠોનું કારણ હોય છે. આવા સમયે આ ગાંઠોની સાઈઝ ૧ મહિનાનાં અંતરે બે-ત્રણ સોનોગ્રાફીની તપાસ કરાવી માપવામાં આવે છે. ૧.૫ સેમી. અથવા મોટી સાઈઝની એક થી વધુ ગાંઠો આવે તો લેપ્રોસ્કોપી દ્વારા આૅપરેશન કરી પેટની સંપૂર્ણ તપાસ થાય છે અને એક અથવા વધુ ગાંઠો કાઢી તેની બાયપ્સી દ્વારા સચોટ નિદાન કરાવવું પડે છે. ૯૦% ગાંઠો સામાન્ય ઇન્ફેક્શનના કારણે હોય છે અને તે ચિંતાનું કારણ હોતી નથી. •
HINDI
पेट दर्द एवं पेट में गाँठ
बच्चों में बार-बार पेट दर्द की शिकायत आम है, विशेष रूप से २ से १० वर्ष की आयु के बच्चों में यह समस्या रहती है। पेट दर्द के कारण बच्चे की नींद खराब होना, स्कूल से बार-बार छुट्टी लेना और बच्चे के दैनिक क्रियाकलापों में बाधा होना, इन स्थितियों में डॉक्टर से पामर्श लेना जरूरी है। आवश्यकता पड़ने पर सोनोग्राफी करानी चाहिए।
सोनोग्राफी एक समान्य और हानिरहित जाँच है जिसमें विकिरण का प्रभाव नहीं पड़ता। सोनोग्राफी करने से पेट के भीतर दर्द होने के कारण, आँतों के आसपास गाँठों के होने का पता लगाया जाता है। आँतों का इंफेक्शन या एपेन्डिक्स की सूजन इसका सबसे प्रमुख कारण है, जिसकी पहचान सोनोग्राफी से की जा सकती है। इन गाँठों के होने का कारण टी.बी या कैंसर के होने की शुरूआत भी हो सकती है। ऐसी स्थिति में एक महीने के अंतराल पर दो-तीन सोनोग्राफी से जाँच करके इन गाँठों के आकार को मापा जाता है। १.५ से.मी या उससे बड़ी आकार की एक या अधिक गाँठें होने पर लेप्रोस्कोपी करके पेट की संपूर्ण जाँच की जाती है। इसमें बायोप्सी से गाँठ के अंश को निकाल कर जाँच द्वारा रोग की पक्की पहचान की जाती है। ९०% गाँठें सामान्य इन्फेक्शन के कारण होती है, जो चिंता का विषय नहीं हैं। •
Anaesthesia (Pediatric Anaesthesia)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
PEDIATRIC ANAESTHESIA
A major concern of all parents for their child undergoing surgery is anaesthesia. Most of the parents are worried as to how can a small child be anaesthetized and whether the procedure can be done under a local anaesthetic. One of the major concerns is whether the child will recover uneventfully from the anaesthetic.
Anaesthesia is an age old scientific speciality. As with other specialities, pediatric anaesthesia has also advanced over the years. Anaesthesiologists specially trained in the field of pediatric anaesthesia can now safely anaesthetize even new born and premature children.
Operating under local anaesthesia is most of the times not possible in children as the child is not co-operative and gets scared amongst unknown people and enviornment in the operating room.
Maintainence of anaesthesia during surgery is done using the most modern medicines and latest equipments which are safe and have the least side effects. ●
GUJARATI
પીડીઆટ્રીક એનેસ્થેસીઆ
મોટા ભાગનાં મા-બાપને તેમના બાળકનું આૅપરેશન કરાવતાં પહેલા એક જ સવાલ હોય છે. “આટલા નાના બાળકને બેભાન કરી શકાય?”, “બાળકને લોકલ એનેસ્થેશિઆ ના અપાય?”, “બાળક કોમામાં નહીં જાય ને?”
એનેસ્થેશિયાને સામાન્ય ભાષામાં “શીશી સૂંઘાડવા” તરીકે ઓળખાય છે.
શીશી સૂંઘાડવાની રીત ખૂબ જ દાયકાઓ જૂની હતી. હાલમાં એનેસ્થેશિયા માટે ઇન્જેક્શન દ્વારા નસમાં દવા અપાય છે અને બાળકને સેકંડોમાં બેભાન કરી શકાય છે.
એનેસ્થેશિયાના ખૂબ જ આધુનિક સાધનો દ્વારા નાનામાં નાના બાળકને (અધૂરા માસે જન્મેલા બાળકને પણ) બેભાન કરાય છે અને મશીન બંધ કરતાં, બાળકને તરત ભાનમાં લાવવામાં આવે છે. આ કાર્ય માટે બાળકના નિષ્ણાંત એનેસ્થેટીસ્ટ ડાક્ટર કામ કરે છે.
બાળકોમાં મોટે ભાગે લોકલ એનેસ્થેશિયા આપી શકાતો નથી કારણ કે બાળક આૅપરેશન થિએટરમાં ગભરાઈ જાય છે અને સર્જનને સહકાર આપતું નથી જેથી આૅપરેશન કરી શકાય નહીં. “જનરલ એનેસ્થેશિયા” હવે ખૂબ જ સલામત છે તેથી “લોકલ એનેસ્થેશિયાની” ચોઈસ ડાક્ટર તથા માતા-પિતા નથી લેતા. •
HINDI
पीडीऐट्रीक ऐनेस्थेशिया
अपने बच्चे का ऑपरेशन करवाने से पहले अधिकतर माता-पिता के मन में कई सवाल उठते हैं- जैसे कि क्या इतने छोटे बच्चे को बेहोश किया जा सकता है क्या बच्चे को लोकल ऐनेस्थेशिया दे सकते हैं कहीं बच्चा कोमा में तो नहीं चला जाएगा आदि।
आमतैर पर यह मानते है कि बच्चे को शीशी सुंघाकर बेहोश किया जाता है, जो कि बहुत पुरानी पद्धति थी। आज के समय में ऐनेस्थेशिया के लिए इन्जेक्शन से नस में दवा दी जाती है और बच्चा कुछ सेकण्डों में बेहोश हो जाता है।
ऐनेस्थेशिया द्वारा अत्याधुनिक उपकरणों से छोटे से छोटे बालक को बेहोश कर सकते हैं और मशीन बंद करके बच्चों को तुरंत होश में ला सकते हैं। यह कार्य बाल विशेषज्ञ ऐनेस्थेटीस्ट डॉक्टर द्वारा किया जाता है।
लोकल ऐनेस्थेशिया देकर बच्चे का ऑपरेशन करना संभव नहीं हो पाता। क्योंकि बच्चा ऑपरेशन थिएटर और अनजान लोगों को देखकर डर जाता है और ऑपरेशन के दौरान डॉक्टर को सहयोग नहीं करता।
जनरल ऐनेस्थेशिया द्वारा सर्जरी के दौरान अत्याधुनिक दवाओं और विशेष उपकरणों से बच्चे को बेहोश रखा जाता है, जो कि सुरक्षित तरीका है। •
Bronchoscopy
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a bronchoscopy and why does my child need one?
A bronchoscopy is a procedure that allows the doctor to look inside your child’s airway (trachea and bronchi). During the procedure, the doctor may also take a biopsy (small sample of tissue) or wash out secretions. The secretions will be sent to the laboratory to look for infection. Bronchoscopy is also done to remove any foreign body or particle that your child has inadvertently inhaled and has stuck in his air passage.
Bronchoscopy is also done after an operation to the trachea, bronchi or lungs to check that they are healing well.
What does a bronchoscopy involve?
Your child will have the bronchoscopy under general anaesthetic. The doctor will pass a bronchoscope (a thin, tube with a bright light at the end) down into your child’s airway. He or she will then be able to examine the airways closely. Once the bronchoscopy has finished, the doctor will remove the bronchoscope and spray some local anaesthetic on the back of your child’s throat.


Left Bronchus & Bronchiole


Right Bronchus & Bronchioles

Main Bronchus

Carina

Epiglottis
Impacted Peanut in the Bronchus seen at Bronchoscopy
What happens afterwards?
Your child will wake up from the general anaesthetic in a separate recovery room. Some children wake up straightaway but others may sleep for another two hours or so.
About three hours after the procedure, once your child is awake and sitting up on his or her own, he or she will be able to eat and drink.
GUJARATI
શ્વાસનળીમાં ફારેન બોડી
નાના બાળકોને કોઈપણ વસ્તુ મોંમાં મૂકવાની ટેવ હોય છે. કોઈપણ કારણસર રડતાં, હસતાં, ઉંડો શ્વાસ લેતાં મોંમાં રાખેલી વસ્તુ સીધી શ્વાસનળી અને તેની આગળ ફેફસાંની નળીમાં ભરાઈ જાય છે. આવું થાય ત્યારે બાળકને ખૂબ જ
ઉધરસ આવે છે. ઘણીવાર આ અકસ્માત ભૂલાઈ જાય છે. ઘણા દિવસો પછી પણ બાળકને ખાંસી મટતી ન હોવાથી બાળકનો છાતીનો X-ray પડાવવામાં આવે છે, અને તેમાં જા મેટાલીક ફારેન બોડી હોય તો દેખાય છે, પણ જાૅ
બિન મેટાલીક (દા.ત, સીંગનો દાણો) હોય તો તે દેખાતો નથી, પરંતુ ફેફસાંમાં દેખાતાં બદલાવ (Emphysema)થી ફારેન બોડી છે તેવો ખ્યાલ આવે છે.
જાૅ ફારેન બોડી મુખ્ય શ્વાસનળીમાં ફસાય તો બાળકને શ્વાસ લેવામાં સખત તકલીફ પડે છે અને ઘણીવાર બાળક મરણ પણ પામે છે. તાત્કાલીક શ્વાસનળીની દૂરબીનની તપાસ (બ્રોન્કોસ્કોપી) બાળકને બચાવે છે.
હોસ્પિટલ માં તાત્કાલીક પહોંચી શકાય તેમ ન હોય તો બાળકને ઊંધું પગથી લટકાવી, બરડા પર મારવાથી ફારેન બોડી શ્વાસનળીમાંથી નીકળી શકે.
જાૅ ફારેન બોડી નાની શ્વાસનળીની (બ્રોન્કસ) હોય તો પણ બ્રોન્કોસ્કોપીથી તેને કાઢવાથી બાળક તરત સા૨ું થઈ જાય છે.
શ્વાસનળીમાં સીંગનાં દાણા,ચણા,કચૂંકા અથવા અનેક જાતની મેટાલીક વસ્તુઓ બ્રોન્કોસ્કોપી દ્વારા કાઢી શકાય છે. •
HINDI
श्वासनली में फंसी बाहरी वस्तुएँ
छोटे बच्चों में किसी वस्तु को मुँह में डालने की आदत होती है। किन्हीं कारणों, जैसाकि बच्चों का रोना, हंसना, गहरी साँस लेना आदि के दौरान मुँह में रखी वस्तु सीधी श्वास नली से होकर के फेफड़ों की नली में फंस जाती है। ऐसा होने पर बच्चे को अत्यधिक खाँसी आती है। कई बार ऐसी घटना की ओर ध्यान नहीं जाता है। कई दिनों तक बच्चे की खाँसी मिटती नहीं है और धीमा बुखार भी रहता है। ऐसे में डॉक्टर भी कई बार एंटीबायोटिक और खाँसी की दवाई देते हैं। इसके बाद भी अगर खाँसी बंद नहीं होती है तो छाती का एक्स-रे करवा लेना चाहिए, जिससे यदि कोई धातु वाली वस्तु हो तो दिखाई देगी। यदि जैविक वस्तु (उदा. मूँगफली का दाना) हो तो एक्स-रे में दिखाई नहीं देगा, लेकिन फेफडों में हो रहे परिवर्तन के लक्षणों (एम्फायसेमा) से इसका अंदेशा मिल जाता है।
यदि बाहरी वस्तु श्वास नली में फंस जाती है तो बच्चे को साँस लेने में कठिनाई होती है और उसकी मृत्यु भी हो सकती है। तुरंत श्वास नली की दूरबीन से जांच (ब्रोंकोस्कोपी ) कर के बच्चे की जान बचाई जा सकती है।
यदि बाहरी वस्तु श्वास नली की शाखा (ब्रोंकस) में फंसी हो तो ब्रोंकोस्कोपी द्वारा उसे निकाल देने से बच्चा तुरंत स्वस्थ हो जाता है।
श्वास नली में मूँगफली का दाना, चना, कूंचा अथवा धातु की वस्तु की उपस्थिति की जाँच ब्रोंकोस्कोपी द्वारा की जाती है। ऐसी आपात परिस्थिति में जल्द से जल्द उपचार किया जाना चाहिए। •
Bladder Exstrophy and Epispadias
Exstrophy means ‘turned inside out’. Bladder exstrophy is a congenital (present at birth) abnormality of the bladder. It happens when the skin over the lower abdominal wall (bottom part of the abdomen) does not form properly, so the bladder is open and exposed on the outside of the abdomen.
In epispadias, the urethra does not form properly. All boys with bladder exstrophy also have epispadias, but epispadias can also be isolated and occur on its own.
In boys, the urethra may be very short and split, and as a result it emerges on the top surface of the penis rather than in its usual position at the end of the penis. The split may be small, or, when it occurs in boys born with bladder exstrophy, it may involve the full length of the penis, making the penis short and broad.
In girls, the opening of the urethra is higher and wider than usual, the labia (the lip-like folds encircling the vaginal opening) are further apart than normal and the clitoris (a small, very sensitive part of the female genitalia) is split in two.
What features are associated with bladder exstrophy?
As well as the bladder being exposed, babies with bladder exstrophy may also have related problems affecting their urinary system and pelvic bones. These related problems vary in severity and do not affect every baby. These will be confirmed using ultrasound scans and x-rays, and may be corrected during a series of operations.
They include:
- Problems with the neck of the bladder and sphincter (ring of muscle that squeezes and relaxes to let urine flow from the bladder)
- The bladder has a smaller capacity than usual, so cannot hold much urine
- The ureters join the bladder in a different place to normal
- The middle part of the pelvic bones are separated
Bladder exstrophy can be associated with other problems, but the doctor will examine your child closely to see if this is the case. Some may need to be corrected with an operation, but others do not.
The more common problems include:
- The anus is further forward than usual
- The umbilicus (belly button) is lower down than usual
- Umbilical and Inguinal Hernia, where part of the abdominal lining and sometimes a section of intestine bulges out through a weak area in the abdominal wall muscles
- Undescended testes, where the testicles are not in their usual place in the scrotum
How are bladder exstrophy and epispadias diagnosed?
Bladder exstrophy is sometimes diagnosed before birth using ultrasound scans. However, it is often not picked up before birth, but will be obvious once your baby is born.
Epispadias in boys is usually identified at birth, but in girls the diagnosis is usually made later when they develop bladder control problems or infections.
What causes bladder exstrophy and epispadias?
We do not know why bladder exstrophy occurs. It affects the developing baby during very early stages of development, at about four to six weeks into the pregnancy. This is when organs, muscles and other tissues start to form. It is not the result of anything either parent did or did not do, and is not simply an inherited condition.
How common is bladder exstrophy?
Bladder exstrophy occurs in one in every 40,000 births, affecting two to three times more boys than girls. If you have a baby with bladder exstrophy the chance of having another baby with bladder exstrophy is increased to about one in 100.
How are bladder exstrophy and associated problems treated?
Bladder exstrophy and epispadias are corrected in a series of operations over the first few years of life. The overall aim of treatment is to prevent any kidney damage and correct the abnormalities so that your child’s urinary system and genitals work properly and look as normal as possible.
The doctor will explain the treatment plan for your child; this can vary from child to child.
What do the operations involve?
Bladder and abdominal wall repair operation – first few days after birth
This operation closes the bladder and abdominal wall, so that that the bladder is inside the body and in the correct position. After the operation, urine will drain from the bladder through a number of catheters (plastic tubes) placed in the bladder.
You and your child will be able to go home once your child is recovering and has been reviewed by the doctors.
Bladder neck reconstruction procedure – at one to two years old
After the initial closure of the bladder exstrophy, there is no sphincter at the junction of the bladder and urethra. Surgery for bladder neck reconstruction uses existing muscle and soft tissue to create a ring of muscle that acts like a sphincter. This holds urine in the bladder allowing it to stretch and gain more capacity and also helps form a strong stream of urine when urinating.
In boys, the bladder neck reconstruction procedure may also involve a reconstruction of the urethra and penis, or it may be done in a separate operation at a later stage.
During the same operation, the ureters may be re-positioned within the bladder if they are not joining the bladder in the correct place. This can cause a condition called vesico-ureteric reflux (VUR) where the valves can fail, allowing urine to flow backwards from the bladder towards the kidney. The ureteric re-implantation operation involves disconnecting the ureters and re-attaching them in the correct place.
Are there any risks with these operations?
All surgery carries a small risk of bleeding during or after the operation. Every anaesthetic carries a risk of complications, but this is small. There is a small risk of infection, but your child may be given antibiotics as a precaution.
After the first operation to repair the bladder and abdominal wall, there is a risk that the wound will not heal properly and open up again. This can cause the bladder to move out of position. This happens more often if the area to be repaired is large, as the skin needs to stretch to cover it. If the wound opens up again, your child will need another operation to repair the bladder and abdominal wall. The surgeons may correct the pelvic bones during this operation as well.
There is also a risk of kidney damage in children with bladder exstrophy. The abnormal join between the ureters and bladder allows urine to flow backwards towards the kidneys. This is called vesicoureteric reflux (VUR). It can sometimes lead to a condition called hydronephrosis, where the kidneys become swollen. Both these conditions will be monitored closely throughout your child’s treatment.
What is the outlook for babies born with bladder exstrophy?
Children with bladder exstrophy repair need some further treatment later in childhood if they are having problems keeping dry.
If the bladder does not develop well, they many need an operation called bladder augmentation, which involves making the bladder larger, and therefore able to hold a larger volume of urine, using a section of intestine. These children then empty their bladder using a catheter to drain away the urine. The catheter can be inserted either into the urethra or a specially made channel called a Mitrofanoff channel.
The external genitalia of an individual born with bladder exstrophy or epispadias will always look different from others. In males the penis tends to be shorter and broader, but this does not usually cause any problems with their sex lives. Men born with bladder exstrophy have fathered children, although they may need fertility treatment. In many cases, sperm production is normal and sperm are healthy but ejaculating may be a problem.
Women born with bladder exstrophy have also had children, although pregnancy should be supervised by a specialist obstretrician and their babies are usually delivered by caesarean section.
Outlook for babies born with bladder exstrophy – Indian Scenario ?
In India, there may be problems with regular follow up due to far away distances from the hospital and lack of nursing care around the area where the child lives. Also in the event of the parents not willing for multiple surgeries, an option for a permanent urinary diversion (ureterosigmoidostomy) may be offered where the tubes from the kidneys are joined into a part of the large intestine (sigmoid colon). This would help to keep the child dry and he would then be passing urine and stools from the anal opening. These are complex surgeries and are carried out only after detailed discussion and interaction between the parents, patient families and the doctors.
Branchial Cyst & Branchial Sinus
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Branchial Cyst and Branchial Sinus
Branchial cysts are found on the side of the neck. They are the embryological remnants of the branchial clefts which normally form many structures in the head and neck region. They are sometimes also seen like a small punctum (hole) which is called a Branchial Sinus. The sinus may discharge a tiny drop of liquid. The branchial cyst or sinus may get infected leading to formation of an abscess at the site. Precise surgery and complete excision of the branchial cyst with its entire tract is curative for this lesion. The tract goes up in the neck and opens near the tonsillar area. Inadequately performed surgery may lead to recurrence. ●
 Left Branchial Sinus
Left Branchial Sinus
 Bilateral Branchial Sinus
Bilateral Branchial Sinus
 Right Branchial Sinus
Right Branchial Sinus

 Infected Branchial Cyst / Sinus
Infected Branchial Cyst / Sinus
GUJARATI
બ્રેન્કયલ સીસ્ટ અને બ્રેન્કયલ સાયનસ
બાળક માઁ ના ગર્ભમાં આકાર લેતું હોય ત્યારે ગળાના ભાગમાં માછલીના ગલેફા જેવા બ્રેન્કયલ ક્લેફ્ટ્સ વિકાસ પામતા હોય છે. આ બ્રેન્કયલ ક્લેફ્ટ્સમાથી મોઢું અને ગળાના વિવિધ અંગો આકાર લેતા હોય છે. આ બ્રેન્કયલ ક્લેફ્ટ્સના કોષ વિકાસ દરમિયાન બનાવવાના હોય તે સિવાયના બીજા અવયવ બનવાથી બ્રેન્કયલ સીસ્ટ અને બ્રેન્કયલ સાયનસ નામની જન્મ જાત ખોડ થાય છે. બ્રેન્કયલ સીસ્ટમાં ગળાના આગળના ભાગમાં ગાંઠ જાવા મળે છે અને બ્રેન્કયલ સાયનસમાં ગળાના આગળના ભાગમાં નાનું કાણું જાવા મળે છે. આ કાણામાંથી પ્રવાહી કે સફેદ પરુ નીકળતું હોય છે. બ્રેન્કયલ સીસ્ટમાં ઇન્ફેક્શન થવાથી પરૂ પણ થતું હોય છે. બ્રેન્કયલ સીસ્ટ તથા બ્રેન્કયલ સાયનસ માટે આૅપરેશનજ એક વિકલ્પ છે પરંતુ આૅપરેશન વખતે આ સીસ્ટ અને સાયનસ તેના મૂળભુત માર્ગ સાથે સંપૂર્ણપણે કાઢવામાં ન આવે તો ફરીથી બ્રેન્કયલ સીસ્ટ અથવા બ્રેન્કયલ સાયનસ થવાની શક્યતા રહેલી છે. આૅપરેશન બને તેટલું જલ્દી કરાવવું. બાળકની ઉમર/વજનનું આૅપરેશન માટે મહત્વ નથી. •
HINDI
ब्रेंकियल सीस्ट और ब्रेंकियल सायनस
गर्भस्त शिशु जब गर्भ में आकार प्राप्त कर रहा होता है तब उसके गले के भाग में मछली के गलफ़डो के समान ब्रेंकियल क्लेफ्ट विकसित होते हैं। इन्हीं ब्रेंकियल क्लेफ्ट से मुँह और गले के विविध अंग आकार प्राप्त करते हैं। यह ब्रेंकियल क्लेफ्ट की कोशिकाएं विकास के दौरान जो अंग बनाने चाहिए उन अंगों के अतिरिक्त अंग बनाते है तब ब्रेंकियल सीस्ट और ब्रेंकियाल सायनस जैसी बीमारियां होती है। ब्रेंकियल सीस्ट होने पर गले के अगले भाग में एक गांठ दिखाई देने लगती है और ब्रेंकियल सायनस होने पर गले के अगले भाग में एक छोटा सा छेद दिखायी देता है। इस छेद से प्रवाही अथवा सफेद रसी का स्त्राव होता है। ब्रेंकियल सीस्ट होने पर संक्रमण के कारण भी रसी हो सकती है। ब्रेंकियल सीस्ट और ब्रेंकियल सायनस दोनों का एक मात्र उपचार ऑपरेशन है। यदि ऑपरेशन के दौरान सीस्ट को उसके मूल मार्ग समेत न निकाला जाए तो ब्रेंकियल सीस्ट अथवा ब्रेंकियल सायनस के पुनः उभर आने की संभावना रहती है। ऑपरेशन जितना जल्दी हो सके उतना जल्दी करा लेना चाहिए। बालक की आयु या वजन से इसका कोई सरोकार नहीं होना चाहिए।•
Bed Wetting / Eneuresis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
BED WETTING
Wetting of the bed in sleep either during the day or night is common in infancy. However, a majority of these children get better with time and toilet training. If a child is more than 4 years and is continuing to wet, medical attention and treatment is necessary.
If the child wets both when awake and in sleep, then he definitely has a problem with his urinary control mechanism and all necessary investigations need to be done to find out the cause and treat the same. ●
GUJARATI
પથારીમાં પેશાબ (એન્યુરેસીસ)
નાની ઉંમરમાં બાળક ઉંઘમાં (રાત્રે અથવા દિવસે) પથારીમાં પેશાબ કરે એ સામાન્ય ગણાય છે. બાળકને યોગ્ય ટ્રેનીંગ આપવાથી મોટા ભાગનાં બાળકો ઉંમર વધતા સારા થઈ જાય છે.
જા બાળક ૪ વર્ષથી મોટું હોય અને ઉંઘમાં પેશાબ કરતું હોય તો ડાક્ટરની તપાસ અને ટ્રીટમેન્ટ જરૂરી છે.
બાળક જાગતાં અને ઉંઘતા જા પેશાબને કન્ટ્રોલ ન કરતું હોય અથવા કાયમ કપડાં ભીનાં કરતું હોય તો અચૂક કંન્ટ્રોલ સીસ્ટમની ખામી સમજી, જરૂરી બધી જ તપાસ કરાવી ટ્રીટમેન્ટ કરાવવી પડે છે. •
HINDI
बिस्तर गीला करना (एन्युरेसीस)
छोटी उम्र के बच्चे नींद में (रात्री अथवा दिन में) बिस्तर में पेशाब करे तो यह सामान्य बात है। उचित प्रशिक्षण देने से अधिकतर बच्चों में उम्र के साथ यह समस्या हल हो जाती है।
यदि बच्चे की आयु ४ वर्ष से अधिक हो और वह नींद में पेशाब करता है तो डॉक्टर से परामर्श और उपचार आवश्यक है।
बच्चा सोते-जागते यदि पेशाब पर नियंत्रण नहीं रख पाता है अथवा हमेशा कपडे गीले करता हो तो अवश्य ही उसकी मूत्र नियंत्रण प्रणाली में कोई दोष है। अतः सभी आवश्यक जांच कराकर उपचार की आवश्यकता होती है। •
Blood in Vomit (Hematemesis)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
BLOOD IN VOMIT (HEMATEMESIS)
Hematemesis (Blood in vomit) is a serious challenge for both the child and its doctor.
New born children: Blood in the vomit of a newborn child is commonly due to deficiency of vitamin K or secondary to swallowed maternal blood from a cracked nipple while breast feeding. This can also happen due to stress gastritis secondary to a stressful delivery.
1-2 years : Bleeding from the gums is swallowed by the child and is brought out in the vomit. Excessive use of pain killers or NSAID’s may cause gastritis and hematemesis. Food of a particular color or type may falsely raise the alarm of hematemesis.
Some children have severe gastroesophageal reflux (retrograde passage of stomach contents into the oesophagus). This may cause erosions in the inner lining of the oesophagus leading to hematemesis.
5-6 years: Gastroesophageal reflux and reflux oesophagitis can also cause hematemesis in this age. Another common cause for hematemesis in older children is oesophageal varices secondary to Portal Hypertension. This bleeding can be either bright red or coffee coloured. This is a serious problem and needs urgent and thorough treatment. These children need urgent hospitalization and endoscopy / open surgery are necessary for definitive treatment. ●
GUJARATI
ઉલ્ટીમાં લોહી પડવું
લોહીની ઉલ્ટી થવી એ બાળક અને ડાžટર માટે ગંભીર સમસ્યા છે.
નવજાત બાળકઃ આ ઉંમરમાં ઉલ્ટીમાં લોહી આવવાનું કારણ વિટામિન ‘કે’ ની ઉણપ,માતાનાં સ્તનમાં પડેલ ચીરામાંથી નીકળતું લોહી (ધાવણ દરમ્યાન પેટમાં જાય છે) અથવા તો સ્ટ્રેસફૂલ ડિલિવરીનું હોય છે.
એક-બે વર્ષઃ આ ઉંમરનાં બાળકોમાં દાંતના પેઢામાંથી નીકળતું લોહી ગળી જવાને કારણે અથવા કોઈ દુઃખાવા- તાવ માટેની દવા લેવાથી અથવા કલરવાળો ખોરાક ખાવાથી, લોહી રૂપે ઉલ્ટીમાં આવે છે. ઘણા બાળકોમાં હોજરી અને અન્નનળી વચ્ચેનો વાલ્વ લૂઝ હોવાથી હોજરીનું એસીડ અન્નનળીમાં ‘બેક મારે’ છે. આને ‘ગેસ્ટ્રોઈસોફેજિયલ રીફ્લક્ષ’ કહે છે. હોજરીના એસિડથી અન્નનળીમાં ઉઝરડા/ચાંદા પડવાના કારણે પણ ઉલ્ટીમાં લોહી આવે છે.
૫-૬ વર્ષ અને મોટી ઉંમરઃ આ બાળકોમાં વધુ પડતી લોહીની ઉલ્ટીનું કારણ અન્નનળીમાં ફૂલી ગયેલી લોહીની નળી (જેનું કારણ પોરટલ હાયપર ટેન્સન હોય છે) ફાટવાથી થાય છે. આ બીમારી સીરિયસ પ્રકારની હોય છે જેની યોગ્ય સારવાર કરાવવી પડે છે. આ જાતની લોહીની ઉલ્ટી કોફી કલરની અથવા લાલ કલરની હોય છે. મોટા બાળકોમાં પણ ગેસ્ટ્રોઈસોફેજિયલ રીફ્લક્ષના કારણે ઉલ્ટીમાં લોહી આવી શકે છે.
બાળકને તાત્કાલિક દાખલ કરી જરૂર પડે લોહી આપી એન્ડોસ્કોપી કરાવવી પડે છે. •
HINDI
उल्टी में खून
खून की उल्टी होना, बच्चा और डॉक्टर दोनों के लिए एक गंभीर चुनौतीपूर्ण समस्या है।
नवजात शिशुः आमतौर पर नवजात शिशु की उल्टी में खून आने का कारण विटामिन K की कमी या स्तनपान के दौरान माँ के स्तन से निकले खून को पीने से होती है। तनावपूर्ण डिलीवरी भी इसका कारण हो सकता है।
१ से २ वर्ष के बच्चों के दांत के पेढू से निकलने वाला खून गटकने के कारण बाद में उल्टी में निकलता है। दर्द से राहत के लिए अतिरिक्त मात्रा में दवाई लेने पर या किसी विशेष रंग वाला भोजन करने पर वह उल्टी में खून जैसा लगता है।
५ से ६ वर्ष और उससे अधिक आयु के बच्चों की उल्टी में खून की मात्रा अधिक होने का कारण आहारनली में फूली हुई खून की नली का टूट जाना है(पोरटल हायपर टेन्शन इसका कारण है)। यह उल्टी हल्के लाल रंग या कॉफी रंग की हो सकती है, जो कि काफी गंभीर बीमारी है और इसका तत्काल इलाज किये जाने की आवश्यकता है। ऐसे में बच्चे को तुरंत अस्पताल में भर्ती करके एन्डोस्कोपी करने की जरूरत है।•
Blood in Stool (Melena / Bleeding Per rectum)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
CHILD WITH BLEEDING PER RECTUM
Bleeding from any site in the body of a child can be a cause of concern for parents. When a child has bleeding from the anal canal, the following thing needs to be noted:
- Child’s age
- Amount of bleeding
- Colour of bleeding
- Any associated symptoms
GUJARATI
સંડાસમાં લોહી પડવું
દરેક મા-બાપ માટે તેનાં બાળકને કોઈ પણ જગ્યાએથી લોહીનું એક ટીપું પણ આવે તે ખૂબ જ ચિંતાનો વિષય બની જાય છે.
સંડાસમાં લોહી પડવાની તકલીફ આવે તો આટલું ધ્યાનમાં રાખોઃ
૧. બાળકની ઉંમર
૨. બ્લીડીંગનો રંગ
૩. બ્લીડીંગનું પ્રમાણ
૪. સાથે બીજી કોઈ તકલીફ
HINDI
मलद्वार से खून का बहना
बच्चे के शरीर के किसी भी हिस्से से खून की एक बूंद भी निकलने पर माता-पिता चिंतित हो जाते हैं। जब बच्चे के मलद्वार से खून बहता है तो नीचे दी गई बातों पर ध्यान देने की आवश्यकता है-
बच्चे की उम्र, बहते खून की मात्रा और उसका रंग। साथ ही उससे जुड़ी कोई समस्या।
Blood in Urine (Hematuria)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Hematuria
Hematuria is presence of red blood cells in the urine. Microscopic hematuria means blood is detected only with a microscope, while gross hematuria means urine appears red or like the colour of tea or cola.
Causes of hematuria?
- Abnormal structures in the urinary tract e.g. stones, tumors etc.
- Inherited diseases e.g. bleeding disorders, polycystic kidneys, sickle cell disorder etc.
- Mineral imbalances in the urine e.g. hypercalciuria
- Glomerulonephritis
- Idiopathic i.e. no specific cause can be found
Evaluation of Hematuria:
- An ultrasound of the urinary system
- Urine should be checked for protein and may be checked for calcium and creatinine.
- Blood tests to determine kidney function and other tests may be performed.
- If all tests are negative and urine remains blood stained, an endoscopic examination of the urinary tract may also be necessary.
Children who have microscopic hematuria with high blood pressure, abnormal blood tests, or high levels of protein in the urine may need to have a kidney biopsy. ●
GUJARATI
પેશાબમાં લોહી પડવું :
‘પેશાબમાં લોહી પડવું’ એ બાળક અને માતાપિતા માટે ખૂબ ચિંતાનો વિષય છે. કોઈ દવાની આડ અસર અથવા હીમોગ્લોબીન જવાથી પણ પેશાબ લોહી જેવો દેખાય છે.
મુખ્ય કારણો :
૧.કિડનીની ગાંઠ
૨. રક્તસ્ત્રાવ ડિસઓર્ડર
૩. પેશાબમાં ઇન્ફેક્શન
૪.નેફ્રાઈટીસ
૫. પેશાબમાં પથરી
મુખ્ય તપાસ:
ડાક્ટરી તપાસ કર્યા પછી જરૂરી લેબોરેટરી અને એક્સ-રે /સોનોગ્રાફી તપાસ કરાવવી પડે છે. ઘણીવાર દૂરબીનથી પેશાબની નળી અને કોથળીની તપાસ પણ કરવામાં આવે છે. •
HINDI
रक्तमेह (हीमेचुरीया)
मूत्र में लाल रक्त कणों की उपस्थिति को हीमेचुरीया कहते हैं। सामान्यतः गुर्दे खून को मूत्र में प्रवेश करने से रोकते हैं। हीमेचुरीया की स्थिति में, मूत्रमार्ग के फिल्टर अथवा अन्य अंग खून को रीस कर मूत्र में प्रवेश करने देते हैं। माईकोस्कोपिक हीमेचुरीया में केवल माईक्रोस्कोप के द्वारा ही खून के होने का पता चलता है, जबकि ग्ा्रॉस हिमेचुरीया में मूत्र रंग लाल अथवा चाय के रंग अथवा कोला जैसा दिखायी पड़ता है।
हीमेचुरीया के कारण :
मूत्रमार्ग में पथरी, गांठ आदि, जैसी असामान्य संरचनाओं का होना।
रक्तस्त्राव विकार, पॉलिसीस्टिक गुर्दे, सिकल सैल विकार जैसे रोग।
मूत्र में खनीजों का असंतुलन जैसे, हाईपरकॅल्कुरीया।
ग्लोमेरूलोनेफ्रीटिस
हीमेचुरीया का मूल्यांकन
मूत्र प्राणाली का अल्ट्रासाउंड। प्रोटीन, कैल्शीयम और क्रियटीनाइन के लिए मूत्र की जांच। गुर्दे के कार्यों की जांच के लिए खून की जांच और अन्य जांच। यदि सभी जांच का परिणाम नेगेटीव है और फिर भी मूत्र में खून पाया जाता है तो मूत्रमार्ग की एंडोस्कोपिक जांच करनी आवश्यक हो सकती है। माइक्रोस्कोपिक हीमेचुरीया वाले बच्चे की गुर्दे की बायोप्सी करने की आवश्यकता हो सकती है।•
Cystoscopy
How does the urinary system work?
The urinary system consists of the kidneys, the bladder, the ureters and the urethra. The kidneys filter the blood to remove waste products and form urine. The urine flows from the kidneys, down through the ureters to the bladder. From here it passes through another tube called the urethra to the outside when urinating (urinating).
What is a cystoscopy and why does my child need one?
A cystoscopy is a test that allows the doctor to look inside and around your child’s bladder using an endoscope (a tube containing a small camera and a light). The cystoscopy is carried out under a general anaesthetic (your child will be asleep) and lasts less than an hour.
A cystoscopy allows the doctors to find out what is causing your child’s problems without performing a larger operation. Your child may need a cystoscopy to find out if the bladder is infected, why there is blood in his or her urine or why he or she has poor bladder control.
Are there any alternatives to a cystoscopy?
A cystoscopy can give your doctor a fuller picture of your child’s condition. The only real alternative is an operation to examine the inside of the bladder, but this is avoided wherever possible. A cystscopy is quicker and has fewer lasting effects than an operation.
What does the procedure involve?
Your child will have this procedure under a general anaesthetic. This means he or she will be asleep and not feel any pain during the test.
Once your child is asleep, the doctor will insert the endoscope into your child’s urethra. From here, he or she will pass it into your child’s bladder. The doctor can now look at the inside of your child’s bladder, and also the tubes leading from it to the kidneys. Before your child wakes up, we will give him or her some pain relieving medications. This will reduce any discomfort in the hours following the test.
Right and Left ureteric orifice
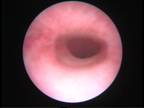
Urethra seen at cystoscopy
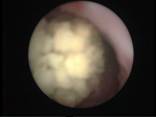
Stone seen in the ureter (urinary tube) at cystoureteroscopy
What happens afterwards?
Your child will come back to the ward to recover and will be able to go home once he or she has had something to drink and urinated.
You should encourage, but not force, him or her to drink plenty of fluids. He or she may feel a stinging sensation when passing urine but this will pass in a day or two. Try to avoid giving your child fruit juice as this is acidic and makes the stinging worse. It does not matter if he or she does not feel like eating for the first couple of days. There may also be a small amount of blood in your child’s urine, but this is also temporary.
When you get home, you should give your child regular pain relief as often as he or she seems to need it.
Cleft Lip
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a cleft lip repair?
Cleft lip repair is an operation to reconstruct the shape of the lip . If there is a cleft palate as well, then the front half (anterior) of the palate is also repaired. The earliest we do the operation is when babies are approximately three months of age. Babies are usually in hospital for about 3-4 days after the operation.
Bilateral Cleft Lip

Unilateral Cleft Lip

Unilateral Cleft Lip
What does the operation involve?
The operation involves joining the tissues that have not joined before birth. The surgeon may use an operating microscope to allow the small structures to be accurately joined. The operation usually takes from one to two hours, depending on the extent of the cleft.
What anaesthetic is used?
Your baby is given a general anaesthetic by an anaesthetist who specializes in giving anaesthetics to babies and children.
Are there any risks?
There is a small risk of infection following the operation, but your baby will be given an antibiotic injection during the operation, and continue to take antibiotics afterwards in the form of medicine. Every anaesthetic carries a risk of complications, but this is very small.
Your baby’s mouth will be sore after the operations, partly due to the operation itself, but also because the surgeon will need to move it about to repair the lip. The nurses will give pain relief medicine, so that he or she is not uncomfortable, particularly when feeding.
When can my baby feed?
We are happy for your baby to feed as soon as he or she is awake after the anaesthetic. The first feed may be difficult, partly because the lip is numb from the operation.
What happens afterwards?
When your baby has returned to the ward, he or she may be offered fluids that may be taken more easily from a spoon or syringe. If your baby is reluctant to drink it may be necessary to give extra fluid through the drip. The drip will be removed once he or she is drinking well again. It is important to give your baby some cooled, boiled water to drink after each feed and medicine to keep the inside of the mouth clean.
Soon after the operation there may be some bleeding but this usually stops quickly. Only very rarely will any further measures be necessary to stop the bleeding. Your child’s lip may look swollen and bruised for the first few days after the operation, but this will soon go down.
A course of antibiotics will be prescribed to reduce the risk of infection. You will need to continue giving this antibiotic medicine for a few days after leaving hospital to complete the course.
Unilateral Cleft Lip (After surgery)

Bilateral Cleft Lip (After Surgery)
When you get home…
By the time your child goes home he or she should be getting back to a normal feeding pattern. It is important to make sure your child is drinking enough. His or her lip may be swollen after the operation and the shape of his or her mouth may be different, but your child will soon adapt. You will be called to hospital for removal of the stitches on the 7th day following surgery.
GUJARATI
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું દર છસો એ એક બાળકમાં જાવામાં આવે છે. ઘણીવાર બાળકનો ફક્ત હોંઠ જ કપાયેલો હોય છે. જ્યારે ઘણીવાર હોંઠ, તાળવું અને પેઢું ત્રણે કપાયેલા હોય છે. માતા અથવા પિતામાં જા કપાયેલો હોંઠ અને ફાટેલું તાળવું હોય તો તેમનાં બાળકોમાં પણ આ ખોડ આવવાની શક્યતા બીજા બાળકો કરતાં વધારે રહેલ છે. ફાટેલું તાળવું હોવાથી બાળક સ્તનપાન નથી કરી શકતું તેથી આવા બાળકોને એક વિશેષ પ્રકારની બોટલ અથવા વાટકી અને ચમચીથી દૂધ પીવડાવવું જાઈએ. સ્તનપાન કરાવવાથી અથવા સાદી દૂધની બાટલીઓથી ઘણીવાર બાળકને આંતરાશ જઈ બાળકની જિંદગીને જાખમ પણ ઊંભું થતું હોય છે. કપાયેલા હોંઠનું આૅપરેશન ત્રણ મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાનું આૅપરેશન નવ થી બાર મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાના આૅપરેશન પછી બાળકોને ઘણીવાર વાંકાચૂકા દાંતની સારાવાર કરવાની જરૂર પડે છે. સ્પીચ થેરાપીની પણ જરૂર પડી શકે છે. •
HINDI
कटा होंठ और फटा तालु
कटा होंठ और फटा तालु हर ६०० में से एक बच्चे में देखा गया है। कई बार बालक का केवल होंठ ही कटा हुआ होता है। जबकि कभी-कभी होंठ, तालु और मसूड़े तीनों ही फटे हुए होते हैं। यदि माता या पिता में से किसी को भी कटे होंठ या फटे हुए तालु की समस्या है तो, उनके बच्चों में अन्य बच्चों के अपेक्षा यह दोष होने की संभावना अधिक रहती है। कटे होंठ या फटे तालु के साथ जन्मे शिशु को स्तनपान करने में तकलीफ होती है। अतः ऐसे बालक को विशेष प्रकार की बोतल या कटोरी-चम्मच से दूध पिलाना पड़ता है। सामान्य स्तनपान अथवा दूध की बोतल से दूध पिलाने पर कई बार दूध बच्चे के फेफडे में जाने की संभावना है और बच्चे की जान को खतरा पैदा कर सकता है। कटे होंठ का ऑपरेशन तीन महीने की उम्र में किया जाता है। फटे तालु का ऑपरेशन नौ से बारह महीने की आयु में किया जाता है। फटे तालु के कारण कई बार दांतों का उपचार अर्थात टेढ़े-मेढ़े दांतों के उपचार की आवश्यकता होती है। स्पीच थेरापी की भी आवश्यकता हो सकती है।•
Cleft Palate
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Cleft Palate
A cleft palate is a defect or gap in the roof of the mouth. It can involve some or all of the part of the palate.
A cleft palate can occur separately or together with a cleft lip.
What causes a cleft palate?
A cleft palate occurs during the first weeks of development in the womb. The palate is initially formed in two halves, lying either side of the tongue. Around the seventh or eight week the palate joins. This joining process may fail completely or stop at any point, resulting in a defect (cleft).
In any unaffected family, the chance of cleft lip / palate is one in 700. If one parent or child has a cleft, the chance of cleft lip / palate in future children is one in 25 to one in 40.
What are the signs and symptoms of cleft palate?
The main symptoms are the effect the condition has on hearing, feeding and later speech.
If a baby has an isolated cleft palate, they might have difficulty feeding properly because they can’t suck very well. The baby is unable to create a seal enabling them to create suction to get milk from the breast or bottle.
Some special bottles are used to help babies with isolated cleft palates feed but difficulty with feeding can mean the baby gains weight more slowly than is meant to happen over the first few months.
Other symptoms can include hearing problems as children with the condition are more at risk of glue ear. This can also lead to ear infections. As the palate plays an important role in speech it is important the cleft is repaired with surgery to reduce speech problems when the child is older.
How is a cleft palate normally diagnosed?
A cleft palate will be seen once a baby is born and is usually diagnosed at the time of the routine newborn baby check.
How is a cleft palate treated?
Treatment involves surgery. Most children require just one operation, but sometimes other operations may be needed to ensure the best possible speech outcome.
An operation to repair a cleft palate usually takes place when a child is between nine and 12 months of age. The operation involves joining the tissues that have not joined before birth.
What happens next?
In the vast majority of cases, surgery is very successful. Most babies born with a cleft palate will lead totally normal lives.
Children with a cleft palate will be monitored closely as they grow and develop. This will include their hearing and speech.
Most children are able to develop good speech and language skills following surgery. But sometimes a repaired cleft palate can make it difficult for a child to pronounce some sounds clearly. This may affect speech quality making it sound a bit ‘nasal’. A speech and language therapist will be able to help. However, most children will be able to speak normally.


 Cleft Palate
Cleft Palate

 After Repair
After Repair
GUJARATI
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું દર છસો એ એક બાળકમાં જાવામાં આવે છે. ઘણીવાર બાળકનો ફક્ત હોંઠ જ કપાયેલો હોય છે. જ્યારે ઘણીવાર હોંઠ, તાળવું અને પેઢું ત્રણે કપાયેલા હોય છે. માતા અથવા પિતામાં જા કપાયેલો હોંઠ અને ફાટેલું તાળવું હોય તો તેમનાં બાળકોમાં પણ આ ખોડ આવવાની શક્યતા બીજા બાળકો કરતાં વધારે રહેલ છે. ફાટેલું તાળવું હોવાથી બાળક સ્તનપાન નથી કરી શકતું તેથી આવા બાળકોને એક વિશેષ પ્રકારની બોટલ અથવા વાટકી અને ચમચીથી દૂધ પીવડાવવું જાઈએ. સ્તનપાન કરાવવાથી અથવા સાદી દૂધની બાટલીઓથી ઘણીવાર બાળકને આંતરાશ જઈ બાળકની જિંદગીને જાખમ પણ ઊંભું થતું હોય છે. કપાયેલા હોંઠનું આૅપરેશન ત્રણ મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાનું આૅપરેશન નવ થી બાર મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાના આૅપરેશન પછી બાળકોને ઘણીવાર વાંકાચૂકા દાંતની સારાવાર કરવાની જરૂર પડે છે. સ્પીચ થેરાપીની પણ જરૂર પડી શકે છે. •
HINDI
कटा होंठ और फटा तालु
कटा होंठ और फटा तालु हर ६०० में से एक बच्चे में देखा गया है। कई बार बालक का केवल होंठ ही कटा हुआ होता है। जबकि कभी-कभी होंठ, तालु और मसूड़े तीनों ही फटे हुए होते हैं। यदि माता या पिता में से किसी को भी कटे होंठ या फटे हुए तालु की समस्या है तो, उनके बच्चों में अन्य बच्चों के अपेक्षा यह दोष होने की संभावना अधिक रहती है। कटे होंठ या फटे तालु के साथ जन्मे शिशु को स्तनपान करने में तकलीफ होती है। अतः ऐसे बालक को विशेष प्रकार की बोतल या कटोरी-चम्मच से दूध पिलाना पड़ता है। सामान्य स्तनपान अथवा दूध की बोतल से दूध पिलाने पर कई बार दूध बच्चे के फेफडे में जाने की संभावना है और बच्चे की जान को खतरा पैदा कर सकता है। कटे होंठ का ऑपरेशन तीन महीने की उम्र में किया जाता है। फटे तालु का ऑपरेशन नौ से बारह महीने की आयु में किया जाता है। फटे तालु के कारण कई बार दांतों का उपचार अर्थात टेढ़े-मेढ़े दांतों के उपचार की आवश्यकता होती है। स्पीच थेरापी की भी आवश्यकता हो सकती है।•
Cystic Hygroma
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Cystic Hygroma: (Also read Lymphatic Malformations)
A cystic hygroma is a collection fluid-filled sacs known as cysts that result from a malformation in the lymphatic system.
A cystic hygroma is also known as a lymphatic malformation. The lymphatic system is a network of vessels within the body which form part of the immune system. Lymph nodes are located in the neck, armpits and groin areas and filter the lymph fluid.
What does a cystic hygroma look like?
Cystic hygromas can develop anywhere in the body, but are commonly found in the neck and armpits. It appears as a painless soft lump, which may be translucent.
What causes a cystic hygroma and can it be prevented?
A cystic hygroma forms when the lymph vessels fail to form correctly during the first few weeks of pregnancy. It cannot be prevented as it occurs so early in pregnancy, usually before the pregnancy is confirmed.
Nothing you did or did not do during pregnancy caused the cystic hygroma to develop. The exact cause of cystic hygromas is not clear. They occur in approximately one per cent of children and can affect children of any race and both boys and girls.
How is it diagnosed?
Cystic hygromas may be seen on scans during pregnancy. Many cystic hygromas are visible at birth or in early infancy, with almost all being diagnosed by the time a child is two years old. If the cystic hygroma is in a location where it may be interfering with other tissues and structures, scans such as ultrasound or magnetic resonance imaging (MRI) may be needed.
How can cystic hygroma be treated?
Sometimes cystic hygromas do not need to be treated. For babies, where the cystic hygroma is causing functional problems, the treatment options include surgical removal or injection sclerotherapy.
Surgical removal
Detailed scans will be needed to plan the operation, and it will only be carried out if the surgeon is confident that the operation will be beneficial. There will be an amount of scarring after the operation, as with all surgery.
Sclerotherapy
This is a procedure carried out under ultrasound guidance where a special medicine is injected into the cysts. The medicine mimics an infection, causing an inflammatory reaction, which makes the cystic hygroma shrink. It may take several sclerotherapy sessions for the cystic hygroma to be completely treated and even then, it might grow again.
Both surgical removal and sclerotherapy are carried out while the child is under a general anaesthetic. The doctors will discuss with you the treatment options suitable for your child. Some children may need both treatments.
Are there any risks with these treatment options?
Every procedure carries some risk of infection and bleeding. Your child will be given an antibiotic injection during their operation to reduce the risk of infection. Every anaesthetic carries a risk, but this is very small. Modern anaesthetics are very safe and your child’s anaesthetist is a very experienced doctor who is trained to deal with any complications.
With surgical removal and sclerotherapy, there is a small chance of damage to the structures surrounding the cystic hygroma. This is why detailed imaging scans are carried out before the operation. Even after the cystic hygroma has been removed or shrunk, there is a chance that it could return. Treatment can be repeated if needed.
What happens afterwards?
After the procedure, your child will return to the ward to wake up fully from the anaesthetic. The wound area will be covered with a dressing to protect it and a drain may be in place for the first few days then removed.
When you get home
• You should give your child pain relief medicines and a course of oral antibiotics.
• Your child will need to come back to the hospital for a check up appointment one to two weeks after the operation.
What is the outlook for children with a cystic hygroma?
The outlook is generally good, although the size and location of the cystic hygroma can influence long term outcomes. As explained above, cystic hygromas can come back after treatment, which would require another operation or sclerotherapy procedure.

 Cystic Hygromas in the neck
Cystic Hygromas in the neck
 Bilateral Cystic Hygromas in the neck
Bilateral Cystic Hygromas in the neck
GUJARATI
લિમ્ફેન્જયોમા
બાળકનું શરીર બે કોષમાંથી આકાર લેતું હોય છે. આમાંથી ચેતાઓ, ધમનીઓ અને લિમ્ફેટીક નામની ગ્રંથિઓના કોષ પણ છૂટા પડતા હોય છે. લિમ્ફેટીક નામની નળીઓ બનાવતા કોષ જે નોર્મલ કોષથી છુટા પડીને ગાંઠ બનાવે તેને લિમ્ફેન્જયોમા કહેવામાં આવે છે. હિમેન્જયોમા એટલે કે લોહીની નળીઓની ગાંઠથી વિપરીત લિમ્ફેન્જયોમા તેની જાતે ક્યારેય મટતું નથી તેના માટે આપરેશન જરૂરી હોય છે. આપરેશન દરમિયાન જા ગાંઠ સંપૂર્ણપણે ન નીકળે તો ભવિષ્યમાં આ રીતની ગાંઠ ફરી થવાની શક્યતા રહે છે. હિમેન્જયોમાની જેમ જ લિમ્ફેન્જયોમા પણ શરીરના કોઈ પણ બાહ્ય અથવાતો આંતરિક અવયવ કે વિભાગમાં થઈ શકે છે. સામાન્ય પણે તો તે ગળામાં અથવા બગલમાં વધુ જાવા મળે છે. •
Hindi
लिम्फेंजीयोमा
बालक का शरीर दो कोशिकाओं में से आकार प्राप्त करता है। इसमें नसें, धमनियाँ और लिम्फेटिक नामक ग्ा्रंथियों की कोशिकाएं अलग हो जाती है। लिम्फेटिक नामक नलिकाएं बनाने वाली कोशिकाएं सामान्य कोशिकाओं से अलग होकर जो गांठ बनाती है उसे लिम्फेंजीयोमा कहा जाता है। हिमेंजीयोमा अर्थात खून की नलिकाओं की गांठ के विपरीत लिम्फेंजीयोमा कभी भी अपने आप ठीक नहीं होता है और उसके लिए ऑपरेशन जरूरी हो जाता है। ऑपरेशन के दौरान यदि गांठ पूरी तरह से नहीं निकाल ली जाती तो भविष्य में गांठ फिर से उभर आने की संभावना बनी रहती है। हिमेंजीयोमा की भान्ति लिम्फेंजीयोमा भी शरीर के किसी भी बाहरी अथवा अंदरुनी भाग में हो सकता है। •
Choledochal Cyst
Choledochal Cysts in Children
A choledochal cyst is a rare congenital swelling of the hepatic or bile duct of the child’s liver.
- This is the tract that transports bile produced by the cells to the gallbladder and duodenum (the first part of the small intestine).
- These cysts can be intrahepatic, meaning that they occur in the part of the duct located inside of the liver.
- They can also be extrahepatic, meaning part of the bile duct that is located outside the liver.
What does the liver do?
The liver is located in the upper right-hand portion of the child’s abdominal cavity, beneath the diaphragm and on top of the stomach, right kidney and intestines. The liver consists of two main lobes, both of which are made up of thousands of lobules.These lobules are connected to small ducts that connect with larger ducts to ultimately form the hepatic duct. The hepatic duct transports bile produced by the liver cells to the gallbladder and duodenum, which helps to break down fats, preparing them for further digestion and absorption.
All of the blood leaving the stomach and intestines passes through the liver. The liver processes this blood and breaks down the nutrients and drugs in the blood into forms that are easier to use for the rest of the body.
What are the most common varieties of these cysts?
There are five basic types and they’re classified by where they appear.
- Type 1 — A cystic dilation of the extrahepatic bililary duct. This is the most common type, making up about half of all choledochal cysts.
- Type 2 — An abnormal pouch or sac opening from the duct.
- Type 3 —A cyst located within the duodenal wall.
- Type 4 — Swellings of both the intrahepatic and extrahepatic biliary tracts.
- Type 5 —Multiple intrahepatic cysts. This type of clustering of cysts is also known as Caroli’s disease and is the least common type.
How common are choledochal cysts?
- Choledochal cysts occur in between 1 and 100,000 and 1 in 150,000 people in Western countries but is much more common in Japan.
- They are three to eight times more common in females than males.
What causes choledochal cysts?
The cause of these cysts is unknown, but researchers believe that their formation is due to an abnormal connection between the pancreatic and hepatic ducts.
This abnormal connection leads to a reflux of pancreatic juice into the biliary tract, which could be responsible for cyst formation.
What are the symptoms of choledochal cysts?
The following symptoms are usually experienced by an older child whose earlier diagnosis of this congenital anomaly may have been missed.
- Abdominal pain in the right upper quadrant
- Jaundice
- Abdominal Mass
- Nausea
- Fever
- Pancreatitis
How are choledochal cysts diagnosed?
Choledochal cysts can be diagnosed prenatally (before birth) on an ultrasound.
After your baby is born, you or your child’s doctor may notice a right upper quadrant mass, with or without jaundice.
Your child will likely undergo a combination of the following tests to verify the diagnosis:
Computerized tomography scan (CT or CAT scan):
A CT scan shows detailed images of any part of your child’s biliary system.
Magnetic Resonance Cholangiopancreatography (MRCP):
Magnetic resonance cholangiopancreatography (MRCP) is a special type of magnetic resonance imaging (MRI) exam that produces detailed images of the hepatobiliary and pancreatic systems, including the liver, gallbladder, bile ducts, pancreas and pancreatic duct.
What is the treatment for choledochal cysts?
Surgery is the only feasible treatment for choledochal cyst. This involves removal of the choledochal cyst, followed by duct reconstruction using a piece of intestine. A number of possible approaches exist, depending on cyst location etc… Sometimes, the appendix is also used as a conduit for reconstruction of the biliary tree.
Surgery showing the gall bladder, choledochal cyst
The right and left hepatic ducts seen after removal of the choledochal cyst
Without surgery, there is an ongoing risk of other problems:
- Biliary obstruction and stone formation
- Infection of the ducts
- Jaundice
- Cirrhosis
- Perforation of the cyst
Another long-term concern is for malignant degeneration. Choledochal cysts are inflammatory in nature, which makes them at risk for becoming cancerous if left untreated.
Outcome for children with choledochal cysts after surgery
Children can lead a normal life after surgery for choledochal cysts. There are no issues related to digestion or their growing up. We normally follow then up after surgery with ultrasound scan after 6 months. If required blood tests are also carried out on follow up.
Constipation
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
CONSTIPATION
If a child passes hard stools, has pain while passing stools or has excessive abdominal distention or flatus (gas) formation, a doctor needs to be consulted. Treatment needs to be done only according to the doctor’s advice. It is not advisable to start the child on home remedies. If the child does not pass stools daily, but passes soft stools without any discomfort every 2 – 3 days, then it does not qualify as constipation.
If the child has constipation since birth and is associated with abdominal distention requiring suppositories or enemas, then it raises a suspicion of a disease of the large intestine called “Hirschsprung’s disease”. This needs consultation by a pediatric surgeon and may need investigations like a Barium enema or even a Rectal biopsy. ●

 Children with constipation causing abdominal distention
Children with constipation causing abdominal distention
કબજિયાત
કઠણ ઝાડો થવો અને તે કરવામાં બાળક ને દુઃખાવો થાય પેટ ફૂલી જાય, વધુ પડતો ગેસ થાય તો અચુક ડાક્ટરની સલાહ મુજબ તપાસ કરાવવી અને દવા લેવી. ઘરગથ્થુ દવાઓ ન કરવી. ઝાડો દરરોજ ન થતો હોય, પણ બાળક પોચો સંડાસ ૨-૩ દિવસે કરે તો તેને કબજિયાત ન ગણવી.
કબજિયાત લગભગ જન્મથી હોય અને બાળકનું પેટ ફૂલે, વારંવાર એનીમા અપાવવા પડે અને બાળકનું વજન ન વધે તો ચોક્કસ આ મોટા આંતરડાની જન્મજાત બીમારી હોઈ શકે. આને હર્ષસ્પૃન્ગ ડીઝીઝ કહે છે. આ માટે બાળકના સર્જનને બતાવી બાળકની વધુ તપાસ જેમ કે બેરિયમ એનીમા અથવા રેક્ટલ બાયપસી કરાવવી પડે છે. •
कब्ज
मल सख्त हो और उसे करने में बच्चे को दर्द हो, पेट फूल जाए, अत्यधिक गैस हो जाए तो डॉक्टर से अवश्य परामर्श करें और निर्देश के अनुसार जाँच कराएं और दवाइयां लेनी चाहिए। घरेलू दवाइयाँ नहीं लेनी चाहिए। मल हर रोज न होता हो, लेकिन बच्चा भले ही २-३ दिन में नरम संडास करे तो इसे कब्ज नहीं समझा जाना चाहिए। कब्ज जन्म से हो और बच्चे का पेट फूल जाए, बार-बार जुलाब देने की आवश्यकता पड़ती हो, और बच्चे का वजन न बढ़ रहा हो तो निसंदेह यह बड़ी आंत सम्बंधी जन्मजात बीमारी हो सकती है। इसे हर्षस्प्रंग रोग कहते हैं। बच्चे को सर्जन के पास ले जा कर अधिक जांच करानी पड़ती है जैसाकि बेरीयम एनिमा अथवा रेक्टल बायोप्सी।•
Duodenal Atresia
What is duodenal atresia?
Duodenal atresia means the duodenum (first part of the small intestine just beyond the stomach) is closed off rather than being a tube. This stops food and fluid passing from the stomach into the intestines.
How is it diagnosed?
Duodenal atresia can sometimes be discovered during pregnancy as it often shows up on antenatal ultrasound scanning. Some babies with this condition are born prematurely. Many babies appear well at birth but when they start to feed, they are sick and their vomit is green. An X-ray scan can confirm this diagnosis.
Duodenal atresia is a rare condition and occurs in about one in 10,000 births. It can be associated with other problems, so the doctors will examine your child closely to check if this is the case. One third of all children with duodenal atresia have Downs’ syndrome.
How is it treated?
Duodenal atresia is repaired in an operation under general anaesthetic (so your baby is deeply asleep), which lasts around 1 – ½ hours.
Are there any alternatives?
No. Duodenal atresia always requires treatment to allow your baby to feed.
What happens before the operation?
Your baby will need admission in hospital. To begin with, your child will be nursed in a warner and will have a naso-gastric (NG) tube passed through his or her nose into the stomach. This will drain off the contents of the stomach and stop your child from vomiting. It also releases any excess air from the stomach, which could make your child uncomfortable. He or she will also have an intravenous infusion (drip) of fluids and medicines.
What does the operation involve?
The surgeon will cut the blind end of the duodenum and connect it to the rest of the intestine. This provides a clear passage for food and fluid to travel from your child’s stomach to his or her intestine.
What happens afterwards?
Your baby will return to the ward to recover. All babies are closely monitored after the operation, and so your baby will be connected to monitors to check his or her breathing, heart rate and oxygen levels. He or she will also be given pain relief through the intravenous infusion (drip).
While your child’s intestines recover and start to work, he or she will be fed through a tube into his or her veins. This will gradually be replaced by breast or bottled milk, given through the naso-gastric tube when your child is able to tolerate this. As your baby recovers, you will be able to feed him or her from the breast or bottle.
You will be able to go home once your baby is feeding properly and gaining weight.
Disorders of Sexual Differentiation (DSD) / Intersex / Ambiguous Genitalia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
INTERSEX / DISORDERS OF SEXUAL DIFFERENTIATION / AMBIGUOUS GENITALIA
At conception, a fetus’s gender is already determined based on the 23rd pair of chromosomes it inherits from the parents. Females have two X chromosomes and males have an X and a Y chromosome. The sexual organs of males and females develop from the same fetal tissue. The main factor controlling the next step is male hormones. The presence of male sex hormones causes male organs to develop and the absence of male hormones causes female organs to develop. Without enough male hormones, a genetic male will develop ambiguous genitalia. Likewise, a genetic female will develop ambiguous genitalia if male hormones are present.
Characteristics of ambiguous genitalia in genetic females:
- An enlarged clitoris which appears to be a small penis
- A concealed vagina
Characteristics of ambiguous genitalia in genetic males:
- Microphallus
- Severe degree of hypospadias
- Bilateral undescended testes
What is the long-term outlook for a child with ambiguous genitalia?
Intersex is a major social challenge also. A complete and thorough investigation with in-depth counselling of the family is mandatory to manage these children. ●
GUJARATI
ઇન્ટરસેક્સ
બાળકનું લીંગ માતા-પિતામાંથી મળેલ સેક્સ ક્રોમોઝોમ્સ પર નિર્ભર છે. સ્ત્રીઓ માં XX ક્રોમોઝોમ્સ અને પુરૂષોમાં XY ક્રોમોઝોમ્સ હોય છે. બાળકની જનેન્દ્રિયો નો વિકાસ ગર્ભ દરમ્યાન થયેલ હોરમોન્સની અસરથી જ થાય છે. હોરમોન્સની થોડી પણ ચૂક/ વધુ અસર/ઓછી અસરના કારણે ઇન્ટરસેક્સના પ્રોબ્લેમ ઉભા થાય છે.
ઇન્ટરસેક્સ એક મોટી મેડીકલ અને સોશીયલ ચેલેન્જ છે. બાળકના જન્મ સમયે જા નીચે જણાવેલ ચિન્હો દેખાય તો ડાક્ટરે તેને બાબો/બેબી જાહેર કરવાની ઉતાવળ કરવી ના જાઈએ. આવા બાળકોને બાળકોના સર્જન દ્વારા તપાસ અને રીપોર્ટ કરાવવા જરૂરી હોય છે. આજના જમાનામાં એન્ડોસ્કોપી અને લેપ્રોસ્કોપી આ બાળકોના લિંગના સચોટ નિદાન અને તેની યોગ્ય સારવાર માટે ખૂબ જ મદદરૂપ થાય છે.
ઇન્ટરસેક્સના ચિન્હો :
(૧) બાળકીઓ (XX) માં ઇન્ટરસેક્સના ચિન્હો :
– યોનિમાર્ગની ઉપર ભગ્નનો આકાર લિંગ જેવો હોવો
– યોનિમાર્ગ બંદ હોવો/ન હોવો
(૨) બાબાઓ (XY) માં ઇન્ટરસ્ક્સના ચિન્હો :
– બાળકી જેવી જનેન્દ્રિયો હોવી.
– પેશાબનો માર્ગ લિંગની નીચે/પાછળ હોવો.
– લિંગ નો ભાગ ખૂબ જ નાનો હોવો અને પેશાબનો રસ્તો ખોટી જગ્યાએ હોવો.
– વૃષણની બંન્ને ગોળી વૃષણ કોથળીમાં ન હોવી. •
HINDI
इंटरसैक्स/यौन भेदभाव का विकार/अस्पष्ट जननांगता
गर्भधारण के समय से ही, अपने माता-पिता से विरासत में प्राप्त २३वें गुणसूत्र के आधार पर भ्ा्रूण का लिंग निश्चित हो जाता है। कन्या में दो ङ्ग गुणसूत्र होते हैं और पुरूष बालक में एक ङ्ग और एक Y गुणसूत्र होता है। पुरूषों और महिलाओं के जनन अंगों का विकास एक ही भ्ा्रूण मांस-तंतु से होता है। अगले चरण को नियंत्रित करनेवाले मुख्य कारक पुरूष हार्मोन है। पुरूष अंगों के विकास का कारण पुरूष जनन हार्मोन की उपस्थिति है और इनकी अनुपस्थिति महिला जनन अंग विकसित करता है। अपर्याप्त पुरूष हार्मोन के कारण आनुवांशिक पुरूष में अस्पष्ट जननांगता का विकास होता है। इसी प्रकार, पुरूष हार्मोन की उपस्थिति के कारण आनुवांशिक महिला में अस्पष्ट जननांगता का विकास होता है।
आनुवांशिक महिलाओं में अस्पष्ट जननांगता के लक्षणः
१. बढ़ा हुआ भगशेफ (Clitoris), जो लघु शिश्न (Penis) सा प्रतीत होता है।
२. छुपा योनि।
आनुवांशिक पुरूषों में अस्पष्ट जननांगता के लक्षणः
१. गैर पहचान योग्य (अथवा अस्पष्ट) पुरूष गुप्तांग।
२. अनुपस्थित जननपिंड के साथ गंभीर अधोमूत्रमार्गता।
३. एक बहुत ही छोटा शिश्न जिसका मूत्रमार्ग अंडकोश की थैली के पास खुला हो।
४. दोनों ही अंडकोशों का अनुपस्थित होना और अंडकोश की थैली का अविकसित होना।
इंटरसैक्स एक प्रमुख सामाजिक चुनौती भी है। ऐसे बच्चों के उपचार के लिए परिवारवाले से बारीकी से परामर्श करने के साथ गहन जांच अनिवार्य है। कई बार, एक निश्चित निदान पर पहुंचने के लिए बहुविशिष्ट दृष्टिकोण आवश्यक होता है। अस्पष्ट जननांगता के साथ जन्मे कुछ बच्चों के जनन अंग सामान्य होते हैं जो उन्हें प्रजननक्षम जीवन व्यापन करने की अनुमति प्रदान करते हैं। अन्य कुछ प्रजननक्षम नहीं होते हैं अथवा वे गर्भधारण करने में कठिनाई का अनुभव करते हैं। कभी-कभार बाद के जीवनकाल में उनके जननअंग में गांठ हो जाने का खतरा होता है।•
Exomphalos
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Exomphalos is a type of abdominal wall defect. It occurs when a child’s abdomen does not develop fully while in the womb.
Early in all pregnancies, the intestine develops inside the umbilical cord and then usually moves inside the abdomen a few weeks later. In exomphalos, the intestines and sometimes other organs such as the liver, remain inside the umbilical cord but outside the abdomen.
What causes exomphalos?
We do not know what causes exomphalos. It affects two in every 5,000 children born each year. Exomphalos can be associated with other problems, but the doctors will examine your child closely to check if this is the case.
What are the signs and symptoms of exomphalos?
Exomphalos is immediately recognizable because the child’s intestines are outside the body and covered in a membrane. The size of the bulging membrane containing the intestines and other organs varies from a small protrusion to quite a large lump.
There are two types of exompahlos:
Exomphalos minor where the opening is less than 4cm and only containing the intestine, and Exomphalos major where the opening is greater than 4cm and/or with the liver inside the cord.
How is exomphalos diagnosed?
In many cases, exomphalos is visible on pre-natal ultrasound scanning, which is useful because it gives time for discussions and planning for when and where to give birth.
How is exomphalos treated?
Exomphalos is a serious condition so needs prompt treatment soon after birth.
Depending on the size of the exomphalos, your child may need to have it repaired in one operation or in several stages. If the exomphalos is small and the child is stable, they may have an operation soon after admission to the hospital, where the surgeon replaces the contents back inside the abdomen and closes up the base of the umbilical cord.
If the exomphalos is larger, contains the liver and/or your child needs to be stabilised, doctors may place a silo or pouch over the intestines, which is closed over a period of days to weeks, to allow your child to grow so that there is room inside the abdomen.
What does the operation involve?
If your child is having a one-stage repair under general anaesthetic, the surgeons will replace your child’s entire intestine into the abdominal space and close up the hole at the base of the umbilical cord.
Sometimes, they may need to use a ‘patch’ of material if the hole is quite large. They will cover the area with a dressing to protect the wound while it heals.
In a staged repair, there is too much intestine outside of the abdomen to put back without causing further damage or the space inside the abdomen is too tight. While your child is under general anaesthetic, the surgeon will make a mesh sac and put it over the intestine which keeps it contained and protected.
This sac is then suspended above your child so that gravity gradually moves the intestines back inside the abdomen. It is tightened regularly until all the intestine is inside the abdomen, which usually takes a few days to a few weeks. Your child will then have an operation under general anaesthetic to close up the skin and muscles.
Are there any risks with the operation?
All surgery carries a small risk of bleeding during or after the operation. During the operation, the surgeon will minimise any bleeding by sealing off the blood vessels affected. There is a very small chance that nearby structures in the abdomen could be damaged during surgery but this is a very rare occurrence.
Every anaesthetic carries a risk of complications, but this is very small. Your child’s anaesthetist is a very experienced doctor who is trained to deal with any complications.
It can take a while after the operation for the intestine to start working properly so your child may need to be fed intravenously using total parenteral nutrition (TPN) for a while. Some babies with exomphalos have breathing problems which may require more support for a longer period.
Are there any alternatives to the operation?
In some scenarios, the child may be treated with particular chemicals / ointments in order to make the membrane covering the intestine hard. The surgery may hence be delayed by a few weeks. Ultimately, the condition needs to be treated to allow your child to grow and develop.
What happens after the operation?
Your baby will come back to recover either in the intensive care unit .All babies are closely monitored after the operation, and so your baby will be connected to monitors to check their breathing, heart rate and oxygen levels. If your child needs help with breathing, they will be connected to a ventilator. They will also be given pain relief through the intravenous infusion (drip).
What happens next?
The outlook for children born with exomphalos varies depending on the size of the defect and any other problems. Many children have grown up to live normal lives.
Children who have had aexomphalos repair may develop hernias in the years after the operation. This is because the abdomen has fewer muscles than usual.
GUJARATI
એક્ઝોમ્ફેલોસ
એક્ઝોમ્ફેલોસ ૫૦૦૦ એ ફક્ત ૨ બાળકોમાં જાવા મળતી એક ગંભીર જન્મજાત ખોડ છે.
સામાન્ય રીતે ગર્ભમાંના બાળકનાં આંતરડા તેના પેટની બહાર આકાર લઈને નાળના માર્ગેથી પેટની અંદર જતાં હોય છે. આ ખોડમાં બાળકના પેટની દીવાલ બરાબર ન બનતા તેના આંતરડા અને કોઈક વખતે બાળકનું લીવર પેટની બહાર નાળની અંદર ફસાયેલા રહેતા હોય છે.
આ ખોડ બાળકને જાતાં જ ખબર પડી જાય છે. બાળકના આંતરડા પેટની બહાર પારદર્શક પડથી ઢંકાયેલા દેખાય છે. બાળકને તાત્કાલિક સારવારની જરૂર પડે છે. સારવાર અર્થે મોકલતા પહેલાં બાળકનાં આંતરડાને ચોખ્ખા સલાઈનવાળા કાપડથી ઢાંકી દેવું જાઈએ. આ બાળકોમાં ઓપરેશનની જરૂર પડતી હોય છે. આૅપરેશન એક સ્ટેજ અથવા બે સ્ટેજમાં કરવામાં આવે છે. જા બાળક આૅપરેશન ખમી શકવાની પરિસ્થિતિમાં ન હોય તો અમુક કેમિકલ/દવાઓ લગાવી આંતરડાના ઉપરના પડને કડક કરવામાં આવે છે જેથી બાળકને ઇન્ફેક્શન ન લાગે. આ બાદ યોગ્ય સમયે આૅપરેશન કરી પેટની દીવાલ બનાવવામાં આવે છે. •
HINDI
एक्जोमफेलस (नाभि सम्बंधी जन्मनात हर्निया)
एक्ज़ोमफेलस पेट की दीवार का एक दोष है। हर ५००० में २ बच्चों को यह प्रभावित करता है। गर्भाधान के कुछ ही सप्ताह बाद, गर्भनाल के भीतर आंतों का विकास होता है। एक्ज़ोमफेलस में आंतें और कभी-कभी अन्य अंग जैसाकि जीगर गर्भनाल के भीतर परंतु उदर के बाहर रह जाते हैं। एक्ज़ोमफेलस के बारे में तुरंत पता लग जाता है क्योंकि बच्चे की आंते शरीर के बाहर होती है और इनपर एक आवरण होता है। जन्म से पहले ही अल्ट्रासाउंड के द्वारा एक्ज़ोमफेलस का पता चल जाता है। एक्ज़ोमफेलस एक गंभीर परिस्थिति है और जन्म के तुरंत बाद इसका उपचार किया जाना आवश्यक होता है।
प्रसूति करानेवाले फिजीशीयन को सावधानीपूर्वक इन्हें (आंतो को) पानी में भीगोए जंतुरहित कपड़े से ढंक देना चाहिए और बच्चे को बालविशेषज्ञ के पास स्थानांतरित करना चाहिए।
एक्ज़ोमफेलस के आकार के आधार पर, एक ऑपरेशन अथवा अनेक स्तरीय ऑपरेशन के द्वारा इसे ठीक करने की आवश्यकता हो सकती है। यदि एक्ज़ोमफेलस अधिक बड़ा है, उसमें जीगर शामिल है और/अथवा बच्चे को स्थायीकरण की आवश्यकता हो, तो सर्जन को आंतों के ऊपर कुशूल अथवा थैली रख देनी चाहिए, ताकि बच्चा बढ़ सके और उदर के भीतर अधिक जगह बन सके। कुछ मामलों में, उपचार विशेष रसायनों/मलमों के द्वारा किया जाना चाहिए जिससे कि आंतों के ऊपर का आवरण सख्त हो जाए। तदनुसार, सर्जरी को कुछ हफ्तों के लिए विलम्बित किया जाना चाहिए। एक्ज़ोमफेलस के साथ जन्मे बच्चे का दृष्टिकोण विसंगति के आकर और अन्य समस्याओं के अनुसार भिन्न हो सकता है। कई बच्चे बड़े होकर सामान्य जीवन व्यतीत करते हैं। •
Empyema
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Empyema is a condition where pus collects in the pleural space (space outside the lung and inside the chest wall), often as a complication of pneumonia.
The lungs and inside of the chest cavity have a smooth covering called the pleura that lets the lungs expand without rubbing on the inside of the chest. The two layers of pleura are usually in close contact with only a small space in between (pleural space) filled with a small amount of pleural fluid acting as lubrication.
This complication of pneumonia usually occurs in three stages. Initially, clear fluid collects up in the pleural space which can then become infected. The fluid thickens and can affect the pleura, causing sections to ‘stick together’ eventually forming ’pockets’– this is called empyema. The infected fluid stops the lungs inflating completely, causing increasing breathing difficulties.
What causes empyema?
Empyema usually develops following pneumonia – various bacteria can cause pneumonia (most common ones are Staphylococcus pneumoniae and Staphylococcus aureus). Empyema seems to becoming more common, particularly in young children aged one to four years. It tends to occur during winter and spring season, when pneumonia and other chest infections are more common. Sometimes tuberculosis may also be a cause of empyema.
What are the signs and symptoms of empyema?
Empyema is usually suspected when a severe bout of pneumonia does not improve with treatment. Children usually show symptoms of being generally unwell with a high temperature. They may find breathing harder than normal, struggling to catch a breath. Their heart rate may also be higher than usual. Some children may describe pain in their chest when breathing.
How is empyema diagnosed?
If empyema is suspected, a chest x-ray may be the first test suggested to confirm or rule out the diagnosis. Chest x-rays will show white areas that suggest fluid. An ultrasound of the chest is more precise at showing the amount of fluid and the exact location and whether there are any pockets. In some cases, the doctor may also ask for a CT Scan of the chest to make sure that the child does not have any structural problems with the lung like a lung abscess which may have caused an empyema.
How is empyema treated?
Empyema previously used to be treated by placing a chest drain in the chest and with intravenous antibiotics as well as medicines to stop the pus clumping together.
However, nowadays with the advance of minimally invasive surgery, Empyema is treated with VATS (Video assisted thoracoscopic surgery) wherein a telescope is inserted into the chest cavity and all the pus is removed under vision. The pus pockets are broken down and washed with antiseptic liquids and a chest drain is placed. The surgery is completed with 2 or 3 5 mm instruments rather than placing a big cut on the chest. Also as the procedure is done undervision, the doctor is sure that the pus has been completely cleared and the child also recovers early.
What happens next?
The outlook for children with empyema is usually good once it has been diagnosed and treated promptly. Long term lung damage is rare. With thoracoscopy, the recovery is just in a few days. Once the lung is completely expanded as seen on follow up x-ray, the chest tube is removed and the child is sent home on oral medications. They will also need regular follow up clinic appointments, usually involving a chest x-ray, to check that the pleura is healing properly without any problems.
 Early Stage of Empyema (At Thoracoscopy)
Early Stage of Empyema (At Thoracoscopy)

 Late Stage of Empyema (At Thoracoscopy)
Late Stage of Empyema (At Thoracoscopy)
 Lungs seen after clearance of Empyema (At Thorascopy)
Lungs seen after clearance of Empyema (At Thorascopy)
 Late Stage Empyema (Needing open surgery)
Late Stage Empyema (Needing open surgery)
GUJARATI
એમપાઈમા
એમપાઇમા ન્યુમોનિયાને કારણે ફેફસાંની બહારના ભાગમાં થતાં પાણી અને પરૂના ભરાવાને કહેવામાં આવે છે. સામાન્ય રીતે ન્યુમોનિયા દવાઓથી સારું થઈ જાય છે પરંતુ બાળકમાં જ્યારે રોગ પ્રતીકારક શક્તિ ઓછી હોય અથવા જંતુઓનો પ્રભાવ વધારે હોય તો ન્યુમોનિયાના એક કામ્પ્લીકેશન તરીકે છાતીમાં ફેફસાંના બહારના ભાગમાં પરૂ અને પાણીનો ભરાવો થાય છે જેને એમપાઇમા કહેવામાં આવે છે. એમપાઇમામાં ફેફસું દબાણમાં આવે જેથી બાળકને શ્વાસ લેવામાં તકલીફ પડે છે અને તાવ પણ ખૂબ જ આવે. પહેલા એમપાઇમાની સારવાર માટે બે પાંસળીઓ વચ્ચે નળી મૂકી પરૂ આપોઆપ બહાર નીકળે અને સુકાય તેની રાહ જાવી પડતી હતી. આ માટે બાળકને ઘણીવાર અઠવાડિયાઓ અને મહિનાઓ સુધી હોસ્પિટલ માં રહેવું પડતું. હવે આધુનિક સાધનો અને લેપ્રોસ્કોપીના આગમન પછી બે પાંસળી વચ્ચે દુરબીન મૂકીને ફેફસાંની બહાર આવેલું બધૂજ પરૂ અને પ્રવાહી સંપૂર્ણપણે સાફ કરવામાં આવે છે. ફેફસું સામાન્ય રીતે ફૂલી જાય તેની ચોકસાઈ કરીને આૅપરેશન થઈ શકે છે. આ આૅપરેશન પછી બાળકને ત્રણ થી પાંચ દિવસ હોસ્પિટલ માં રહેવું પડે છે અને બાળક સંપૂર્ણપણે સ્વસ્થ અને સારુ થઈ જાય છે. આ દુરબીનની ટેક્નીકને થોરેકોસ્કોપી કહે છે. •
HINDI
एमपाइमा (छाती में रसी)
न्युमोनिया के कारण फेफड़ों के बाहरी भाग में उत्पन्न होने वाले पानी और रसी के जमाव को एमपाइमा कहते हैं। सामान्यतः न्युमोनीया दवाइयों से ठीक हो जाता है। लेकिन बच्चे की रोग प्रतिकारक शक्ति कमजोर हो अथवा किटाणुओं का प्रभाव अधिक हो, तो न्युमोनिया की जटीलता के कारण छाती के भीतर फेफड़ों के बाहरी भाग में पानी और मवाद का जमाव हो जाता है, जिसे एमपाइमा कहा जाता है। एमपाइमा के कारण बच्चे के फेफड़ों पर दबाव पड़ता है और तेज़ बुखार भी हो सकता है। पूर्व काल में एमपाइमा के उपचार हेतु दो पसलियों के बीच एक नली रख कर मवाद के अपनेआप सुख जाने की अथवा बाहर रीस जाने की प्रतीक्षा की जाती थी। इसके लिए बच्चे को हफ्तों और कई बार तो महीनों तक अस्पताल में भर्ती होना पड़ता था। लेकिन वर्तमान में आधुनिक उपकरणों के चलते और लेप्रोस्कोपी तकनीक के आने से दो पसलियों के बीच दूरबीन लगाकर फेफड़ों के बाहर का मवाद और प्रवाही को पूरी तरह साफ कर दिया जाता है। इस ऑपरेशन के पश्चात बच्चे को तीन से पाँच दिन अस्पताल में रहना पड़ता है जिसके बाद बच्चा सम्पूर्ण स्वस्थ हो जाता है। दूरबीन की इस टेकनीक को थोरेकोस्कोपी कहा जाता है। •
Epistaxis (Nose Bleed)
Nose bleeds are when the small fragile blood vessels in the nose break. This will cause the nose to bleed. It is a common condition, especially in young children. Children who have frequent nosebleeds should be checked for underlying conditions by a doctor.
What causes nose bleeds?
Nosebleeds are pretty common, especially in young children. This is because the blood vessels in the nasal lining are close to the surface and quite fragile. They can rupture easily.
A bump or bang on the nose can often result in a nosebleed. Young children often play very physical games, whether it’s rushing around on the playground at nursery or school or tumbling about at home. Bumps on the nose can be pretty common.
If a child picks their nose or blows it too vigorously, this can also start a nosebleed.
Sometimes even a violent sneeze can damage the nasal blood vessels, and trigger a nose bleed.
While nosebleeds are rarely dangerous, very occasionally, a nosebleed can indicate a more serious underlying problem like a head injury.
What are the signs and symptoms of nose bleeds?
If a child has a nosebleed after suffering from a bump on the head, it’s important to look carefully for other signs that might indicate an underlying injury.
If the child has any of the following symptoms emergency medical advice should be sought:
• confusion
• drowsiness
• nausea and vomiting
• losing fluid through their nose that is thin and watery
How are nose bleeds treated?
If a child has a nose bleed, the recommended course of action is:
• Ask the child to sit down with their head tilted forward.
• Get them to breathe through their mouth.
• Put a bowl under the nose and give them tissues or a cloth.
• Ask them to pinch the front, soft part of their nose for 10 minutes – or pinch it for them if it is a young child.
• If tolerated, apply an ice pack to the affected area
• After 10 minutes, release the pressure – if the bleeding has not stopped, reapply the pressure for up to two further periods of 10 minutes.
• Once the bleeding stops gently clean the area.
Do not tilt the child’s head backwards. This will not stop the bleeding and can cause blood to trickle down their throat. This can make them vomit or choke and affect their ability to breathe.
When to ask for medical help about nose bleeds ?
If the bleeding does not stop after 30 minutes, it’s best to take the child down to your local hospital or seek medical advise.
Frequent nosebleeds
Some children do seem more prone than others to frequent nosebleeds. If a child does seem to suffer from them more than twice a week, it’s advisable to see a doctor.
It’s important in the first instance to rule out an underlying bleeding disorder.The doctor may recommend blood tests.
Another more common explanation for frequent nosebleeds is that the child may have picked their nose causing blood vessels in the septum, the cartilage which divides the nostrils, to bleed.
The doctor can also check for any signs of infection. If there is any infection, the doctor will probably prescribe a course of ointment with antibiotic and anti-inflammatory properties.
A child who has a deviated septum is more likely to suffer from nosebleeds. A deviated septum means that the septum is slightly bent, usually as a result of injury (for instance a sports injury or an injury sustained during birth). The deviated septum causes abnormal airflow through the nose which causes the lining of the septum to dry out and bleed easily.
What happens next?
Most children, even those who suffer from frequent nosebleeds, tend to outgrow it. Nosebleeds can also happen in adult life but it is less common.
Encephalocele
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
ENCEPHALOCELE
Encephalocele is a neural tube defect which is characterized by a sac like protrusion behind the head. They may also present in the front of the skull between the forehead and nose.
This is formed by protrusion of the brain and its covering membranes through an opening in the skull. These swellings may be small or massive. The child may also have other problems like hydrocephalus, quadriplegia, microcephaly, vision problems, seizures, mental and growth retardation.
Encephaloceles can also be picked up on an antenatal ultrasound scan.
Treatment of encephalocele is surgery and should be performed immediately after birth or latest during early infancy. Recovery is difficult to predict prior to surgery and depends on the location and type of brain tissue involved.
The child will need help of specialists following surgery to focus on both mental and physical development.
Folic acid when taken before pregnancy and early in gestation has been shown to help prevent such defects. ●
GUJARATI
એનકીફેલોસીલ (માથાની પાછળની ગાંઠ)
આ એક મગજની ગાંઠ છે. ખોપરીની પાછળનાં ભાગમાં કાણું હોવાનાં લીધે બાળકનાં માથાની પાછળનાં ભાગમાં આ ગાંઠ દેખાય છે. આ ગાંઠની સાઈઝ નાની અથવા ઘણી મોટી હોય છે. ઘણી વાર બાળકમાં પોતાના માથા કરતાં પણ આ ગાંઠ મોટી હોય છે.
આ જાતની ગાંઠ બાળક માઁનાં પેટમાં હોય ત્યારે માતાની સોનોગ્રાફીમાં જ ખબર પડે છે. આવા બાળકો અચૂક થોડી અથવા મોટી માનસિક વિકાસની ખામી અનુભવે છે. પેનલ આૅફ ડાક્ટર્સ જા નક્કી કરે તો આવા બાળકનું ચાર માસ પહેલાં અબોર્શન કરાવું સારું.
જા આ સમય ચૂકી જાય તો આ જન્મજાત ખોડનું આૅપરેશન જરૂર થઈ શકે છે અને તે જન્મનાં પહેલાં સપ્તાહમાં કરવું જાઈએે જેથી બાળકને માતાની કાળજી સારી રીતે મળી શકે .
બાળકના મગજનો વિકાસ બાળક જેમ જેમ મોટું થાય તેમ તપાસ દ્વારા જાણવા મળે છે.
પ્રેગ્નન્સી શરૂ થતાં પહેલાં જા ફાલીક એસિડની ગોળી લેવામાં આવે તો આવી ખોડનું પ્રમાણ ઓછું જાવામા આવે છે. •
HINDI
सिर के पीछे की गांठ (अेनकीफेलोसील)
यह मस्तिष्क की एक गांठ है, जो खोपड़ी के पीछे के भाग में छेद होने के कारण बच्चे के सिर के पीछे के हिस्से में गांठ के रूप में उभरती है। इसका आकार छोटा या बड़ा हो सकता है। अक्सर यह गांठ बच्चे के सिर से भी बड़ी होती है।
गर्भावस्था में माँ की सोनोग्राफी से इस गांठ के बारे में पता चलता है। अक्सर इस तकलीफ वाले बच्चों में कम या थोडी बहुत मानसिक विकास की कमी पायी जाती है। सिर के पीछे की गांठ को सर्जरी से ठीक किया जा सकता है। डॉक्टर से परामर्श लेकर चार महीने से पहले यह ऑपरेशन कराना बेहतर है। सर्जरी के बाद बच्चे के शारीरिक और मानसिक विकास के लिए डॉक्टर से सलाह लेकर नियमित जाँच कराना आावश्यक है।
गर्भावस्था में फोलिक एसिड की दवाई लेने से इस प्रकार के जन्मजात दोष से बचा जा सकता है। •
Enuresis / Bed Wetting
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
BED WETTING
Wetting of the bed in sleep either during the day or night is common in infancy. However, a majority of these children get better with time and toilet training. If a child is more than 4 years and is continuing to wet, medical attention and treatment is necessary.
If the child wets both when awake and in sleep, then he definitely has a problem with his urinary control mechanism and all necessary investigations need to be done to find out the cause and treat the same. ●
GUJARATI
પથારીમાં પેશાબ (એન્યુરેસીસ)
નાની ઉંમરમાં બાળક ઉંઘમાં (રાત્રે અથવા દિવસે) પથારીમાં પેશાબ કરે એ સામાન્ય ગણાય છે. બાળકને યોગ્ય ટ્રેનીંગ આપવાથી મોટા ભાગનાં બાળકો ઉંમર વધતા સારા થઈ જાય છે.
જા બાળક ૪ વર્ષથી મોટું હોય અને ઉંઘમાં પેશાબ કરતું હોય તો ડાક્ટરની તપાસ અને ટ્રીટમેન્ટ જરૂરી છે.
બાળક જાગતાં અને ઉંઘતા જા પેશાબને કન્ટ્રોલ ન કરતું હોય અથવા કાયમ કપડાં ભીનાં કરતું હોય તો અચૂક કંન્ટ્રોલ સીસ્ટમની ખામી સમજી, જરૂરી બધી જ તપાસ કરાવી ટ્રીટમેન્ટ કરાવવી પડે છે. •
HINDI
बिस्तर गीला करना (एन्युरेसीस)
छोटी उम्र के बच्चे नींद में (रात्री अथवा दिन में) बिस्तर में पेशाब करे तो यह सामान्य बात है। उचित प्रशिक्षण देने से अधिकतर बच्चों में उम्र के साथ यह समस्या हल हो जाती है।
यदि बच्चे की आयु ४ वर्ष से अधिक हो और वह नींद में पेशाब करता है तो डॉक्टर से परामर्श और उपचार आवश्यक है।
बच्चा सोते-जागते यदि पेशाब पर नियंत्रण नहीं रख पाता है अथवा हमेशा कपडे गीले करता हो तो अवश्य ही उसकी मूत्र नियंत्रण प्रणाली में कोई दोष है। अतः सभी आवश्यक जांच कराकर उपचार की आवश्यकता होती है। •
Foreskin Problems
INFORMATION AVAILABLE IN ENGLISH, HINDI AND GUJARATI
There are a number of conditions that can affect the foreskin (the piece of skin covering the top of the penis). They can affect boys of all ages and are usually easily treated.
The foreskin is the piece of skin that covers the top of the penis.
Conditions that can affect the foreskin include:
• Tight foreskin (Phimosis) – where the foreskin cannot be pulled back to reveal the head of the penis. All boys are born with phimosis. The foreskin retracts spontaneously by the age of 1 ½ to 2 years. A tight foreskin in puberty or adulthood can increase the risk of infection and cause problems with urination.
• Paraphimosis – A condition where the foreskin has retracted but gets trapped, restricting blood flow to the head of the penis. The penis will turn dark purple. Paraphimosis requires immediate medical attention as this condition can cause permanent damage to the penis if not treated early.
• Balanitis – an inflammation of the tip of the penis and foreskin usually caused by chemical irritation, bacterial or fungal infection. The head of the penis will become red, swollen and sore and there may be a thick and lumpy discharge.
What causes foreskin problems?
Foreskin problems can be the result of:
• Poor personal hygiene (not cleaning the head of the penis correctly)
• Infection
• Forcible attempts to retract the foreskin
What are the signs and symptoms of foreskin problems?
The appearance of the foreskin is usually enough to see whether there is a problem.
How are foreskin problems diagnosed?
In the case of paraphimosis (where blood flow is restricted and the penis turns purple), you should visit the hospital immediately as this condition can cause permanent damage to the penis.
How are foreskin problems usually treated?
In the case of infection, a child may be given a course of antibiotics or a steroid cream to reduce inflammation and irritation. The course of treatment may last between two and four weeks, depending on the severity of the strain of infection.
Some children may require a surgical procedure, such as:
• Circumcision – where the foreskin is removed altogether.
• Preputialplasty – where the opening of the penis is widened by an incision without removing the foreskin. The foreskin at the end of the operation would look just like a normal skin.
All of these procedures are carried out under anesthetic
Can foreskin problems be prevented?
Good hygiene is key to preventing problems that can be caused by infection.
In babies and children, the best way to clean the penis is by using water and baby soap. Don’t worry that you are not able to pull back the foreskin at this age – it’s very important not to try to retract a child’s foreskin forcibly, because this may cause damage to the delicate tissues of the penis. It could lead to bleeding, inflammation and the formation of scar tissue.
Once the foreskin begins to retract, the glans will naturally become more visible and easier to clean. It is important to be gentle – the less scrubbing the better. When boys reach adolescence, they should be encouraged to retract and clean their foreskin regularly.
What happens next?
Once treated, a child should not experience any further discomfort and there should be no further impact on his health.


 Acute Balanoposthitis
Acute Balanoposthitis

 Scarred prepuce
Scarred prepuce
 Photograph after circumcison
Photograph after circumcison
 Paraphimosis
Paraphimosis
 Zip Injury over prepuce
Zip Injury over prepuce
GUJARATI
ફાઇમોસીસ
ફાઇમોસીસ એટલે ઇન્દ્રિની ચામડી ઇન્દ્રિ ઊપર ચડી નહીં શકવાની ખોડ. બાળક જ્યારે જન્મે છે ત્યારે ઇન્દ્રિ તેની ખુદની ચામડીથી ઢંકાયેલી હોય છે. સામાન્ય સંજાગોમાં આ ચામડી ઇન્દ્રિ ઉપર ચડી શકતી નથી. કુદરતે આ વ્યવસ્થા એટલા માટે કરેલી છે કે જેથી બાળકના પેશાબની અંદર રહેલ એમોનિયાથી ઇન્દ્રિના મુખ અને પેશાબની નળીને નુકસાન ન થાય. સામાન્ય રીતે ઇન્દ્રિની ચામડી ઇન્દ્રિ ઉપર દોઢ થી બે વર્ષની અંદર આપોઆપ ચડતી થઈ જાય છે. પરંતુ દોઢ વર્ષની ઉંમર પછી પણ જા ચામડી ઇન્દ્રિ ઉપર ન ચડતી હોય તો આ બીમારીને ફાઇમોસીસ કહેવામાં આવે છે. ફાઇમોસીસની બીમારી માટે સુન્નત એટલે કે પેશાબની ચામડીનો આગળનો ભાગ કાઢી નાખવાની સર્જરી કરવામાં આવે છે. આ આૅપરેશન મુસલમાન, યહુદી અને બીજા ધર્મોમાં ધાર્મિક માન્યતાઓથી કરવામાં આવે છે. ચામડી સંપૂર્ણપણે ન કાઢવી હોય તો ‘Prepuceplasty’ નામની પણ એક સર્જરી કરી શકાય જેથી ચામડી ઇન્દ્રિ ઉપર આસાનીથી ચડી શકે અને ઇન્દ્રિનો દેખાવ નોર્મલ ઇન્દ્રિ જેવોજ રહેતો હોય છે. ફાઇમોસીસના કારણે ઘણીવાર ઇન્દ્રિના મૂખ ઉપર અને ઇન્દ્રિની ચામડીની અંદર ઇન્ફેક્શન પણ થાય છે. જેને ‘બેલેનોપોસ્થાઈટીસ’ કહેવામાં આવે છે. •
HINDI
फाइमोसीस
फाइमोसीस अर्थात इंद्रीय की त्वचा का इंद्रीय पर न चढ़ सकना। बच्चा जब जन्म लेता है तब उसकी इंद्रीय त्वचा से ढकी होती है। कुदरत ने यह व्यवस्था इसलिए रखी गई है ताकि बच्चे के मूत्र में उपस्थित अमोनीया के कारण इंद्रीय का मुख और मूत्र नलिका को हानि न होने पाए। सामान्यतया इंद्रीय की त्वचा इंद्रीय के उपर डेढ़ से दो वर्ष के भीतर अपने आप चढ़ती जाती है। लेकिन यदि डेढ़ वर्ष की आयु के बाद भी यदि त्वचा इंद्रीय के ऊपर नहीं चढ़ती है तो इसे फाइमोसीस कहते है। फाइमोसीस की बीमारी के लिए सुन्नत अर्थात इंद्रीय की चमड़ी के आगे के भाग को सर्जरी के द्वारा काट दिया जाता है। मुस्लिम, यहुदी और अन्य कुछ धर्मों में यह ऑपरेशन धार्मिक मान्यताओं के आधार पर किया जाता है। कई बार यदि चमड़ी पूरी तरह से न हटानी हो तो ‘प्रेप्युझ्प्लास्टी’ नामक सर्जरी की जा सकती है, जिससे की चमडी इंद्रीय के उपर आसानी से चढ़ सके और इंद्रीय का आकार सामान्य रहे। फाइमोसीस के कारण कई बार इंद्रीय के मुख पर और इंद्रीय की चमडी के भीतर संक्रमण हो जाता है। इसे ‘बेलेनोपोस्थाइटीस’ कहा जाता है। •
Foreign Body in the Air Passage (Respiratory tract)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
FOREIGN BODY IN THE AIR PASSAGE RESPIRATORY TRACT
Children have a tendency to put one or the other thing in their mouth. If the child is crying, laughing or taking a deep breath, a food particle or foreign body in the mouth may easily slip into the air passage and the lung tubes (bronchus). This may cause the child to have bouts of severe coughing and even difficulty in breathing. If the inhaled foreign body has gone unnoticed, the child may continue to have chronic cough and ill health and a suspicion may be raised only when the child visits a doctor or an x-ray is taken. Most of food particles like peanuts, gram seeds, beetel seeds etc. are not seen on x-ray. However, a suspicion of the same can be raised when the x-ray shows emphysematous changes due to air trapping in the lung. Foreign bodies in the respiratory tract are removed by bronchoscopy where an endoscope is placed through the air passage and the foreign body is removed.
Foreign bodies in the air passage may prevent the child from breathing normally and may also cause a risk to life. They should hence be treated as an emergency. ●


Left Bronchus & Bronchiole


Right Bronchus & Bronchioles

Main Bronchus

Carina

Epiglottis
GUJARATI
શ્વાસનળીમાં ફારેન બોડી
નાના બાળકોને કોઈપણ વસ્તુ મોંમાં મૂકવાની ટેવ હોય છે. કોઈપણ કારણસર રડતાં, હસતાં, ઉંડો શ્વાસ લેતાં મોંમાં રાખેલી વસ્તુ સીધી શ્વાસનળી અને તેની આગળ ફેફસાંની નળીમાં ભરાઈ જાય છે. આવું થાય ત્યારે બાળકને ખૂબ જ
ઉધરસ આવે છે. ઘણીવાર આ અકસ્માત ભૂલાઈ જાય છે. ઘણા દિવસો પછી પણ બાળકને ખાંસી મટતી ન હોવાથી બાળકનો છાતીનો X-ray પડાવવામાં આવે છે, અને તેમાં જા મેટાલીક ફારેન બોડી હોય તો દેખાય છે, પણ જાૅ
બિન મેટાલીક (દા.ત, સીંગનો દાણો) હોય તો તે દેખાતો નથી, પરંતુ ફેફસાંમાં દેખાતાં બદલાવ (Emphysema)થી ફારેન બોડી છે તેવો ખ્યાલ આવે છે.
જાૅ ફારેન બોડી મુખ્ય શ્વાસનળીમાં ફસાય તો બાળકને શ્વાસ લેવામાં સખત તકલીફ પડે છે અને ઘણીવાર બાળક મરણ પણ પામે છે. તાત્કાલીક શ્વાસનળીની દૂરબીનની તપાસ (બ્રોન્કોસ્કોપી) બાળકને બચાવે છે.
હોસ્પિટલ માં તાત્કાલીક પહોંચી શકાય તેમ ન હોય તો બાળકને ઊંધું પગથી લટકાવી, બરડા પર મારવાથી ફારેન બોડી શ્વાસનળીમાંથી નીકળી શકે.
જાૅ ફારેન બોડી નાની શ્વાસનળીની (બ્રોન્કસ) હોય તો પણ બ્રોન્કોસ્કોપીથી તેને કાઢવાથી બાળક તરત સા૨ું થઈ જાય છે.
શ્વાસનળીમાં સીંગનાં દાણા,ચણા,કચૂંકા અથવા અનેક જાતની મેટાલીક વસ્તુઓ બ્રોન્કોસ્કોપી દ્વારા કાઢી શકાય છે. •
 Gram Seed in the Air Passage
Gram Seed in the Air Passage
 Button Battery in the Air Passage
Button Battery in the Air Passage
 Vegetable particle in air passage
Vegetable particle in air passage
 Balloon in the air passage
Balloon in the air passage
HINDI
श्वासनली में फंसी बाहरी वस्तुएँ
छोटे बच्चों में किसी वस्तु को मुँह में डालने की आदत होती है। किन्हीं कारणों, जैसाकि बच्चों का रोना, हंसना, गहरी साँस लेना आदि के दौरान मुँह में रखी वस्तु सीधी श्वास नली से होकर के फेफड़ों की नली में फंस जाती है। ऐसा होने पर बच्चे को अत्यधिक खाँसी आती है। कई बार ऐसी घटना की ओर ध्यान नहीं जाता है। कई दिनों तक बच्चे की खाँसी मिटती नहीं है और धीमा बुखार भी रहता है। ऐसे में डॉक्टर भी कई बार एंटीबायोटिक और खाँसी की दवाई देते हैं। इसके बाद भी अगर खाँसी बंद नहीं होती है तो छाती का एक्स-रे करवा लेना चाहिए, जिससे यदि कोई धातु वाली वस्तु हो तो दिखाई देगी। यदि जैविक वस्तु (उदा. मूँगफली का दाना) हो तो एक्स-रे में दिखाई नहीं देगा, लेकिन फेफडों में हो रहे परिवर्तन के लक्षणों (एम्फायसेमा) से इसका अंदेशा मिल जाता है।
यदि बाहरी वस्तु श्वास नली में फंस जाती है तो बच्चे को साँस लेने में कठिनाई होती है और उसकी मृत्यु भी हो सकती है। तुरंत श्वास नली की दूरबीन से जांच (ब्रोंकोस्कोपी ) कर के बच्चे की जान बचाई जा सकती है।
यदि बाहरी वस्तु श्वास नली की शाखा (ब्रोंकस) में फंसी हो तो ब्रोंकोस्कोपी द्वारा उसे निकाल देने से बच्चा तुरंत स्वस्थ हो जाता है।
श्वास नली में मूँगफली का दाना, चना, कूंचा अथवा धातु की वस्तु की उपस्थिति की जाँच ब्रोंकोस्कोपी द्वारा की जाती है। ऐसी आपात परिस्थिति में जल्द से जल्द उपचार किया जाना चाहिए। •
Foreign body in Food Pipe and Stomach
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
FOREIGN BODY IN THE GASTROINTESTINAL TRACT
Children have a tendency to put one or the other thing in their mouth. Sometimes these things may get swallowed and stuck in the oesophagus or stomach and may create an emergency situation.
Oesophageal Foreign bodies: When the child swallows an object which is larger than the size of its oesophagus, it gets stuck into it. Objects like coins, hair pins, home decor pieces commonly get stuck in the oesophagus.
Nowadays, children have access to the button batteries commonly used in Chinese toys. This button battery if incidentally swallowed and stuck in the oesophagus can have disastrous consequences due to the alkali contained in it. This may even cause perforation of the oesophagus or its adjoining wind pipe. A swallowed button battery should hence be treated as a serious emergency.
Gastric Foreign bodies: Majority of the oesophageal foreign bodies pass into the stomach and further into the intestines. Most of them get spontaneously expelled transanally. However, a foreign body that is persistent or sharp may require intervention to be removed. Most of the gastric foreign bodies are removed by upper G.I. endoscopy.
What is to be done?: In children with foreign bodies, parents should restrain from giving laxatives or bananas. If possible, carry a sample of the foreign body that the child has swallowed if handy. A high degree of caution and urgency should be exercised for a swallowed button battery. ●
GUJARATI
આકસ્મિક ગળી ગયેલી વસ્તુઓ (ફારેન બોડી)
૨વર્ષની ઉંમર પછી બાળકોને ગમે તે વસ્તુ મોં માં મૂકવાની ઇચ્છા થતી હોય છે. આવી વસ્તુ ગળી જતાં તે અન્નનળી અથવા હોજરીમાં જતી રહે છે અને ઇમરજન્સી ઊભી થાય છે.
અન્નનળીમાં ફારેન બોડી : બાળકની અન્નનળીની સાઈઝથી મોટી વસ્તુ જ્યારે બાળક ગળી જાય તો તે અન્નનળીમાં ફસાઈ શકે છે. દા.ત. રૂપિયાનાં સિક્કા, માથાની પીન, પેÂન્સલના ટુકડાં વિગેરે. ચાઈનીઝ રમકડાંમાં વપરાતી બટન બેટરી રમકડાંમાથી બહાર આવતાં બાળક તેને મોંમાં મૂકે અને જ્યારે તે અન્નનળીમાં ફસાય અને તેને તાત્કાલિક કાઢવામાં ન અવે તો તેમાં રહેલાં સ્ટ્રોંગ આલ્કલી અન્નનળીમાં કાણું પાડી દે છે. ઘણીવાર અન્નનળીની બાજુમાં આવેલ શ્વાસનળીમાં પણ કાણું પાડે છે જે ખૂબ જ સીરિસય Âસ્થતિ છે.
હોજરીમાં ફારેન બોડી : મોટા ભાગની ફારેન બોડી અન્નનળીમાંથી પસાર થઈ હોજરીમાં જાય છે. અને ઘણી ખરી ફારેન બોડી આંતરડામાં જઈ સંડાસ વાટે બહાર નીકળી જાય છે. ફક્ત તીક્ષ્ણ ફારેન બોડી અથવા હોજરીમાં પડી રહેલી ફારેન બોડીને દૂરબીન વડે બહાર કાઢવી પડે છે.
શુ કરવું? : જુલાબની દવા ન આપો, કેળા ન ખવડાવો, ફારેન બોડીનો નમૂનો હોય તો ડાક્ટર ને બતાવવા સાથે લઈ જાઓ, બટન બેટરી સેલ ખૂબ જ નુકસાનકર્તા છે. •
HINDI
अकस्मात निगली गई वस्तु
२ वर्ष की आयु के उपरांत बच्चे किसी भी वस्तु को उठाकर मुँह में डाल देते हैं और ऐसी वस्तु के निगल लेने पर वह वस्तु अन्ननली अथवा पेट में चली जाती है और आपात स्थिति उत्पन्न हो जाती है।
बच्चे की अन्न नली के आकर से अधिक बड़ी वस्तु के निगल जाने पर वह गले में अथवा अन्न नली में फंस जाती है जैसे कि रूपये का सिक्का, हेर पीन, पेंसिल का टुकड़ा, चीनी मिट्टी के खिलौने आदि। बटन सैल से चलनेवाले खिलौनों की बैटरी निकाल कर बच्चा मुँह के अंदर डाल देता है। ऐसी वस्तु अन्न नली में फंस जाने पर यदि उसे तुरंत बाहर न निकाल लिया जाए तो उनमें मौजूद तीव्र आल्कली अन्न नली में छेद बना सकता है। कई बार अन्न नली के पास स्थित श्वास नली में भी छेद बना सकता है, जो गंभीर स्थिति उत्पन्न कर सकता है।
पेट में बाहरी वस्तुएँ
अधिकतर बाहरी वस्तुएं अन्न नली से होकर पेट में जाती है। इनमें से कई वस्तुएं मल के साथ बाहर आ जाती हैं। केवल तीक्ष्ण अथवा पेट में फंसी हुई वस्तुओं को ही दूरबीन की सहायता से बाहर निकालने की आवश्यकता होती है।
क्या करना चाहिए
जुलाब की दवाई नहीं देनी चाहिए, केला न खिलाएं। निगली गई वस्तु का नमूना उपलब्ध हो तो डॉक्टर को दिखाना चाहिए। बटन सैल बहुत नुकसानदायक है।•
Gastroesophageal Reflux and Fundoplication
What is gastro-oesophageal reflux?
Normally, when we swallow food and drink, it moves down the foodpipe (oesophagus) to the stomach, where it starts to be broken down by the acids released from the stomach wall. After it has been partially broken down, it passes through to the small and large intestines, where all the goodness and excess water is removed.
When a baby or child has gastrooesophageal reflux, the food and drink travels down the foodpipe as normal, but some of the mixture of food, drink and acid travels back up the foodpipe, instead of passing through to the large and small intestines. As the food and drink is mixed with acid from the stomach, it can irritate the lining of the foodpipe, making it sore. This is gastro-oesophageal reflux disease. Some children also breathe some of the mixture into the windpipe (aspiration), which can irritate the lungs and cause chest infections.
In some children, the symptoms associated with gastro-oesophageal reflux disease disappear with or without treatment, usually by the age of two. However, in some children, gastro-oesophageal reflux disease is more of a long-term condition and can have a serious effect on both the child and family’s quality of life. The options for treating gastro-oesophageal reflux disease are improving all the time, with new medicines and surgical options being discovered.
Remember, not all children with gastroesophageal reflux need surgery.
What is Fundoplication?
A fundoplication is an operation used to treat gastro-oesophageal reflux. It uses the top of the stomach to strengthen the sphincter so it is less likely to allow food, drink or acid to travel back into the foodpipe.
What does the operation involve?
Many a times, this surgery can also be done with the help of laparoscopy or key hole surgery.
There is a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons, or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision (cut) instead.
Details regarding the same will be explained to you by your doctor.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Any surgery carries a small risk of infection or bleeding.
What happens afterwards?
Your child will be monitored closely for the first couple of days.
After keyhole surgery, some older children may complain of shoulder pain and some crackling under the skin, caused by the carbon dioxide escaping into the tissue just under the skin; this does not usually last long and gradually improves over a day or two.
Your child will be able to drink when drainage from the naso-gastric tube or gastrostomy has slowed down and the fluid draining away is clear. As he or she gets used to drinking, small amounts of soft food can be added until your child is eating and drinking normally again. It may take up to 7 – 10 days for your child’s eating and drinking to get back to how it was before the operation.
Once your child is eating and drinking as normal and has recovered well from the operation, he or she will be able to go home. Most children stay in hospital for about five to seven days after this operation.
Are there any long-term effects of the operation?
Although the Nissen’s fundoplication operation is very successful at improving a baby’s gastro-oesophageal reflux disease and the symptoms associated with it, a quarter of all patients develop some long term effects afterwards, some of which we are able to treat.
Changes in feeding pattern – The operation makes the stomach slightly smaller. For some children this can mean that they may need to have smaller volumes of feed given more regularly.
Burping and vomiting – After the Nissen’s fundoplication operation, some children are unable to burp or vomit. In some this is temporary, but in many this is permanent.
Gas bloat – This is the name given to wind trapped in the stomach. It can usually be corrected by giving your child smaller feeds more frequently, rather than a few large feeds each day.
Dumping syndrome – This is a combination of things including nausea, retching, sweating, diarrhoea. It is caused by food travelling through the stomach at a much faster rate than usual so none of the goodness in the feed is absorbed. This can also be corrected by giving your child smaller feeds more frequently. These symptoms can take up to six weeks to settle.
Gall Stones
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
GALL STONES
Gallstones form when the liquid in the gallbladder (Bile) hardens.
The liver makes bile, and the gallbladder stores it until the body needs it. Bile contains water, cholesterol, fats, salts and proteins.
Gallstones are not as common in children as they are in adults. But some factors can put children at an increased risk:
- Having certain inherited blood problems, such as sickle cell disease or spherocytosis
- Obesity
- Family history of gallstones
- Taking certain medicines
The most common symptoms are pain in the upper abdomen. It may be associated with nausea or vomiting.
Ultrasound scan is diagnostic for gall stones. In the event of the stones blocking the biliary ducts, an MRI (MRCP Scan) may be necessary.
If the child’s gallstones cause symptoms, it will need surgery to remove the gallbladder. This surgery is called cholecystectomy and is mostly done by laparoscopy.
If the gall stones get lodged in a duct, they can block the flow of bile. This can cause the gallbladder to swell. Ongoing blockage can also lead to jaundice, infections, damage to the liver, gallbladder or pancreas.
If the child doesn’t have a gallbladder, the bile will simply flow from the liver directly into the intestine. The child should be able to eat normally and continue with normal activities after having the gallbladder removed. ●
GUJARATI
પિત્તાશયમાં પથરી
જા બાળકમાં વારંવાર પેટનો દુઃખાવો, ખાવા-પીવામાં તકલીફ, વજન વધતું અટકે, ઉલ્ટીઓ અથવા કમળો થાય, તો અચૂક પેટની સોનોગ્રાફી કરાવવી પડે છે.
સોનોગ્રાફીની તપાસમાં ઉપરની તકલીફવાળા બાળકોમાં આશરે પ% માં પિત્તાશયની કોથળી (જે લીવર નીચે હોય છે) માં એક અથવા અનેક પથરી જાવા મળે છે.
પિત્તાશયની કોથળીનું કામ લીવરમાંથી આવતા પિત્તનું સંગ્રહ કરી જરૂર પડે પાચન માટે આંતરડામાં મોકલવાનું છે. પિત્તમાં રહેલા ક્ષાર અને કોલેસ્ટ્રોલનું પ્રમાણ બગડી જાય તો પથરી બનવાનું શરૂ થાય છે. પિત્તાશયની થેલી નબળી હોય તો પણ પથરી થઈ શકે છે. ખૂબ ઓછા કિસ્સામાં બાળકને લોહીની બીમારી હોય તો પણ નાની-નાની પથરી બને છે.
બાળકના ઈલાજ માટે દર બે-ત્રણ માસે પેટની સોનોગ્રાફી દ્વારા પથરીની સાઈઝ પર ધ્યાન રાખવામાં આવે છે. જા પથરીની સાઈઝ અથવા બાળકની તકલિફો વધે તો આૅપરેશન દ્વારા પિત્તાશયની થેલી અને તેમાં રહેલી પથરી કાઢવાની જરૂર પડે છે. આૅપરેશન લેપ્રોસ્કોપી(દૂરબીન)થી જ કરાવવું હિતાવહ છે.
પિત્તાશયની થેલી કઢાવવાથી બાળકને તકલીફ કે લાંબે ગાળે કોઇ નુકસાન થતું નથી. પિત્તનો પ્રવાહ લીવરમાંથી નળીઓ દ્વારા સીધો આંતરડામાં જાય છે. તેથી પાચનક્રિયામાં પણ કોઇ તકલીફ થતી નથી. •
HINDI
पित्ताशय में पथरी
पित्ताशय में जब द्रव के रूप में पित्त ठोस होने लगाता है तो वह पथरी बन जाता है। यदि किसी बच्चे को बार-बार पेट में दर्द, खाना-खाने में तकलीफ, वजन का नहीं बढ़ना, कभी-कभी उल्टी या पीलिया होता है, तो ऐसे में बच्चे के पेट की सोनोग्राफी कराना जरूरी है। सोनोग्राफी की जाँच में ऊपर बताई गई समस्याओं वाले बच्चों में लगभग ५% बच्चों में पित्ताशय की थैली में एक या अनेक पथरी होती है।
पित्ताशय की थैली का काम लीवर में से निकल रहे पित्त का संग्रह करके आवश्यकता अनुसार पाचन हेतु आंतों में भेजना होता है। पित्त में निहित क्षार और कोलेस्ट्रोल का प्रमाण असंतुलित होने पर पथरी बननी शुरू होती है। पित्ताशय की थैली ज्यादा कमजोर होने पर भी पथरी बन सकती है। बहुत कम मामलों में यदि बच्चे को खून से संबंधित कोई बीमारी है तो पथरी बन सकती है। बच्चे के इलाज के लिए हर दो-तीन महीने में सोनोग्राफी द्वारा पथरी के आकार पर ध्यान रखा जाता है। यदि पथरी का आकार बढ़ता जाता है या बच्चे को ज्यादा तकलीफ हो, तो ऑपरेशन द्वारा पथरीवाले पित्ताशय की थैली निकालने की आवश्यकता होती है। यह ऑपरेशन लेप्रोस्कोपी द्वारा कराना उचित है।
पित्ताशय की थैली निकाल देने पर बच्चे को भविष्य में कोई नुकसान नहीं होता। पित्त का प्रवाह लीवर में से निकलकर सीधा आंतों में चला जाता है, जिसे पाचन क्रिया में कोई तकलीफ नहीं होती। •
Gastroschisis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
GASTROSCHISIS
Gastroschisis is a type of abdominal wall defect which occurs when the child’s abdomen does not develop fully while inside the womb. It affects 1 in every 3000 children. In gastroschisis, the intestines are open to the air when the child is born.
The umbilical cord is visible but pushed to the side by the exposed intestines.
Gastroschisis is a serious condition and needs prompt treatment soon after birth. Immediately after birth, the exposed intestines need to be wrapped in a sterile saline soaked cloth which reduces the amount of fluids and body heat lost and protects the intestines from further damage.
Once the child is stable, it will have an operation to put the intestines back inside the abdomen. Occasionally a ready made plastic bag / mesh is placed over the intestines and they are gradually moved back into the abdomen which may take a few days. ●
ગેસ્ટ્રોસ્ચેસીસ
દર ૩૦૦૦ એ ૧ બાળકમાં જાવામાં આવતી આ ખોડમાં પેટની દીવાલનાં વિકાસના અભાવે બાળકના જન્મ સમયે તેના પેટનાં આંતરડા પેટની બહાર રહેલા હોય છે.
બાળકનો જન્મ થતાં જ આ ખોડ જાઈ શકાય છે. આંતરડા દૂંટીની નાળની જમણી બાજુએથી બહાર નીકળતા હોય છે. આ ખોડમાં બાળકને તાત્કાલિક સારવારની જરૂર પડે છે. સારવાર અર્થે મોકલતાં પહેલા બાળકનાં આંતરડાને ચોખ્ખા સલાઈનવાળા કપડાંથી ઢાંકી દેવા જાઈએ. બાળકની સ્થતિને સ્ટેબીલાઈઝ કર્યા બાદ ઓપરેશન દ્વારા આંતરડાને પેટમાં પાછા મૂકીને પેટની દીવાલ બંધ કરવી પડે છે. અમુક કેસમાં આંતરડાને પ્લાસ્ટીકની બેગમાં મૂકી ધીરે ધીરે પેટમાં પાછા મુકાય છે. •
गेस्ट्रोस्काईसीस
गेस्ट्रोस्काईसीस पेट की दीवार का एक प्रकार का दोष है। हर ३००० में १ बच्चा इस दोष से प्रभावित होता है। गेस्ट्रोस्काईसीस की स्थिति में, उदर की दीवार पूर्णरूप से निर्मित नहीं हो सकने के कारण आंतें बाहर विकसित होती हैं और बच्चे के जन्म के समय शरीर से बाहर खुले में रह जाती है।
गेस्ट्रोस्काईसीस की पहचान तुरंत ही हो जाती है। गर्भनाल दिखाई देती है परंतु वह खुले आंतों के कारण एक ओर धकेली सी दिखाई देती है। गेस्ट्रोस्काईसीस एक गंभीर परिस्थिति है। जन्म के तुरंत बाद इसका उपचार किया जाना आवश्यक होता है। जन्म के तुरंत बाद, बच्चे को पानी में भीगोए जंतुरहित कपड़े में लपेट लेना चाहिए। इससे बच्चे के शरीर से पानी तथा ऊष्मा का नाश कम होगा और आंतों को नुकसान से सुरक्षित रखेगा। बच्चे के स्थिरता प्राप्त कर लेने के उपरांत, आंतों को उदर में पुनःस्थापित करने हेतु एक ऑपरेशन किया जाता है। कभी-कभार एक प्लास्टिक की तैयार थैली/जाली खुली आंतों पर रख दी जाती है, तत्पश्चात, आंतों को क्रम से उदर में स्थापित कर दिया जाता है। इसमें कुछ दिनों का समय लग सकता है। •
Gynecological Problems in Children
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
GYNECOLOGICAL PROBLEMS IN CHILDREN
(1) PASSAGE OF MUCUS OR BLOOD PER VAGINUM: Exposure to many maternal hormones may cause the child to have a thick, milky discharge from the vagina. This may continue intermittently until the child is on breast milk. Sometimes at 2 or 3 days, the child may also have a little bleeding from her vagina. This is perfectly normal.
(2) LABIAL FUSION: A condition when the two labia minora stick together. It may appear that the child does not have a vagina, but that is not the case. It can sometimes happen after an inflammation of the labial area or vulvovaginitis. The fusion will usually separate itself or by gentle pressure. In younger girls, local application cream is prescribed to help prevent the labia from fusing again. Very occasionally, the girl may get a urinary tract infection due to labial fusion.
(3) IMPERFORATE HYMEN: The hymen is a ring like membrane interposed between the proximal uterovaginal tract and the vaginal introitus. When this central portion of the hymen is closed, it is known as an imperforate hymen. This may cause vaginal secretions to get accumulated causing the hymen to protrude through the vaginal introitus giving the appearance of a vaginal mass. This may also cause compression over the urethral opening leading to urinary retention in the child. Management of imperforate hymen is straightforward and the long-term complications are minimal.
(4) VAGINAL DISCHARGE: Children can also develop a vaginal odour which is considered normal. Wearing a diaper can exacerbate the odour especially when mixed with urine and stools. With no other symptoms, bathing and frequent diaper changes can keep this under control.
Noninfectious form of vaginitis can be caused by perfumed soaps or detergents. In some children this can be an allergic reaction to such chemicals. In addition to unusual odour, the child may have itching, burning or discharge.
Infectious vaginitis is caused by bacteria and lead to a foul smelling or fishy odour from the vagina. Bacteria can also spread from the anus to the vagina by wiping or cleaning the child from back to front instead of the opposite. In rare cases, an accidentally inserted and retained foreign body in the vagina may also be the cause of a foul smelling discharge.
A thorough medical examination and treatment would be necessary in these cases. ●
GUJARATI
બાળકમાં ગાયનેક પ્રોબ્લેમ
નાની બાળકીમાં ઘણીવાર જુદાં જુદાં ગાયનેક પ્રોબ્લેમ જાવા મળે છે.
(૧) બેબીને માસિક આવવું અથવા મ્યુક્સ (ચીકાશ) આવવું :
ખાસ કરીને આ નવજાત બાળકીઓમાં જાવા મળે છે. તેનું મુખ્ય કારણ માતાનાં હોરમોનની અસર છે. માનું દૂધ પીતા બાળકમાં ઘણાં મહિના સુધી આ તકલીફ રહી શકે છે. અને ધીમે ધીમે આપમેળે મટી જાય છે.
(૨) લેબીયલ ફ્યુઝન :
બાળકીનાં યોનીમાર્ગના મુખની ચામડી (લેબિયા માઈનોરા) ઘણીવાર એકબીજાને ચોંટી જાય છે અને બહારથી તપાસ કરતા લાગે કે બેબીને યોનિમાર્ગ જ નથી, પણ આવું હોતું નથી. સાધારણ પ્રેસરથી આ જાડાણ છૂટું પડી જાય છે અને માતાને બાળકને દરરોજ નવડાવતી વખતે કેવી રીતે ફરી આ જાડાણ ન થાય એ સમજાવાય છે. આવા બાળકોને પેશાબમાં ઇન્ફેક્શન થવાની તકલીફ હોઈ શકે.
(૩) ઈમપરફોરેટેડ હાઈમન :
યોનિમાર્ગની અંદરના ભાગમાં આવેલ પડદાં (હાઈમન)નું છિદ્ર બંધ થઈ જવાથી યોનિમાર્ગમાં બનતા ચીકાશ અને પ્રવાહી અંદર ભરાઈ રહે છે. આ કારણે ઘણીવાર પેશાબનો ભરાવો અને યોનિમાર્ગમાં ઇન્ફેક્શન થઈ શકે છે. આૅપરેશન દ્વારા આ પડદાંનું છિદ્ર મોટું કરવાથી સારું થઈ જાય છે.
સારવાર ન મળવાથી મોટી ઉંમરે આવી બાળકીઓ માસિક નહીં આવવાની તકલીફ સાથે આવે છે. સોનોગ્રાફીમાં માસિક યોનિમાર્ગ અને ગર્ભાશયમાં ભરાઈ ગયેલું દેખાય છે. દૂરબીન વડે આૅપરેશન કરી આ તકલીફ સારી થઈ જાય છે.
(૪) વજાયનલ ડીસ્ચાર્જ :
આવી તકલીફ વાળી બાળકીને યોનિમાર્ગમાં ખંજવાળ આવે છે અને પેશાબમાં બળતરા થાય છે.
વધુ પ્રમાણમાં અને વધારે પડતો વાસવાળો બગાડ યોનિમાર્ગમાં કોઈ ઇન્ફેક્શન અથવા ફોરેન બોડી હોવાથી થાય છે. એનેસ્થેશિયા આપી યોગ્ય તપાસ કરવાથી તકલીફનું સમાધાન થાય છે. •
HINDI
बच्चों में स्त्रीरोग सम्बंधी समस्याएं
१) योनि मार्ग से बलगम या खून का बहना :
नवजात बालिका के गुप्तांग पर मातृ हार्मोन के प्रभाव से योनि से गाढ़ा, दूधिया रिसाव हो सकता है। कभी बच्ची की योनि से थोड़ा रक्त रिसाव भी हो सकता है। यह पूर्णतः सामान्य बात है।
२) योनि के होठों (भगोष्ठ) का आपस में जुड़ा होना (लेबियल फ्यूज़न) :
लेबियल फ्यूज़न वह स्थिति है जब दो लघु भगोष्ठ एक-दूसरे के साथ चिपक जाते हैं। जांच करने पर ऐसा प्रतीत होता है मानो बच्ची की योनि ही नहीं है, परंतु वास्तव में ऐसा नहीं होता है। इस प्रकार का विलय प्रायः अपने-आप अथवा कोमल दबाव से अलग हो जाता। इस प्रकार का भगोष्ठ विलय पुनः न हो इसके लिए उस स्थान पर लगाने के लिए क्रीम दी जाती है। भगोष्ठ विलय के कारण यदा-कदा लड़कियों के मूत्रमार्ग में संक्रमण हो सकता है।
३) छिद्रहीन योनिच्छद (इम्परफोरेट हाइमेन) :
हाइमेन एक झिल्ली है जो योनि के भीतर गर्भाशय के समीप जड़ी हुई होती है। इसके मध्य भाग के बंद होने की स्थिति को इम्पर्फोरेट हाइमेन कहते हैं। इसके परिणामस्वरूप
Hypospadias
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is hypospadias and what causes it?
Hypospadias is a birth defect affecting a boy’s penis.
It is a combination of three separate problems:
- The hole through which urine passes (meatus) is not at the tip of the penis
- The foreskin is gathered at the back of the penis with none at the front
- The penis may be bent when stiff.
The position of the meatus varies; in some boys, the hole is only a small distance away from the tip of the penis, whereas in others, it is at the base of the penis, in the scrotum or behind the scrotum.
About one in every 300 boys has hypospadias, although this figure seems to be rising. We do not know what causes hypospadias; more research is needed to learn more about the causes. It is unlikely to have been caused by anything that happened during pregnancy. Hypospadias can be associated with other conditions, such as inguinal hernia or undescended testicles, and your doctor will check your child to confirm or rule out any other problems.
Incomplete prepuce seen in hypospadias

Hypospadias
How is hypospadias diagnosed?
Hypospadias is usually diagnosed by clinical evaluation of the appearance of the penis as early as at birth.
Most boys need consultation when a few months’ old, so that treatment can be planned for when the child is about a year old. It is important that circumcision does not take place, as the foreskin is needed during the operation.
How is hypospadias treated?
Although hypospadias does not cause any immediate problems and is not life threatening. If hypospadias is left untreated it may not be possible for the child to pass urine standing up as the urinary stream may go on to wet his trousers or legs. Later on in life, having an adequate erection and having sex may be difficult. The aim of the operation is to straighten the penis, move the meatus to the tip of the penis and to remove the excess foreskin. By doing this, the penis will also look more normal. Usually, it is possible to make these corrections in one operation, but if the hypospadias is severe, correction may be needed in two or three stages in separate operations.
What does the operation involve?
The operation is carried out under an anaesthetic and lasts between one and two hours, depending on the severity of the hypospadias. The skin of the penis is used to create a tube, which extends the length of the urethra so that a new hole can be created at the tip of the penis.
Are there any risks?
There is also a small risk of infection, but your child may be given antibiotics as a precaution.
After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe.
For about one in ten boys, the original hole opens up again, so that your son passes urine through two holes. This can happen at any point after the operation. Small holes or fistula heal on their own over a course of 4 – 6 months. It will need to be fixed if it does not heal on its own by an operation. Occasionally, the new hole at the tip of the penis becomes small and your son may need follow up and dilatation to keep it of an adequate size.
What happens after the operation?
After the child comes back from operation theatre, he will be able to eat and drink once it wakes up and feels like it. When he comes back from the operating theatre, there will be a thin, tube (catheter) draining urine from your child’s bladder and a large dressing covering the penis; these will both need to stay in place for one week.
The drainage tube can irritate the inside of the bladder, causing ‘bladder spasm’, but we will give your child some medicine to reduce this as well as pain relief medicine.
The dressing and drainage tube will need to stay in place for one week. As there is a small risk of infection, your child is likely to need a course of antibiotics for a week after the operation The dressing and tube will be removed a week after surgery. When the dressing has been removed, the penis will look red and swollen; this is normal and it will settle down within a few days.
Your son will be called for follow up a week to 10 days after surgery. If need be, the new tube will be examined with a dilator. This is a short procedure and your son will be ready to go home in about 3-4 hours.

 Distal Penile Hypospadias
Distal Penile Hypospadias

 Proximal Penile Hypospadias
Proximal Penile Hypospadias
GUJARATI
હાયપાસ્પૅડીઆસ
હાયપાસ્પૅડીઆસ એ છોકરાઓમાં જાવામાં આવતી એક સામાન્ય ખોડ છે. દર અઢીસો બાળકોએ એક બાળકમાં આ ખોડ જાવા મળે છે. આ ખોડમાં પેશાબનો રસ્તો ઇન્દ્રિની છેવટના ભાગમાં ખૂલવાને બદલે ઇન્દ્રિની નીચેના ભાગમાં ખૂલતો હોય છે. આ રસ્તો વૃષણ કોથળીથી લઈને ઇન્દ્રિના છેવટના ભાગ સુધી ગમે ત્યાં ખૂલી શકે છે અને જે જગ્યાએ આ રસ્તો ખુલે તેના પરથી તેનું વર્ણીકરણ કરવામાં આવે છે. જેમકે ‘પ્રોક્ષીમલ હાયપાસ્પૅડીઆસ’ અને ‘ડીસ્ટલ હાયપાસ્પૅડીઆસ’. આ ખોડમાં ઇન્દ્રિની ઉપરની ચામડી પણ અધૂરી હોય છે. હાયપાસ્પૅડીઆસનું આૅપરેશન સામાન્ય સંજાગોમાં બે વર્ષની ઉંમર પહેલાં કરી દેવું જાઈએ. બાળકને બે વર્ષની ઉંમરમાં પેશાબ અને મળ માર્ગનો કંટ્રોલ આવી જતો હોય છે અને બે વર્ષની ઉંમર પહેલાં આ આૅપરેશન કરવાથી બાળકને શારીરિક અને માનસિક રીકવરીમાં તકલીફ થતી નથી. ૮૦% થી ૯૦% બાળકોમાં હાયપાસ્પૅડીઆસનું આૅપરેશન ફક્ત એક સ્ટેજમાં કરી શકાય છે. અલબત્ત, ઘણા સીવીયર હાયપાસ્પૅડીઆસના દર્દીઓમાં બે અથવા ત્રણ સ્ટેજમાં પણ આૅપરેશન કરવા પડતાં હોય છે. આ આૅપરેશનમાં કોઈ કૃત્રિમ પ્રકારની નળી મૂકવામાં આવતી નથી. બાળકના પોતાના સ્નાયુ અને ચામડીમાંથીજ આ આૅપરેશન કરવામાં આવે છે. આૅપરેશન પછી બાળકનો શારીરિક અને માનસિક વિકાસ નોર્મલ હોય છે અને આગળ જતાં તેનાં લગ્ન જીવનમાં કે બાળકો થવામાં કોઈપણ આડઅસર પડતી નથી. •
HINDI
हायपोस्पेडीआस
हायपोस्पेडीआस प्रत्येक २५० में से १ पुरूष बालकों में देखा गया है। इस प्रकार के दोष में मूत्रमार्ग का छेद लिंग के सिरे के बजाय लिंग की सतह के नीचे स्थित होता है। यह हमेशा शिशन के मुख पर खुली त्वचा के साथ अधूरा (hooded prepuce) होता है। मूत्रमार्ग का छेद शिशन के सिरे से लेकर अंडकोश क्षेत्र में कहीं भी स्थित हो सकता है और तदनुसार इसे समीपस्थ, मध्य और दूरदराज के पेनिल हाइपोस्पिडिया के रूप में वर्गीकृत किया जाता है। इसके साथ अनवतीर्ण वृषण जैसी अन्य विसंगतियाँ हो सकती है। हायपोस्पेडीआस के लिए सर्जरी 1 1/2 – 2 साल की उम्र के आसपास की जाना चाहिए। यही लक्ष्य होना चाहिए कि बच्चे के टॉयलेट प्रशिक्षित हो जाने से पहले ही उपचार पूरा हो जाना चाहिए। लगभग ८० – ९०% मामलों में हाइपोस्पिअडिया एक ही चरण में किया जा सकता है। हालांकि, समीपस्थ और जटिल हायपोस्पेडीआस के लिए, दो या दो से अधिक चरणों में सर्जरी की आवश्यकता हो सकती है। हायपोस्पेडीआस के लिए सर्जरी में बच्चे की अपनी त्वचा और ऊतकों से नए मूत्रमार्ग का निर्माण किया जाता है। किसी भी प्रकार की कृत्रिम नलिका लगाने की कोई आवश्यकता नहीं है। जिन बच्चों पर हायपोस्पेडीआस के लिए सर्जरी की जाती है उनका शारीरिक और मानसिक विकास सामान्यरूप से होता है। उन्हें अपने वैवाहिक जीवन में तथा अपनी प्रजनन क्षमताओं में कोई दीर्घकालिक समस्याएँ नहीं होती हैं। •
Hydronephrosis
How does the urinary system work?
The urinary system consists of the kidneys, the bladder and ureters. The kidneys filter the blood to remove waste products and form urine. The urine flows from the kidneys down through the ureters to the bladder. From here it passes through another tube called the urethra to the outside when urinating.
The ureters tunnel through the wall of the bladder at an angle to form a flap that acts as a valve. There is also a ring of muscle (sphincter) at the junction of the bladder and the urethra that stops urine leaking out in between episodes of urination. When passing urine, the muscles of the bladder wall squeeze the urine out of the bladder, at the same time as the muscles in the sphincter need to relax to let the urine flow down the urethra.
The valves between the ureters and the bladder prevent urine flowing backwards into the ureters, so that all the urine in the bladder is passed in one go, as the urine cannot travel anywhere else. As the urine leaves the bladder at a high pressure, the valves stop this high pressure being passed on to the kidneys.
What is hydronephrosis?
Hydronephrosis is a condition that can occur in the womb, where a baby’s kidneys fill up with urine and become larger. This can happen for various reasons. Hydronephrosis can also occur in adults, but the cause and treatment modalities are different from that of a child.
What are the symptoms of hydronephrosis?
Even if hydronephrosis is diagnosed before birth, this should not cause any symptoms in the mother and should not alter her antenatal care, other than possibly having a few more scans. Hydronephrosis does not usually cause a baby any problems before birth, but he or she may need close monitoring and assessment after birth to discover what is causing the hydronephrosis and keep an eye on the condition.
How is hydronephrosis diagnosed?
It is often diagnosed before a baby is born, as the enlarged kidneys can be seen on an ultrasound scan. Hydronephrosis can also be diagnosed after the baby is born using ultrasound scans.
What causes hydronephrosis?
There are many causes of hydronephrosis, including:
A blockage, which can occur between the kidney and the ureter (pelviureteric junction or PUJ), between the bladder and the ureter (vesicoureteric junction or VUJ) or in the urethra (posterior urethral valve).
How common is the condition?
About 1 in every 300 people has one kidney affected by hydronephrosis. About 1 in every 600 people have both kidneys affected by hydronephrosis.
How can hydronephrosis be treated?
If the hydronephrosis is diagnosed during pregnancy, early treatment will consist of monitoring with ultrasound, to check that the baby is growing normally and the kidneys are not getting too large. The baby will usually be born by a routine delivery.
After the baby is born, the hydronephrosis will be monitored using ultrasound scans and other tests. The overall treatment for hydronephrosis depends on what is causing it:
- If the cause is VUR, the child will probably be treated using antibiotics. Details can be obtained on the information on vesicoureteric reflux.
- If the cause is a blockage, the treatment will depend on the degree of the blockage, the effect it is causing on the functioning of the kidneys or symptoms it is producing i.e. pain, urinary tract infections etc. In severe cases surgery may be necessary to clear the blockage. Many children with mild or moderate degrees of obstruction, regular follow up with close monitoring may be necessary. The decision of treatment however varies from child to child. Operation done for hydronephrosis to clear the blockage between the kidney and ureter is called a ‘pyeloplasty’.
What is the future for children with hydronephrosis?
If the cause of the hydronephrosis is an obstruction and this is removed, your child’s kidneys will be able to work properly. If the cause of the hydronephrosis is VUR that is not too severe, your child’s kidneys are also likely to work properly. If the cause of the hydronephrosis is severe VUR, the outlook may be less good. Your child may need an operation to correct the reflux and his or her kidneys may be damaged. However, the earlier the hydronephrosis is discovered, the better the outcome for your child.
What is a pyeloplasty and why is it needed?
A pyeloplasty is an operation to remove a blockage in one of the ureters.
The blockage in one of the ureters is stopping urine flowing easily from the kidney into the bladder. The blockage is usually present from birth, but occasionally may appear later. If the ureter remains blocked, the kidney could become swollen and damaged. Sometimes, the blockage is caused by blood vessels getting in the way of the ureter. In this case, they will be moved and secured away from the ureter during the operation, but not removed.
What does the operation involve?
The operation involves locating the blockage in the ureter, remove the affected section and joining the cut ends of the ureter again. Details regarding the same will be explained in further details by the doctor.
Hydrocephalus (Large Head)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is hydrocephalus?
Hydrocephalus occurs when either too much cerebrospinal fluid (CSF) is produced (very rare) or when it is stopped from circulating or being re-absorbed. The CSF builds up within the ventricles (cavities) of the brain resulting in increased pressure on the brain. In babies, this also causes the head to enlarge.
CSF is a watery liquid that surrounds the brain and spinal cord, acting as a ‘cushion’. It also supplies nutrients to the brain.
What causes hydrocephalus?
The most common causes are:
- Congenital – This means that your child was born with hydrocephalus. Children born with spina bifida often develop hydrocephalus. This does not mean that all children with hydrocephalus also have spina bifida.
- Prematurity – Hydrocephalus can occur as a complication of being born too early, and when there has been bleeding in the brain.
- Meningitis – Hydrocephalus can occur as a complication of meningitis as the infection may cause a problem with reabsorption of CSF.
- As a complication from a brain tumour – this does not mean children with hydrocephalus develop brain tumours.
- Unknown – In many cases, we do not know what caused the hydrocephalus.
A child with massive hydrocephalus
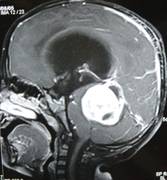
MRI Scan of a child with hydrocephalus because of a brain tumour
How is hydrocephalus diagnosed?
It is usually diagnosed by an increasing head circumference in infants, an ultrasound scan, a CT scan or sometimes an MRI scan.
How is hydrocephalus treated?
If hydrocephalus is not treated, your child’s head would get larger and the pressure on the brain would interfere with his or her development. In severe cases, this can result in permanent brain damage or visual problems. The aim of treatment is to reduce the pressure on the brain by draining the CSF away.
The fluid is drained away using a ‘shunt’, which is a long tube made of silicone. It is inserted in to the ventricles in an operation and drains the CSF away to the abdomen. The shunt contains a valve so that the fluid can only drain away from the head at the desired rate.
The operation
Part of your child’s hair, behind the ear, will be shaved and he or she will have an incision (cut) there in a horseshoe shape and a small incision on his or her abdomen.
Your child will have this operation under a general anaesthetic. The operation takes about 45 min to an hour. At the time of surgery fluid that is drained from the brain will be sent to the laboratory for examination.
What happens after the operation?
Close observation will be needed following surgery. Most children are able to take oral feeds the same evening of the operation. The usual stay in hospital is four to six days.
To begin with, the area around the top of the shunt may be slightly raised, but as the swelling settles and your child’s hair grows back you will not notice this. As your child grows, the area will become less prominent.
Going home
Your child may have dissolvable stitches or they may have stitches that need to be removed seven days after the operation.
Complications of a shunt
There can be complications to having a shunt inserted, of which you should be aware. The most common could be either an infection or a blocked shunt.
Symptoms of Infection
The symptoms of an infection in the shunt may include:
- Headache
- Irritability
- High temperature (over 37°C)
- Not feeding well
- Possibly vomiting
- Possibly drowsy
Symptoms of a blocked shunt
In babies:
- A bulging fontanelle (soft part of the top of the head)
- Vomiting
- Crying and irritability
- Becoming sleepy (less responsive)
- Looking pale
- Increased head size
In toddlers and children:
- Headache
- Vomiting
- Tiredness
- Drowsy
- Looking pale
GUJARATI
માથું મોટું હોવું
બાળકનું માથું મોટું હોવું એક ચિંતાનો વિષય જરૂર છે, અને તેનાં માટે ડાક્ટરની સલાહ જરૂરી છે. જન્મથીજ ડાક્ટર માથું અને છાતીના માપનો રેકોર્ડ રાખે છે અને તેને સ્ટાન્ડર્ડ ચાર્ટ સાથે સરખાવે છે. તેના પ્રમાણે સતત વધતાં માથા માટે જરૂરી તપાસ કરાવવી પડે છે.
માથું મોટું થવાનું સૌથી મુખ્ય કારણ નવજાત બાળકોના મગજની અંદર આવેલ પાણી (C.S.F.) નો ભરાવો છે. જેને હાઈડ્રોકેફલસ કહે છે. આમાં બાળકનું માથું નિયમિત ગતિથી વધ્યાં કરે છે. બીજા કારણોમાં બાળકને જન્મ પછી બ્રેન હેમરેજ થયું હોય તો પણ માથું મોટું થાય છે. જ્વલ્લે જ બાળકને બ્રેન કેન્સર જેવી બીમારીથી માથું મોટું થઈ શકે છે.
હાઈડ્રોકેફલસ સૌથી સામાન્ય કારણ છે. અને તેનું સચોટ નિદાન નાના બાળકોમાં સોનોગ્રાફી દ્વારા અને મોટા બાળકોમાં સી.ટી.સ્કેન અથવા એમ.આર.આઈ.થી થઈ શકે છે.
બાળકોનાં સર્જન આવા કેસમાં એક શંટ મૂકવાની સલાહ આપે છે જેમાં એક પાતળી ટ્યુબ દ્વારા માથાના વધારાના પાણીને પેટમાં ડાયવર્ટ કરાય છે. આ ટ્યુબને વી.પી. શંટ કહે છે.તેનું રેગ્યુલર ચેકઅપ કરાવતાં રહેવું જરૂરી છે. •
HINDI
बडा सिर (जल शीर्ष)
बच्चे के सिर का बड़ा होना चिंता का विषय जरुर है और इसके लिए डॉक्टर से परामर्श जरुरी है। बच्चे के जन्म लेते ही डॉक्टर उसके सिर तथा छाती के माप का रिकार्ड रखते है और उसकी तुलना मानक चार्ट से करते रहते हैं। अगर सिर के माप में निरंतर वृद्धि हो तो जाँच आवश्यक होती है।
इसका प्रमुख कारण नवजात शिशु के मस्तिष्क में जल भराव (C.S.F.) जिसे हाइड्रोसीफेलस कहते हैं। इसमें बच्चे का माथा नियमित गति से बढ़ता रहता है। इसका दूसरा कारण जन्म के समय बच्चे को ब्रेन हेमरेज होना भी हो सकता है। ब्रेन कैंसर जैसी बीमारी के कारण सिर का बड़ा हो जाना बच्चों में कम ही पाया जाता है।
हाइड्रोसीफेलस एक सर्वसामान्य कारण है। बच्चों के मामले में इसका सटीक निदान सोनोग्राफी के द्वारा तथा वयस्कों में सी.टी. स्कैन अथवा एम.आर.आई के द्वारा किया जाता है।
बालरोग सर्जन ऐसे मामलों में एक सादा सा शंट लगाने की सलाह देते हैं। इस प्रक्रिया में एक नलीका के माध्यम से माथे का पानी पेट में डायवर्ट किया जाता है। इस नलिका को वी.पी. शंट कहते हैं। इस में नियमित चेकअप की आवश्यकता होती है। •
Hydrocele
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a hydrocele and what causes them?
A hydrocele is a very common condition affecting boys, where a fluid filled sac develops inside the scrotum, making it look swollen. It is not painful and feels like a balloon filled with water. One or both sides of the scrotum can be affected.
While your child was developing in the womb, the testicles were developing inside the abdomen. Towards the end of pregnancy, the testicle travel through a passage into the scrotum. A hydrocele can develop when this passage fails to close, allowing fluid from the abdomen to flow through it to the scrotum. This causes the fluid-filled sac to develop.
Can a hydrocele be prevented?
There is no known way of preventing hydroceles. It is not due to anything a mother did during pregnancy.
How is a hydrocele diagnosed?
The doctors will feel your child’s scrotum to see if the swelling is caused by fluid or something solid. This can also be confirmed with an ultrasound scan.
How is a hydrocele treated?
Most hydroceles go down within a few months of birth, but occasionally they last longer. If a hydrocele is still present after the first birthday or is causing any problems, an operation might be suggested. Surgery for hydrocele is the same as that for a hernia wherein the passage through which the fluid or the bowel comes down from the abdomen is closed.
What does the operation involve?
The operation is carried out under general anaesthetic and lasts for about 30 – 45 minutes. Once your child is asleep, the surgeon will make a small incision (cut) on the lower abdomen to remove the fluid inside your child’s scrotum. The passage between the abdomen and scrotum will then be sealed off. The cut will be closed with dissolvable stitches.
Can this operation be done laparoscopically?
Operation in hydrocele involves closing of the open passage through which the testis has come down. This can be done from outside as in open surgery or from inside by laparoscopy. With the help of laparoscopy we are able to look at the opposite side to see if the passage is open on that side as well. This can be closed at the same sitting if you wish to. Recovery from surgery, timing of surgery and discharge from hospital are the similar for open surgery and laparoscopic surgery.
However, it is important to note that an open passage does not always mean that your child will get a hydrocele or hernia on the opposite side. There is no harm in opting for a second surgery later if your child at all develops a hernia on the opposite side.
Laparoscopic repairs have a slightly higher chance of recurrence as compared to open surgery. You can discuss the pros and cons in details with your doctor when you come for consultation.
Internal Ring in a Boy – Laparoscopic View

Internal ring in a Girl – Laparoscopic View

Open Internal Ring

Closed ring after surgery


Closed Internal Ring
What are the risks of surgery?
After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe. Some children develop swelling over the scrotum 24 hours after surgery. This gradually resolves on its own over the course of the next week.
What happens after the operation?
Your child will recover from the anaesthetic on the ward. Once he feels comfortable and has something to drink and eat, you will be able to take your child home. We recommend that you bring in some loose clothing for your child to wear home and for the next few days, as this will be a lot more comfortable.
What happens after you go home?
Your child should not have a bath or shower for three to five days after the operation. After this, it is fine for your child to have a shower, but try to avoid long baths as this may cause the scab to soften and fall off too early.
Your child should be ready to go back to school or nursery about a week after the operation.
The stitches will dissolve on their own within two weeks or so. You will need to visit hospital for a follow up check 7 – 10 days after surgery.
GUJARATI
સારણગાંઠ અને વધરાવળ
સારણગાંઠ ૨% બાળકોમાં જાવા મળે છે. બાળક માઁના ગર્ભમાં હોય ત્યારે બાળકના પેટમાં વૃષણની ગોળી બને છે, અને આ ગોળી પેટની બહાર નીકળી અને વૃષણ કોથળીમાં આવે છે. બાળકના જન્મ દરમિયાન આ રસ્તો સામાન્ય રીતે બંધ થઈ જાય છે, પરંતુ જ્યારે આ રસ્તો બંધ નથી થતો ત્યારે આંતરડા બહાર આવે છે અને સારણગાંઠ થાય છે. જા રસ્તો નાનો હોય અને ફક્ત પેટનું પાણી જ બહાર આવે, તો તેને વધરાવળ કહેવાય છે.
સારણગાંઠનું આૅપરેશન નિદાન થયા પછી તુરંતજ, બની શકે તેટલું વહેલું કરી દેવું જાઈએ. સારણગાંઠના આૅપરેશન માટે બાળકની ઉંમર કે બાળકના વજન જેવા કોઈ પરિબળ હોતા નથી. સારણગાંઠનો આૅપરેશન સિવાય બીજા કોઈ ઇલાજ નથી.
સામાન્ય રીતે બાળકને તપાસતાજ સારણગાંઠ અને વધરાવળની ખબર પડી જાય છે, તેના માટે કોઈ વિશેષ તપાસની જરૂર હોતી નથી. સોનોગ્રાફી કરાવવાનો ફાયદો એટલોજ છે કે એક બાજુ સારણગાંઠ હોય તેવા બાળકને સામેની બાજુએ રસ્તો ખુલ્લો છે કે નહીં તે ખબર પડે.
બાળકોને સારણગાંઠના આૅપરેશનમાં ફક્ત આ ખુલ્લો રહી ગયેલો રસ્તો જ બંધ કરવાનો હોય છે. તેમાં મોટા માણસોની જેમ જાળી મૂકવાની જરૂર હોતી નથી. સારણગાંઠનું આૅપરેશન જા ન કરવામાં આવે તો ૧૦% થી ૧૫% બાળકોમાં આંતરડું ફસાવાની શક્યતા રહેલી છે જે એક સીરિયસ પ્રોબ્લેમ છે. સારણગાંઠનું આૅપરેશન નિદાન બાદ બને તેટલું વહેલું કરાવવું જાઈએ. આથી વિપરીત બાળક ૧ વર્ષનું થાય ત્યાં સુધી વધરાવળ આપમેળે મટવાની શક્યતા રહેલી છે. •
HINDI
हर्निया और हाइड्रोसील
हर्निया और हाइड्रोसील एक आम्ा बि्ाम्ारी है जो २% ब्ाच्चों म्ों देखी जाती है। बच्चों में हर्निया और हाइड्रोसील का कारण मार्ग की आशंका है जिसके साथ वृषण पेट से निकल कर अंडकोश में आते हैं। ग्ाभ्ार् म्ों ब्ाच्चे के विकास के दौरान पेट के संकुचित म्ाग्ार् से आँत और पानी अंडकोष की थैली म्ों उतरता है, जिससे हर्निया और अंडकोष वृद्धि (हाइड्रोसील) की सम्ास्या होती है।
हर्निया और हाइड्रोसील की पहचान केवल चिकित्सीय परीक्षण द्वारा की जा सकती है। इसके लिए कोई विशेष जांच की आवश्यकता नहीं है। हालांकि, विपरीत दिशा में ट्रैक्ट की पेटेंसी को देखने के लिए अल्ट्रासाउंड स्कैन किया जा सकता है। इनगुनल हर्निया की पहचान होते ही बच्चे की आयु या उसके वजन की परवाह किये बिना जल्द से जल्द इसकी सर्जरी की जानी चाहिए। यदि हर्निया का इलाज समय पर न किया जाए तो आँतों में रूकावट या ऐंठन जैसी जटिलताएँ हो सकती है। साम्ान्यतः हर्निया से विपरीत, हाइड्रोसील १ वर्ष की उम्ा्र तक अपने आप ठीक हो जाता है, लेकिन १ वर्ष की उम्ा्र के ब्ाद ब्ाच्चे म्ों हाइड्रोसील की सम्ास्या रहने पर सर्जरी कराना आवश्यक है। सर्जरी (हर्नियोटॉमी) द्वारा पेटेंट स्थान को बंद कर दिया जाता है। वयस्कों की भांति बच्चों में जाली लगाने की आवश्यकता नहीं होती है। यह प्रक्रिया आमतौर पर एक दिन की देखभाल में की जाती है, जहाँ बच्चे को सुबह अस्पताल में भर्ती किया जाता है और शाम को घर भेज दिया जाता है। •
Hernia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a hernia?
A hernia describes a small piece of abdominal lining, and sometimes a section of the bowel, which bulges out through the abdominal wall. Both children and adults can have hernias. Sometimes it is present at birth. The hernia can look bigger when your child cries or strains.
What causes a hernia?
While your child was developing in the womb, the testicles were developing inside the abdomen. Towards the end of pregnancy, the testicle travel through a passage into the scrotum. When this passage fails to close the intestines in the abdomen tend to bulge out through it causing a hernia. Unlike adults, there is no generalized weakness of the abdominal wall that causes hernia in children. Sometimes the passage through which the testis has come down may be small allowing only fluid around the intestines to come down. This is called a ‘hydrocele’.
How common are hernias in children?
Hernias are more common in boys than girls. About one in 50 boys will have a hernia during their childhood. The condition is also more common in babies born prematurely.
Is it possible to prevent a hernia?
There is no known way of preventing a hernia.
How is a hernia diagnosed?
Your doctor will be able to diagnose the hernia by clinical examination as it appears as a characteristic lump in your child’s abdomen. Your child may not need any further diagnostic investigations.
How are hernias treated?
Your child will need a small operation. In many cases this can be carried out as day surgery – your child will arrive at the hospital, have the operation and be able to go home on the same day. Occasionally a child will need to stay in hospital for a day or two.
Hernias in children do not need placing a mesh or a net as is used in adult hernia repairs. The reason for this is that in children cause for the hernia is completely different than in adults where hernia is caused because of the weakness of the abdominal muscles.
At what age should the child have surgery for hernia?
Hernia should be operated earliest after the diagnosis, irrespective of your child’s age or weight. Untreated hernias are known to have complications in the form of obstruction where the intestine gets stuck and fails to go back in the abdomen. This will then require emergency treatment.
Remember: “SMALLER THE CHILD AND SMALLER THE HERNIA, GREATER THE RISK OF OBSTRUCTION.”


Children with obstructed hernias
What does the operation involve?
The operation is carried out under general anaesthetic and lasts for about 30 – 45 minutes. Once your child is asleep, the surgeon will make a small incision (cut) on the lower abdomen, The abdominal lining and piece of bowel will be pushed back into place. The open passage will be repaired and closed with stitches. These stitches will dissolve and will not have to be removed.
Can this operation done by laparoscopy?
Operation in hernia involves closing of the open passage through which the testis has come down. This can be done from outside as in open surgery or from inside by laparoscopy. If your child has got a hernia on one side, there is a 15 – 25 % chance that he / she may develop a hernia on the opposite side at a later date. With the help of laparoscopy we are able to look at the opposite side to see if the passage is open on that side as well. This can be closed at the same sitting if you wish to. Recovery from surgery, timing of surgery and discharge from hospital are the similar for open surgery and laparoscopic surgery.
However, it is important to note that an open passage does not always mean that your child will get a hernia. There is no harm in opting for a second surgery later if your child at all develops a hernia on the opposite side.
Laparoscopic repairs have a slightly higher chance of recurrence (i.e. the hernia coming back again) as compared to open hernias. You can discuss the pros and cons in details with your doctor when you come for consultation.
Internal Ring in a Boy – Laparoscopic View

Internal ring in a Girl – Laparoscopic View

Open Internal Ring

Closed ring after surgery


Closed Internal Ring

Scars after surgery
What are the risks of surgery?
After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe. Some children develop swelling over the scrotum 24 hours after surgery. This gradually resolves on its own over the course of the next week.
What happens after the operation?
Your child will recover from the anaesthetic on the ward. Once he feels comfortable and has something to drink and eat, you will be able to take your child home. We recommend that you bring in some loose clothing for your child to wear home and for the next few days, as this will be a lot more comfortable.
What happens after you go home?
Your child should not have a bath or shower for three to five days after the operation. After this, it is fine for your child to have a shower, but try to avoid long baths as this may cause the scab to soften and fall off too early.
Your child should be ready to go back to school or nursery about a week after the operation.
The stitches will dissolve on their own within two weeks or so. You will need to visit hospital for a follow up check 7 – 10 days after surgery.
Are there any long term effects of hernia repair?
Most hernia repair operations are successful. You should see an immediate reduction or the complete disappearance of the hernia.
One out of ten children develops a hernia on the opposite side of the body. This risk is doubled if your child has been born prematurely.
GUJARATI
સારણગાંઠ અને વધરાવળ
સારણગાંઠ ૨% બાળકોમાં જાવા મળે છે. બાળક માઁના ગર્ભમાં હોય ત્યારે બાળકના પેટમાં વૃષણની ગોળી બને છે, અને આ ગોળી પેટની બહાર નીકળી અને વૃષણ કોથળીમાં આવે છે. બાળકના જન્મ દરમિયાન આ રસ્તો સામાન્ય રીતે બંધ થઈ જાય છે, પરંતુ જ્યારે આ રસ્તો બંધ નથી થતો ત્યારે આંતરડા બહાર આવે છે અને સારણગાંઠ થાય છે. જા રસ્તો નાનો હોય અને ફક્ત પેટનું પાણી જ બહાર આવે, તો તેને વધરાવળ કહેવાય છે.
સારણગાંઠનું આૅપરેશન નિદાન થયા પછી તુરંતજ, બની શકે તેટલું વહેલું કરી દેવું જાઈએ. સારણગાંઠના આૅપરેશન માટે બાળકની ઉંમર કે બાળકના વજન જેવા કોઈ પરિબળ હોતા નથી. સારણગાંઠનો આૅપરેશન સિવાય બીજા કોઈ ઇલાજ નથી.
સામાન્ય રીતે બાળકને તપાસતાજ સારણગાંઠ અને વધરાવળની ખબર પડી જાય છે, તેના માટે કોઈ વિશેષ તપાસની જરૂર હોતી નથી. સોનોગ્રાફી કરાવવાનો ફાયદો એટલોજ છે કે એક બાજુ સારણગાંઠ હોય તેવા બાળકને સામેની બાજુએ રસ્તો ખુલ્લો છે કે નહીં તે ખબર પડે.
બાળકોને સારણગાંઠના આૅપરેશનમાં ફક્ત આ ખુલ્લો રહી ગયેલો રસ્તો જ બંધ કરવાનો હોય છે. તેમાં મોટા માણસોની જેમ જાળી મૂકવાની જરૂર હોતી નથી. સારણગાંઠનું આૅપરેશન જા ન કરવામાં આવે તો ૧૦% થી ૧૫% બાળકોમાં આંતરડું ફસાવાની શક્યતા રહેલી છે જે એક સીરિયસ પ્રોબ્લેમ છે. સારણગાંઠનું આૅપરેશન નિદાન બાદ બને તેટલું વહેલું કરાવવું જાઈએ. આથી વિપરીત બાળક ૧ વર્ષનું થાય ત્યાં સુધી વધરાવળ આપમેળે મટવાની શક્યતા રહેલી છે. •
HINDI
हर्निया और हाइड्रोसील
हर्निया और हाइड्रोसील एक आम्ा बि्ाम्ारी है जो २% ब्ाच्चों म्ों देखी जाती है। बच्चों में हर्निया और हाइड्रोसील का कारण मार्ग की आशंका है जिसके साथ वृषण पेट से निकल कर अंडकोश में आते हैं। ग्ाभ्ार् म्ों ब्ाच्चे के विकास के दौरान पेट के संकुचित म्ाग्ार् से आँत और पानी अंडकोष की थैली म्ों उतरता है, जिससे हर्निया और अंडकोष वृद्धि (हाइड्रोसील) की सम्ास्या होती है।
हर्निया और हाइड्रोसील की पहचान केवल चिकित्सीय परीक्षण द्वारा की जा सकती है। इसके लिए कोई विशेष जांच की आवश्यकता नहीं है। हालांकि, विपरीत दिशा में ट्रैक्ट की पेटेंसी को देखने के लिए अल्ट्रासाउंड स्कैन किया जा सकता है। इनगुनल हर्निया की पहचान होते ही बच्चे की आयु या उसके वजन की परवाह किये बिना जल्द से जल्द इसकी सर्जरी की जानी चाहिए। यदि हर्निया का इलाज समय पर न किया जाए तो आँतों में रूकावट या ऐंठन जैसी जटिलताएँ हो सकती है। साम्ान्यतः हर्निया से विपरीत, हाइड्रोसील १ वर्ष की उम्ा्र तक अपने आप ठीक हो जाता है, लेकिन १ वर्ष की उम्ा्र के ब्ाद ब्ाच्चे म्ों हाइड्रोसील की सम्ास्या रहने पर सर्जरी कराना आवश्यक है। सर्जरी (हर्नियोटॉमी) द्वारा पेटेंट स्थान को बंद कर दिया जाता है। वयस्कों की भांति बच्चों में जाली लगाने की आवश्यकता नहीं होती है। यह प्रक्रिया आमतौर पर एक दिन की देखभाल में की जाती है, जहाँ बच्चे को सुबह अस्पताल में भर्ती किया जाता है और शाम को घर भेज दिया जाता है। •
Haemangiomas
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a haemangioma?
A haemangioma is a collection of small blood vessels that form a lump under the skin. They are sometimes called ‘strawberry marks’ because the surface of a haemangioma looks a bit like the surface of a strawberry.
Haemangiomas can be superficial or deep. Some haemangiomas are a combination of the superficial and deep kinds, with a raised, red area on the surface of the skin, and a bluish swelling of abnormal blood vessels deeper in the skin.
What causes haemangiomas?
There is now some scientific evidence to suggest that nearly three quarters of haemangiomas may be caused by placental tissue. If a tiny piece of tissue from the placenta embeds into the baby’s developing tissue very early in pregnancy, this can start to grow on his or her skin after the baby is born, forming a haemangioma. We do not yet know fully what might cause the placental tissue to embed. Other theories have evolved, but more research is needed to confirm the causes of haemangiomas.
How common are haemangiomas?
About one in every ten babies has a haemangioma. They are more common in girls, in premature babies, low birth weight babies and multiple births, such as twins, triplets and quadruplets. Haemangiomas are not inherited, but because they are quite common, families often report another relative who has had a haemangioma in childhood.
What do haemangiomas look like?
Superficial haemangiomas are usually a raised, bright red area of skin, which feels quite warm because the abnormal blood vessels are close to the surface. A superficial haemangioma may appear initially as a small area of pale skin on which a red spot develops.
Deep haemangiomas may appear bluish in colour because the abnormal blood vessels are deeper in the skin. Sometimes they are not noticeable for the first few weeks, only appearing as a lump as the haemangioma grows; this is particularly true if the surface of the skin is not affected.
Haemangiomas are not usually present at birth but develop a few days or weeks later. They often grow rapidly in the first three months, increasing in size and sometimes in redness. It is unusual for haemangiomas to grow after six to ten months of age, when most haemangiomas tend to have a ‘rest period’ and then begin to shrink.





Where do haemangiomas occur?
Most children only develop one haemangioma, but occasionally, a child has multiple haemangiomas in various parts of the body. This seems to happen most often in twins or other multiple births.
Haemangiomas can appear anywhere on the body. The majority of haemangiomas appear on the head or neck, particularly on the cheek, lips or upper eyelid. Haemangiomas can also appear on the organs inside the body. This is most common when a child has multiple haemangiomas. The organ most commonly affected is the liver, but occasionally the airway, heart and brain may also be involved. Babies with multiple haemangiomas should have an ultrasound scan to confirm this or rule it out.
How are haemangiomas diagnosed?
Superficial haemangiomas are clearly noticeable and quite different to other types of birthmark so no special diagnostic tests are usually needed.
A child with a haemangioma near the eye, or a deep haemangioma, or one affecting the internal organs may require ultrasound and/or MRI scans to confirm the diagnosis, location, and also to check the depth of the affected blood vessels.
Looking after your child’s haemangioma
In most cases, haemangiomas just need looking after carefully.
As the blood vessels in a haemangioma are so near the surface of the skin, they can bleed if they are knocked or scratched. It is important to keep both your nails and your children’s nails cut short and buffed smooth, so that they don’t catch the surface of the haemangioma.
If the haemangioma starts to bleed, apply pressure over it with a clean handkerchief, cloth or tissue for at least five minutes. If blood soaks through the handkerchief, cloth or tissue, put another one on top and keep up the pressure. Do not take it off to have a look as this could start the bleeding again. If the bleeding continues, even after pressing down on the haemangioma for five minutes, go to your nearest doctor or contact us at the numbers provided.
The surface of the haemangioma is delicate and can be very dry, so avoid using bubble baths and rinse any soap or shampoo off carefully and pat the area gently afterwards. A thin layer of coconut oil or jelly (Vaseline etc.) put gently over the top of the haemangioma can stop it drying out.
Haemangiomas need protection from the sun because it can make them swell up for a while and look redder. You can use sun protection cream on all areas of exposed skin or use a hat to protect your child’s face and/or an umbrella when the baby is outdoors.
When might my child’s haemangioma need treatment?
Most haemangiomas do not require any treatment, but there are circumstances when treatment might be needed.
Occasionally, haemangiomas can form an open sore or ulcer, which is painful. Ulcers can become infected, so a visit to your doctor is important, as infected ulcerated areas may need treatment with antibiotics.
Haemangiomas that are around the mouth, in the nappy area or in natural folds of skin, like the armpit, ear and neck, are most likely to become ulcerated. This is often due to the friction of the two surfaces of skin rubbing together.
A child with a haemangioma around the mouth can suck or chew the lip/ haemangioma, and feeding, either by breast or bottle, can irritate the area further.
The nappy can rub haemangiomas in the nappy area, and contact with stools or urine makes the ulcer more painful. Wherever the haemangioma is located, an ulcer is painful, more likely to bleed, and more likely to become infected. In the long term, an ulcerated area is more likely to leave a scar than a non-ulcerated area of haemangioma.
If your child’s haemangioma develops an ulcer, it will need special attention until it heals. Keep the area clean by washing it twice a day, preferably in a bath or by pouring water over the area, and leave it to dry naturally.
Haemangiomas near the eye
Haemangiomas near the eye can have long-term effects on a child’s vision, so need to be checked by a specialist eye doctor (ophthalmologist). The haemangioma can press on the eyeball, causing it to go slightly out of shape, affecting how images are focused on the retina, which in turn alters the messages sent to the brain from the eye.
Haemangiomas that are blocking vision may need treatment with steroid medicines, given either as a liquid by mouth or in certain cases, as an injection directly into the haemangioma.


Haemangiomas on the lips
Haemangiomas on the lips often become ulcerated, and because ulcers are so painful, the child may not want to feed. Giving your child pain relief, before feeding can help. It can also help to put some Vaseline on the teat of the bottle (or around your nipple if you are breast feeding) will reduce friction and make feeding less painful.
Treatment options
There are lots of treatment options available; which option is suggested depends on the size and location of your child’s haemangioma.
Haemangiomas are painful when they are ulcerated, so your child may need regular pain relief.
Antibiotics
Antibiotics are recommended when an infection of an ulcerated haemangioma is suspected. These are usually given in the form of a cream or ointment to put directly on the ulcerated area, but widespread infection may need antibiotics in the form of tablets or a liquid as well. Occasionally, a child might need intravenous (into a vein) antibiotics and a stay in hospital.
Steroids
Steroids may be needed when the haemangioma is near the eye, lips, or nappy area to limit further growth. They are usually given as tablets or a liquid, and need to be given exactly according to instructions. When the haemangioma has shrunk enough, the dosage is gradually reduced, as it can be dangerous to stop steroids suddenly.
Laser Treatment
Laser treatment is sometimes used in the treatment of haemangiomas. It can be useful if used early in the development of flat haemangiomas, as it reduces the redness and also reduces the risk of ulceration. Laser treatment is also helpful if an ulcer has already developed, as it reduces the pain of the ulcer, makes it heal faster and reduces the risk of infection.
Immunosuppressive Medicines
A medicine called vincristine is occasionally used to treat specific types of haemangioma in infancy. This medicine is usually used to treat certain forms of cancer and leukaemia, but the doses used to treat these specific haemangiomas are much smaller. It is usually given alongside steroid medicines, particularly if they have not reduced the swelling.
Embolisation
Embolisation is a procedure to ‘block off’ certain blood vessels by injecting them with a ‘glue-like’ substance or beads that stop the blood flowing through them. Generally, this is only used when haemangiomas are very troublesome and other treatments have had little effect.
Surgery
Sometimes, surgery is an option for removing haemangiomas. The surgeon removes the haemangioma tissue and joins the healthy skin together. There will always be a scar with this sort of operation, but it varies depending on the location and size of the haemangioma. Sometimes, it is better to wait until the haemangioma has resolved completely, and see whether surgery is needed at that point.
What are the long term effects of a haemangioma?
Most haemangiomas will have disappeared completely by the age of five to seven years. Large haemangiomas may continue to get smaller until your child is about eight to ten years old.
Depending on the size and location of the haemangioma, there may be little sign it ever existed. Occasionally the affected area of skin might be a bit lighter in color than the rest of your child’s skin.
Large haemangiomas may distort the surrounding skin and even when they disappear, leave behind an area of stretched skin that looks puckered or wrinkled. This can often be improved with cosmetic surgery. Some children may have an uneven skin texture once the haemangioma has resolved. Some children may have some leftover fatty tissue.
GUJARATI
હિમેન્જયોમા (લોહીની નળીઓની ગાંઠ)
બાળકનું શરીર બે કોષમાંથી આકાર લેતું હોય છે. આ કોષમાંથી નવા-નવા કોષો ઉદ્ભવીને શરીરના અવયવો બનાવતા હોય છે. એમા લોહીની નળીઓ બનાવતા કોષ પણ હોય છે. અમુક પરિસ્થતીમાં લોહીની નળીઓ બનાવતા કોષ છુટા પડી જઈ પોતાનું એક અલગ ઝુમખું અથવા તો ગાંઠ બનાવતા હોય છે. જેને લોહીની નળીઓની ગાંઠ કે હિમેન્જયોમા કહેવામાં આવે છે. હિમેન્જયોમા બાળક જન્મતાની સાથે તુરત જ જાવામાં આવે છે. સામાન્ય રીતે હિમેન્જયોમા ‘લાખુ’ સમજવામાં આવે છે જે ખોટું છે. હિમેન્જયોમા કે લોહીની નળીઓની ગાંઠ પહેલા એક થી દોઢ વર્ષમાં ધીમે-ધીમે વધતી હોય છે અને બે વર્ષની ઉંમર પછી ધીરે-ધીરે તેની જાતે જ ઓછી થવા લાગતી હોય છે. પરંતુ જ્યારે હિમેન્જયોમા શરીરના અગત્યના અવયવો જેમ કે આંખ, નાક, મોઢું, પેશાબનો રસ્તો અથવા કાન વગેરે જગ્યાએ હોય અથવાતો હિમેન્જયોમા જા ઇન્ફેકશન જાણવામાં આવતું હોય તો તેની સારવાર વહેલી કરવાની સલાહ આપવામાં આવે છે. ઘણીવાર હિમેન્જયોમા શરીરના અગત્યના ભાગો ઉપર ખૂબ જ વધારે પડતાં પ્રસરીત હોય છે ત્યારે હિમેન્જયોમા ઓછા કરવા માટે અમુક દવાઓ પણ આપવામાં આવે છે. હિમેન્જયોમા દરેક વખતે સર્જરીથી જ મટતો હોય તેવું જરૂરી નથી. હિમેન્જયોમા અંદર રહેલી લોહીની નળીઓને સંકોચાવા માટે ઇન્જેક્શનનો પણ ઉપયોગ કરવામાં આવે છે. •





HINDI
हिमेंजीयोमा (खून की नलिकाओं की गांठ)
बच्चे का शरीर दो कोशिकाओं से आकार लेता है। इन कोशिकाओं से नयी-नयी कोशिकाएँ बनती हैं, जिनसे शरीर के विभिन्न अंग निर्मित होते हैं। इनमें खून की नलिकाएं बनानेवाली कोशिकाएँ भी होती हैं। कुछ परिस्थितियों में खून की नलिकाएं बनानेवाली कोशिकाएं अलग हो जाती है और एक अलग गुच्छा अथवा गांठ बनाती है। इन्हें खून की नलिकाओं की गांठ अथवा हिमेंजीयोमा कहते हैं। हिमेंजीयोमा बच्चे के जन्म के तुरंत बाद देखा जा सकता है। सामान्यतः हिमेंजीयोमा को ‘जन्म का निशान’ के रूप में समझा जाता है लेकिन यह गलत है। सामान्यतः हिमेंजीयोमा अथवा खून की नलिकाओं की गांठ प्रथम एक से डेढ़ वर्ष में धीरे-धीरे बढ़ती जाती है। और तत्पश्चात, दो वर्ष की आयु के बाद धीरे-धीरे अपने आप ही कम होने लगती है। लेकिन जब हिमेंजीयोमा शरीर के महत्वपूर्ण अंग जैसेकि आँखें, नाक, मुँह, मूत्रमार्ग अथवा कान आदि में होता है अथवा हिमेंजीयोमा में यदि संक्रमण पाया जाता है तो उसका उपचार शीघ्र ही करने की सलाह दी जाती है। कई बार हिमेंजीयोमा शरीर के महत्वपूर्ण अंगों पर बहुत अधिक फैलता है, तब हिमेंजीयोमा को कम करने के लिए कुछ दवाइयाँ भी दी जाती है। यह आवश्यक नहीं है कि हिमेंजीयोमा सर्जरी से हमेशा ठीक होगा। कई बार हिमेंजीयोमा में अंदरूनी खून की नलिकाओं को संकुचित करने के लिए इंजेक्शन का प्रयोग भी किया जाता है। •
Hirschsprung’s Disease
Hirschsprung’s disease is a rare disorder of the bowel, most commonly the large bowel (colon), which can lead to severe constipation and intestinal obstruction. Hirschsprung’s disease affects one in every 5,000 babies.
Normally, the muscles in the bowel squeeze rhythmically to push faeces (stools) through to the rectum. In Hirschsprung’s disease, the nerves that control these muscles (ganglion cells) are missing from part of the bowel. This means that stools cannot be pushed through the bowel in the usual way.
The length of the affected part of bowel varies from child to child. Most commonly the rectum and/or sigmoid colon (the last parts of the large bowel) are affected. The entire colon is affected only very rarely.
What causes Hirschsprung’s disease?
Hirschsprung’s disease is a congenital (present at birth) disorder. While your baby was developing in the womb, the nerve cells did not develop through the full length of the bowel. We do not know what caused this to occur, but it was not due to anything that happened during pregnancy. A number of genes causing Hirschsprung’s disease have now been identified, although not all children have a specific genetic mutation.
What are the signs and symptoms of Hirschsprung’s disease?
The main symptom of Hirschsprung’s disease is constipation, which cannot be treated using laxatives or softeners. This occurs because faeces (stools) are pushed through the bowel until they reach the affected part. As this part of the bowel cannot squeeze rhythmically to push the faeces (stools) through the bowel, the faeces cannot move any further. As more food is digested and turned into faeces, the bowel becomes blocked causing discomfort and a swollen abdomen.
Often babies with Hirschsprung’s disease do not pass meconium – the dark faeces passed in the first day of life. Other symptoms include a swollen abdomen and green vomiting (bile).
How is Hirschsprung’s disease diagnosed?
Hirschsprung’s disease can be suggested on x-rays, either a plain x-ray or a contrast / barium enema. Some sections of the bowel look very bulged but the section after looks narrower than usual.
It is more reliably diagnosed by taking a small piece of tissue from the bowel to examine under a microscope. This is called a rectal biopsy. If the piece of tissue does not have any ganglion cells, this means Hirschsprung’s disease has been diagnosed.
How can Hirschsprung’s disease be treated?
How Hirschsprung’s disease is treated depends on the age at which your child is diagnosed and how well your child is generally. All children will require surgery at some stage.
Some children’s constipation can be helped on a short-term basis using enemas (bowel washouts), where a thin tube is inserted into your child’s bottom and filled with a warm saltwater solution. This softens the faeces and flushes it from your child’s bowel.
If a child is newborn or generally well, we may suggest treating the Hirschsprung’s Diseaselaparoscopically in one operation called a ‘laparoscopic assisted pull-through’ operation. This is where the affected part of the bowel and then connects the healthy section directly to the anus to allow faeces to be passed.
If a child is older or not very well, we may suggest a staged operation. First, we will create an artificial opening (stoma) for the bowel as a temporary measure. This will allow your child to pass faeces through the stoma, allowing their health to improve before the pull-through operation. In the event of the child already having a stoma prior to visiting this hospital, a laparoscopic pull through operation is still possible.
Are there any alternatives other than surgery ?
No. Eventually, all children will need surgery to treat the Hirschsprung’s disease.
What happens before the operation?
The child will need to come into hospital two – three days before the operation. This is so your child’s bowel can be empty of faeces(stools) and ready for the operation. He or she may have laxatives or a bowel washout, and will be allowed to drink clear fluids for 24 hours before the operation.
What does the operation involve?
The surgeon will identify the part of the bowel missing the ganglion cells using a series of biopsies and remove it. Once they have removed the affected portion of bowel, they will attach the end to the anus to create a working bowel, with enough nerve cells to control the muscles so that your child can pass faeces as usual.
If your child is having a staged repair, a stoma may need to be formed first so that they can get better before they have the pull-through operation. As with the pull-through operation, the surgeon will identify the affected portion of bowel using a series of biopsies and remove it. They will then bring the end to an artificial opening in your child’s abdomen called a stoma. This means faeces can be pushed through the bowel to the stoma, where they are collected in a bag to be disposed of later. Some weeks later, in another operation, the surgeon will remove the part of the bowel missing the ganglion cells as in the ‘pull-through’ operation.
The stoma will be closed when your child has had the pull through operation, either during the same procedure or a few weeks or months later.
Are there any risks?
Every anaesthetic carries a risk of complications, but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. All surgery carries a small risk of bleeding during or after the operation. There is a very small chance that the bowel could leak into the abdominal cavity. If this occurs, your child will need a stoma as this reduces the risk of developing a serious infection called peritonitis.
What happens afterwards?
The child will come back to the ward to recover. We will keep your child as comfortable as possible by giving regular pain relieving medications. For the first few days, the pain relief will usually be given through a ‘drip’ and then, when your child is more comfortable, in the form of medicines to be swallowed. For the first few days, your child will need a ‘drip’ of fluids until they feel like eating and drinking again. This will also allow the bowel to rest and start to heal. You will be able to go home once he or she is comfortable.
When you get home
After the pull-through operation, your child may have soreness around the anus when passing faeces normally. You can try using coconut oil to clean your child’s bottom, as this will also ease any discomfort. It will also help to use nappy cream after each nappy change. We will discuss this further with you before you go home. Whenever possible, leave your child’s bottom open to the air as this will help it heal too.
Are there any long-term effects of the operation?
Although the pull-through operation is very successful at treating Hirschsprung’s disease some children develop problems afterwards, some of which we are able to treat.
Constipation may be seen after the pullthrough operation, which may require treatment with medications. Toilet training in children who have had the pull-through operation may be delayed, mainly due to having to learn to coordinate the nerves and muscles in the rectum and anus. Children should follow a normal balanced diet after the pull-through operation.
Sometimes children with Hirschsprung’s disease can develop an infection called Hirschsprung’senterocolitis. If your child develops diarrhoea.If not responding to oral medications, the child may need to come into hospital for a short stay to receive treatment with fluids and antibiotics.
What is the outlook for children with Hirschsprung’s disease?
Overall, the outlook for children with Hirschsprung’s disease is good, with the majority growing up to live normal lives, working and raising a family.If you have a child with Hirschsprung’s disease, future children may be at increased risk of also having this condition.
Hematemesis (Blood in Vomit)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
BLOOD IN VOMIT (HEMATEMESIS)
Hematemesis (Blood in vomit) is a serious challenge for both the child and its doctor.
New born children: Blood in the vomit of a newborn child is commonly due to deficiency of vitamin K or secondary to swallowed maternal blood from a cracked nipple while breast feeding. This can also happen due to stress gastritis secondary to a stressful delivery.
1-2 years : Bleeding from the gums is swallowed by the child and is brought out in the vomit. Excessive use of pain killers or NSAID’s may cause gastritis and hematemesis. Food of a particular color or type may falsely raise the alarm of hematemesis.
Some children have severe gastroesophageal reflux (retrograde passage of stomach contents into the oesophagus). This may cause erosions in the inner lining of the oesophagus leading to hematemesis.
5-6 years: Gastroesophageal reflux and reflux oesophagitis can also cause hematemesis in this age. Another common cause for hematemesis in older children is oesophageal varices secondary to Portal Hypertension. This bleeding can be either bright red or coffee coloured. This is a serious problem and needs urgent and thorough treatment. These children need urgent hospitalization and endoscopy / open surgery are necessary for definitive treatment. ●
GUJARATI
ઉલ્ટીમાં લોહી પડવું
લોહીની ઉલ્ટી થવી એ બાળક અને ડાžટર માટે ગંભીર સમસ્યા છે.
નવજાત બાળકઃ આ ઉંમરમાં ઉલ્ટીમાં લોહી આવવાનું કારણ વિટામિન ‘કે’ ની ઉણપ,માતાનાં સ્તનમાં પડેલ ચીરામાંથી નીકળતું લોહી (ધાવણ દરમ્યાન પેટમાં જાય છે) અથવા તો સ્ટ્રેસફૂલ ડિલિવરીનું હોય છે.
એક-બે વર્ષઃ આ ઉંમરનાં બાળકોમાં દાંતના પેઢામાંથી નીકળતું લોહી ગળી જવાને કારણે અથવા કોઈ દુઃખાવા- તાવ માટેની દવા લેવાથી અથવા કલરવાળો ખોરાક ખાવાથી, લોહી રૂપે ઉલ્ટીમાં આવે છે. ઘણા બાળકોમાં હોજરી અને અન્નનળી વચ્ચેનો વાલ્વ લૂઝ હોવાથી હોજરીનું એસીડ અન્નનળીમાં ‘બેક મારે’ છે. આને ‘ગેસ્ટ્રોઈસોફેજિયલ રીફ્લક્ષ’ કહે છે. હોજરીના એસિડથી અન્નનળીમાં ઉઝરડા/ચાંદા પડવાના કારણે પણ ઉલ્ટીમાં લોહી આવે છે.
૫-૬ વર્ષ અને મોટી ઉંમરઃ આ બાળકોમાં વધુ પડતી લોહીની ઉલ્ટીનું કારણ અન્નનળીમાં ફૂલી ગયેલી લોહીની નળી (જેનું કારણ પોરટલ હાયપર ટેન્સન હોય છે) ફાટવાથી થાય છે. આ બીમારી સીરિયસ પ્રકારની હોય છે જેની યોગ્ય સારવાર કરાવવી પડે છે. આ જાતની લોહીની ઉલ્ટી કોફી કલરની અથવા લાલ કલરની હોય છે. મોટા બાળકોમાં પણ ગેસ્ટ્રોઈસોફેજિયલ રીફ્લક્ષના કારણે ઉલ્ટીમાં લોહી આવી શકે છે.
બાળકને તાત્કાલિક દાખલ કરી જરૂર પડે લોહી આપી એન્ડોસ્કોપી કરાવવી પડે છે. •
HINDI
उल्टी में खून
खून की उल्टी होना, बच्चा और डॉक्टर दोनों के लिए एक गंभीर चुनौतीपूर्ण समस्या है।
नवजात शिशुः आमतौर पर नवजात शिशु की उल्टी में खून आने का कारण विटामिन K की कमी या स्तनपान के दौरान माँ के स्तन से निकले खून को पीने से होती है। तनावपूर्ण डिलीवरी भी इसका कारण हो सकता है।
१ से २ वर्ष के बच्चों के दांत के पेढू से निकलने वाला खून गटकने के कारण बाद में उल्टी में निकलता है। दर्द से राहत के लिए अतिरिक्त मात्रा में दवाई लेने पर या किसी विशेष रंग वाला भोजन करने पर वह उल्टी में खून जैसा लगता है।
५ से ६ वर्ष और उससे अधिक आयु के बच्चों की उल्टी में खून की मात्रा अधिक होने का कारण आहारनली में फूली हुई खून की नली का टूट जाना है(पोरटल हायपर टेन्शन इसका कारण है)। यह उल्टी हल्के लाल रंग या कॉफी रंग की हो सकती है, जो कि काफी गंभीर बीमारी है और इसका तत्काल इलाज किये जाने की आवश्यकता है। ऐसे में बच्चे को तुरंत अस्पताल में भर्ती करके एन्डोस्कोपी करने की जरूरत है।•
Hematuria (Blood in Urine)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Hematuria
Hematuria is presence of red blood cells in the urine. Microscopic hematuria means blood is detected only with a microscope, while gross hematuria means urine appears red or like the colour of tea or cola.
Causes of hematuria?
- Abnormal structures in the urinary tract e.g. stones, tumors etc.
- Inherited diseases e.g. bleeding disorders, polycystic kidneys, sickle cell disorder etc.
- Mineral imbalances in the urine e.g. hypercalciuria
- Glomerulonephritis
- Idiopathic i.e. no specific cause can be found
Evaluation of Hematuria:
- An ultrasound of the urinary system
- Urine should be checked for protein and may be checked for calcium and creatinine.
- Blood tests to determine kidney function and other tests may be performed.
- If all tests are negative and urine remains blood stained, an endoscopic examination of the urinary tract may also be necessary.
Children who have microscopic hematuria with high blood pressure, abnormal blood tests, or high levels of protein in the urine may need to have a kidney biopsy. ●
GUJARATI
પેશાબમાં લોહી પડવું :
‘પેશાબમાં લોહી પડવું’ એ બાળક અને માતાપિતા માટે ખૂબ ચિંતાનો વિષય છે. કોઈ દવાની આડ અસર અથવા હીમોગ્લોબીન જવાથી પણ પેશાબ લોહી જેવો દેખાય છે.
મુખ્ય કારણો :
૧.કિડનીની ગાંઠ
૨. રક્તસ્ત્રાવ ડિસઓર્ડર
૩. પેશાબમાં ઇન્ફેક્શન
૪.નેફ્રાઈટીસ
૫. પેશાબમાં પથરી
મુખ્ય તપાસ:
ડાક્ટરી તપાસ કર્યા પછી જરૂરી લેબોરેટરી અને એક્સ-રે /સોનોગ્રાફી તપાસ કરાવવી પડે છે. ઘણીવાર દૂરબીનથી પેશાબની નળી અને કોથળીની તપાસ પણ કરવામાં આવે છે. •
HINDI
रक्तमेह (हीमेचुरीया)
मूत्र में लाल रक्त कणों की उपस्थिति को हीमेचुरीया कहते हैं। सामान्यतः गुर्दे खून को मूत्र में प्रवेश करने से रोकते हैं। हीमेचुरीया की स्थिति में, मूत्रमार्ग के फिल्टर अथवा अन्य अंग खून को रीस कर मूत्र में प्रवेश करने देते हैं। माईकोस्कोपिक हीमेचुरीया में केवल माईक्रोस्कोप के द्वारा ही खून के होने का पता चलता है, जबकि ग्ा्रॉस हिमेचुरीया में मूत्र रंग लाल अथवा चाय के रंग अथवा कोला जैसा दिखायी पड़ता है।
हीमेचुरीया के कारण :
मूत्रमार्ग में पथरी, गांठ आदि, जैसी असामान्य संरचनाओं का होना।
रक्तस्त्राव विकार, पॉलिसीस्टिक गुर्दे, सिकल सैल विकार जैसे रोग।
मूत्र में खनीजों का असंतुलन जैसे, हाईपरकॅल्कुरीया।
ग्लोमेरूलोनेफ्रीटिस
हीमेचुरीया का मूल्यांकन
मूत्र प्राणाली का अल्ट्रासाउंड। प्रोटीन, कैल्शीयम और क्रियटीनाइन के लिए मूत्र की जांच। गुर्दे के कार्यों की जांच के लिए खून की जांच और अन्य जांच। यदि सभी जांच का परिणाम नेगेटीव है और फिर भी मूत्र में खून पाया जाता है तो मूत्रमार्ग की एंडोस्कोपिक जांच करनी आवश्यक हो सकती है। माइक्रोस्कोपिक हीमेचुरीया वाले बच्चे की गुर्दे की बायोप्सी करने की आवश्यकता हो सकती है।•
Hernia (Inguinal Hernia)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a hernia?
A hernia describes a small piece of abdominal lining, and sometimes a section of the bowel, which bulges out through the abdominal wall. Both children and adults can have hernias. Sometimes it is present at birth. The hernia can look bigger when your child cries or strains.
What causes a hernia?
While your child was developing in the womb, the testicles were developing inside the abdomen. Towards the end of pregnancy, the testicle travel through a passage into the scrotum. When this passage fails to close the intestines in the abdomen tend to bulge out through it causing a hernia. Unlike adults, there is no generalized weakness of the abdominal wall that causes hernia in children. Sometimes the passage through which the testis has come down may be small allowing only fluid around the intestines to come down. This is called a ‘hydrocele’.
How common are hernias in children?
Hernias are more common in boys than girls. About one in 50 boys will have a hernia during their childhood. The condition is also more common in babies born prematurely.
Is it possible to prevent a hernia?
There is no known way of preventing a hernia.
How is a hernia diagnosed?
Your doctor will be able to diagnose the hernia by clinical examination as it appears as a characteristic lump in your child’s abdomen. Your child may not need any further diagnostic investigations.
How are hernias treated?
Your child will need a small operation. In many cases this can be carried out as day surgery – your child will arrive at the hospital, have the operation and be able to go home on the same day. Occasionally a child will need to stay in hospital for a day or two.
Hernias in children do not need placing a mesh or a net as is used in adult hernia repairs. The reason for this is that in children cause for the hernia is completely different than in adults where hernia is caused because of the weakness of the abdominal muscles.
At what age should the child have surgery for hernia?
Hernia should be operated earliest after the diagnosis, irrespective of your child’s age or weight. Untreated hernias are known to have complications in the form of obstruction where the intestine gets stuck and fails to go back in the abdomen. This will then require emergency treatment.
Remember: “SMALLER THE CHILD AND SMALLER THE HERNIA, GREATER THE RISK OF OBSTRUCTION.”


Children with obstructed hernias
What does the operation involve?
The operation is carried out under general anaesthetic and lasts for about 30 – 45 minutes. Once your child is asleep, the surgeon will make a small incision (cut) on the lower abdomen, The abdominal lining and piece of bowel will be pushed back into place. The open passage will be repaired and closed with stitches. These stitches will dissolve and will not have to be removed.
Can this operation done by laparoscopy?
Operation in hernia involves closing of the open passage through which the testis has come down. This can be done from outside as in open surgery or from inside by laparoscopy. If your child has got a hernia on one side, there is a 15 – 25 % chance that he / she may develop a hernia on the opposite side at a later date. With the help of laparoscopy we are able to look at the opposite side to see if the passage is open on that side as well. This can be closed at the same sitting if you wish to. Recovery from surgery, timing of surgery and discharge from hospital are the similar for open surgery and laparoscopic surgery.
However, it is important to note that an open passage does not always mean that your child will get a hernia. There is no harm in opting for a second surgery later if your child at all develops a hernia on the opposite side.
Laparoscopic repairs have a slightly higher chance of recurrence (i.e. the hernia coming back again) as compared to open hernias. You can discuss the pros and cons in details with your doctor when you come for consultation.
Internal Ring in a Boy – Laparoscopic View

Internal ring in a Girl – Laparoscopic View

Open Internal Ring

Closed ring after surgery


Closed Internal Ring

Scars after surgery
What are the risks of surgery?
After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe. Some children develop swelling over the scrotum 24 hours after surgery. This gradually resolves on its own over the course of the next week.
What happens after the operation?
Your child will recover from the anaesthetic on the ward. Once he feels comfortable and has something to drink and eat, you will be able to take your child home. We recommend that you bring in some loose clothing for your child to wear home and for the next few days, as this will be a lot more comfortable.
What happens after you go home?
Your child should not have a bath or shower for three to five days after the operation. After this, it is fine for your child to have a shower, but try to avoid long baths as this may cause the scab to soften and fall off too early.
Your child should be ready to go back to school or nursery about a week after the operation.
The stitches will dissolve on their own within two weeks or so. You will need to visit hospital for a follow up check 7 – 10 days after surgery.
Are there any long term effects of hernia repair?
Most hernia repair operations are successful. You should see an immediate reduction or the complete disappearance of the hernia.
One out of ten children develops a hernia on the opposite side of the body. This risk is doubled if your child has been born prematurely.
GUJARATI
સારણગાંઠ અને વધરાવળ
સારણગાંઠ ૨% બાળકોમાં જાવા મળે છે. બાળક માઁના ગર્ભમાં હોય ત્યારે બાળકના પેટમાં વૃષણની ગોળી બને છે, અને આ ગોળી પેટની બહાર નીકળી અને વૃષણ કોથળીમાં આવે છે. બાળકના જન્મ દરમિયાન આ રસ્તો સામાન્ય રીતે બંધ થઈ જાય છે, પરંતુ જ્યારે આ રસ્તો બંધ નથી થતો ત્યારે આંતરડા બહાર આવે છે અને સારણગાંઠ થાય છે. જા રસ્તો નાનો હોય અને ફક્ત પેટનું પાણી જ બહાર આવે, તો તેને વધરાવળ કહેવાય છે.
સારણગાંઠનું આૅપરેશન નિદાન થયા પછી તુરંતજ, બની શકે તેટલું વહેલું કરી દેવું જાઈએ. સારણગાંઠના આૅપરેશન માટે બાળકની ઉંમર કે બાળકના વજન જેવા કોઈ પરિબળ હોતા નથી. સારણગાંઠનો આૅપરેશન સિવાય બીજા કોઈ ઇલાજ નથી.
સામાન્ય રીતે બાળકને તપાસતાજ સારણગાંઠ અને વધરાવળની ખબર પડી જાય છે, તેના માટે કોઈ વિશેષ તપાસની જરૂર હોતી નથી. સોનોગ્રાફી કરાવવાનો ફાયદો એટલોજ છે કે એક બાજુ સારણગાંઠ હોય તેવા બાળકને સામેની બાજુએ રસ્તો ખુલ્લો છે કે નહીં તે ખબર પડે.
બાળકોને સારણગાંઠના આૅપરેશનમાં ફક્ત આ ખુલ્લો રહી ગયેલો રસ્તો જ બંધ કરવાનો હોય છે. તેમાં મોટા માણસોની જેમ જાળી મૂકવાની જરૂર હોતી નથી. સારણગાંઠનું આૅપરેશન જા ન કરવામાં આવે તો ૧૦% થી ૧૫% બાળકોમાં આંતરડું ફસાવાની શક્યતા રહેલી છે જે એક સીરિયસ પ્રોબ્લેમ છે. સારણગાંઠનું આૅપરેશન નિદાન બાદ બને તેટલું વહેલું કરાવવું જાઈએ. આથી વિપરીત બાળક ૧ વર્ષનું થાય ત્યાં સુધી વધરાવળ આપમેળે મટવાની શક્યતા રહેલી છે. •
HINDI
हर्निया और हाइड्रोसील
हर्निया और हाइड्रोसील एक आम्ा बि्ाम्ारी है जो २% ब्ाच्चों म्ों देखी जाती है। बच्चों में हर्निया और हाइड्रोसील का कारण मार्ग की आशंका है जिसके साथ वृषण पेट से निकल कर अंडकोश में आते हैं। ग्ाभ्ार् म्ों ब्ाच्चे के विकास के दौरान पेट के संकुचित म्ाग्ार् से आँत और पानी अंडकोष की थैली म्ों उतरता है, जिससे हर्निया और अंडकोष वृद्धि (हाइड्रोसील) की सम्ास्या होती है।
हर्निया और हाइड्रोसील की पहचान केवल चिकित्सीय परीक्षण द्वारा की जा सकती है। इसके लिए कोई विशेष जांच की आवश्यकता नहीं है। हालांकि, विपरीत दिशा में ट्रैक्ट की पेटेंसी को देखने के लिए अल्ट्रासाउंड स्कैन किया जा सकता है। इनगुनल हर्निया की पहचान होते ही बच्चे की आयु या उसके वजन की परवाह किये बिना जल्द से जल्द इसकी सर्जरी की जानी चाहिए। यदि हर्निया का इलाज समय पर न किया जाए तो आँतों में रूकावट या ऐंठन जैसी जटिलताएँ हो सकती है। साम्ान्यतः हर्निया से विपरीत, हाइड्रोसील १ वर्ष की उम्ा्र तक अपने आप ठीक हो जाता है, लेकिन १ वर्ष की उम्ा्र के ब्ाद ब्ाच्चे म्ों हाइड्रोसील की सम्ास्या रहने पर सर्जरी कराना आवश्यक है। सर्जरी (हर्नियोटॉमी) द्वारा पेटेंट स्थान को बंद कर दिया जाता है। वयस्कों की भांति बच्चों में जाली लगाने की आवश्यकता नहीं होती है। यह प्रक्रिया आमतौर पर एक दिन की देखभाल में की जाती है, जहाँ बच्चे को सुबह अस्पताल में भर्ती किया जाता है और शाम को घर भेज दिया जाता है। •
Intussusception
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is intussusception?
Intussusception is a condition where the bowel ‘telescopes’ in on itself. This causes the bowel walls to press on one another, blocking the bowel. This can lead to reduced blood flow to that part of the bowel.


Picture of Intussusception with bowel in bowl appearance
What are the symptoms?
The main symptom of intussusception is severe abdominal pain that comes and goes. Each episode (time) tends to last two to three minutes. After 12 hours or so, the pain become more constant, and your child will usually go off food and may vomit.
Your child’s stools may contain blood and mucus. Due to the vomiting, your child may become dehydrated. Symptoms of dehydration include lethargy (tiredness), reduced urine output than usual. Your child may also have a high temperature and a swollen stomach.
How is intussusception diagnosed?
Your doctor will generally be able to feel the intussusception by pressing gently on the abdomen to feel for the swollen bowel. An ultrasound scan will usually confirm the diagnosis.
What causes intussusception?
We are not sure what causes the bowel to telescope in on itself, but there may be some link to infections.
How common is intussusception and whom does it affect?
Intussusception is the most common cause of bowel blockage in infants and young children. It tends to happen between the ages of three and 18 months.
How intussusception is treated and are there any alternatives?
Intussusception can cause reduced blood flow to part of the bowel, which would stop it functioning properly and can also lead to problems with infection. The effects of intussusception, like dehydration due to vomiting, can become serious quite quickly in children, so the condition needs emergency treatment.
If your child is dehydrated, he or she will need a drip of fluids for a while before treatment starts. Your child will also need a nasogastric tube, which is passed up the nose, down the food-pipe and into the stomach. This will drain off the stomach and bowel contents, and ‘vent’ any air that has built up, which will make your child more comfortable.
An enema is usually the first treatment. A tube is inserted into your child’s bottom and air or oxygen is released into the bowel. This works by expanding the bowel, so that the intussusception corrects itself. If the enema works well, you will be able to return home in a day or so.
If your child is not well enough to have an enema, or if the enema did not reduce the intussusception, your child will need an operation under general anaesthetic.
What does the operation involve?
Your child’s surgeon will gently squeeze the bowel to push out the inner segment. He or she will also examine the bowel to see if there is blood flow to that part of the bowel and if it looks healthy. Nowadays, this operation can also be done with the help of laparoscopy in selected cases.
The surgeon will remove any part of the bowel where tissue has died due to the lack of blood flow. The amount can vary, but the surgeon will leave as much bowel as possible.
What happens afterwards?
Your child will not be able to feed for about 24 – 48 hours which will allow the bowel to recover. He or she will continue to have a drip of fluids and the nasogastric tube to drain off the stomach contents.
After a couple of days, your child will be able to feed again, starting with small amounts and increasing the amount as he or she tolerates it. When your child’s bowel has recovered completely, you will be able to feed him or her solids. The doctors will let you know when this is likely.
Your child will be able to go home once he or she is feeding well. This is usually about 3-5 days or so after the operation.
What is the outlook for children with intussusception?
The outlook is good, with the majority of children having no further bowel problems. However, intussusception can come back in a small number of children, which will require further treatment either by enema or an operation.
GUJARATI
ઇન્ટુસસેપ્શન (એક આંતરડું બીજા આંતરડામાં ભરાઈ જાય)
ઇન્ટુસસેપ્શન નાના બાળકોના (ખાસ કરીને ૩ માસથી ૨ વર્ષ) આંતરડામાં થતી અને ઇમરજન્સી સારવાર માંગી લેતી બીમારી છે. આમાં સામાન્ય રીતે નાનું આંતરડું મોટા આંતરડાની અંદર ઘૂસતું જાય છે અને આંતરડામાં અવરોધ કરે છે. અરજન્ટ ટ્રીટમેન્ટ ન મળતાં આંતરડાનો ભાગ લોહીના અભાવે મરી જાય (ગેંગરીન થાય છે) જે આૅપરેશન દ્વારા કાઢી નાંખવો પડે છે.
તંદુરસ્ત બાળક (જેને શરદીની બીમારી થઈ હોય) જે એકાએક ચૂકંથી દર ૫-૭ મિનીટે સખત રડે, ઉલ્ટી કરે અને સંડાસમાં લોહી-ચિકાશ આવે તો સમજવું બાળકને ઇન્ટુસસેપ્શન હોઈ શકે અને અરજન્ટ ડાક્ટરની સલાહ લેવી.
નિદાન કરવાની રીત :
૧) બાળકને થતી ટીપીકલ તકલીફ
૨) પેટ ફૂલેલું ન હોય (શરૂઆતની સ્ટેજમાં) અને પેટમાં કેળા જેવી ગાંઠ માલૂમ પડે.
૩) સોનોગ્રાફીથી લગભગ ૧૦૦% નિદાન આવે છે.
ટ્રીટમેન્ટ શું કરી શકાય?
બાળકોનાં સર્જનની અરજન્ટ સલાહ લેવી
૧) પહેલાં ૧૨ થી ૨૪ કલાકમાં સંડાસની જગ્યાએ હવા અથવા સેલાઇનનાં પ્રેશર દ્વારા એક્ષ રે વિભાગમાં આંતરડું પાછું ધકેલી શકાય.
૨) મોડા આવનાર બાળકમાં લોપ્રોસ્કોપી દ્વારા અથવા આ૨પરેશન દ્વારા જરૂરી સારવાર કરી શકાય છે. •
HINDI
इंटुससेप्शन (एक आंत का दूसरे आंत में फंस जाना)
इंटुससेप्शन छोटे बच्चों (विशेष कर ३ माह से २ वर्ष) की आंतों में होनेवाली तथा आपातकालीन उपचार की आवश्यकता वाली बीमारी है। इसमें सामान्यतया छोटी आंत बड़ी आंत के अंदर घुस जाती है और आंतों में अवरोध उत्पन्न करती है। तुरंत उपचार न किए जाने पर खून की कमी के कारण आंतों का भाग मर जाता है (गेंगरीन) और इसे ऑपरेशन के द्वारा निकाल देना पड़ता है।
स्वस्थ बच्चा (जिसे साधारण सर्दी की बीमारी हो सकती है) यदि अचानक पेट दर्द से हर ५-७ मिनट में बहुत ज्यादा रोने लगे, उल्टी करे और खून एवं चिकनाई के साथ मल आए तो समझ लेना चाहिए कि बच्चे को इंटुससेप्शन हो सकता है और तुरंत डॉक्टर की सलाह लेनी चाहिए।
निदान का तरीका :
१) बच्चे को होने वाली टीपीकल तकलीफ
२) पेट फूला हुआ न हो (शुरुआती चरण में) और पेट में केले जैसी गांठ महसूस हो
३) सोनोग्राफी से करीब-करीब १०० % निदान सम्भव है।
क्या उपचार करना चाहिए ?
बाल सर्जन से तुरंत संपर्क करना चाहिए
१) प्रथम १२ से २४ घंटों में गुदा स्थल में हवा अथवा सेलाइन के दबाव के द्वारा आंत को दुबारा पीछे धकेला जा सकता है।
२) यदि बच्चा डॉक्टर के पास देर से आता है तो लेप्रोस्कोपी द्वारा अथवा ओपन ऑपरेशन द्वारा आवश्यक उपचार किया जा सकता है। •
Inguinal Hernia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a hernia?
A hernia describes a small piece of abdominal lining, and sometimes a section of the bowel, which bulges out through the abdominal wall. Both children and adults can have hernias. Sometimes it is present at birth. The hernia can look bigger when your child cries or strains.
What causes a hernia?
While your child was developing in the womb, the testicles were developing inside the abdomen. Towards the end of pregnancy, the testicle travel through a passage into the scrotum. When this passage fails to close the intestines in the abdomen tend to bulge out through it causing a hernia. Unlike adults, there is no generalized weakness of the abdominal wall that causes hernia in children. Sometimes the passage through which the testis has come down may be small allowing only fluid around the intestines to come down. This is called a ‘hydrocele’.
How common are hernias in children?
Hernias are more common in boys than girls. About one in 50 boys will have a hernia during their childhood. The condition is also more common in babies born prematurely.
Is it possible to prevent a hernia?
There is no known way of preventing a hernia.
How is a hernia diagnosed?
Your doctor will be able to diagnose the hernia by clinical examination as it appears as a characteristic lump in your child’s abdomen. Your child may not need any further diagnostic investigations.
How are hernias treated?
Your child will need a small operation. In many cases this can be carried out as day surgery – your child will arrive at the hospital, have the operation and be able to go home on the same day. Occasionally a child will need to stay in hospital for a day or two.
Hernias in children do not need placing a mesh or a net as is used in adult hernia repairs. The reason for this is that in children cause for the hernia is completely different than in adults where hernia is caused because of the weakness of the abdominal muscles.
At what age should the child have surgery for hernia?
Hernia should be operated earliest after the diagnosis, irrespective of your child’s age or weight. Untreated hernias are known to have complications in the form of obstruction where the intestine gets stuck and fails to go back in the abdomen. This will then require emergency treatment.
Remember: “SMALLER THE CHILD AND SMALLER THE HERNIA, GREATER THE RISK OF OBSTRUCTION.”


Children with obstructed hernias
What does the operation involve?
The operation is carried out under general anaesthetic and lasts for about 30 – 45 minutes. Once your child is asleep, the surgeon will make a small incision (cut) on the lower abdomen, The abdominal lining and piece of bowel will be pushed back into place. The open passage will be repaired and closed with stitches. These stitches will dissolve and will not have to be removed.
Can this operation done by laparoscopy?
Operation in hernia involves closing of the open passage through which the testis has come down. This can be done from outside as in open surgery or from inside by laparoscopy. If your child has got a hernia on one side, there is a 15 – 25 % chance that he / she may develop a hernia on the opposite side at a later date. With the help of laparoscopy we are able to look at the opposite side to see if the passage is open on that side as well. This can be closed at the same sitting if you wish to. Recovery from surgery, timing of surgery and discharge from hospital are the similar for open surgery and laparoscopic surgery.
However, it is important to note that an open passage does not always mean that your child will get a hernia. There is no harm in opting for a second surgery later if your child at all develops a hernia on the opposite side.
Laparoscopic repairs have a slightly higher chance of recurrence (i.e. the hernia coming back again) as compared to open hernias. You can discuss the pros and cons in details with your doctor when you come for consultation.
Internal Ring in a Boy – Laparoscopic View

Internal ring in a Girl – Laparoscopic View

Open Internal Ring

Closed ring after surgery


Closed Internal Ring

Scars after surgery
What are the risks of surgery?
After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe. Some children develop swelling over the scrotum 24 hours after surgery. This gradually resolves on its own over the course of the next week.
What happens after the operation?
Your child will recover from the anaesthetic on the ward. Once he feels comfortable and has something to drink and eat, you will be able to take your child home. We recommend that you bring in some loose clothing for your child to wear home and for the next few days, as this will be a lot more comfortable.
What happens after you go home?
Your child should not have a bath or shower for three to five days after the operation. After this, it is fine for your child to have a shower, but try to avoid long baths as this may cause the scab to soften and fall off too early.
Your child should be ready to go back to school or nursery about a week after the operation.
The stitches will dissolve on their own within two weeks or so. You will need to visit hospital for a follow up check 7 – 10 days after surgery.
Are there any long term effects of hernia repair?
Most hernia repair operations are successful. You should see an immediate reduction or the complete disappearance of the hernia.
One out of ten children develops a hernia on the opposite side of the body. This risk is doubled if your child has been born prematurely.
GUJARATI
સારણગાંઠ અને વધરાવળ
સારણગાંઠ ૨% બાળકોમાં જાવા મળે છે. બાળક માઁના ગર્ભમાં હોય ત્યારે બાળકના પેટમાં વૃષણની ગોળી બને છે, અને આ ગોળી પેટની બહાર નીકળી અને વૃષણ કોથળીમાં આવે છે. બાળકના જન્મ દરમિયાન આ રસ્તો સામાન્ય રીતે બંધ થઈ જાય છે, પરંતુ જ્યારે આ રસ્તો બંધ નથી થતો ત્યારે આંતરડા બહાર આવે છે અને સારણગાંઠ થાય છે. જા રસ્તો નાનો હોય અને ફક્ત પેટનું પાણી જ બહાર આવે, તો તેને વધરાવળ કહેવાય છે.
સારણગાંઠનું આૅપરેશન નિદાન થયા પછી તુરંતજ, બની શકે તેટલું વહેલું કરી દેવું જાઈએ. સારણગાંઠના આૅપરેશન માટે બાળકની ઉંમર કે બાળકના વજન જેવા કોઈ પરિબળ હોતા નથી. સારણગાંઠનો આૅપરેશન સિવાય બીજા કોઈ ઇલાજ નથી.
સામાન્ય રીતે બાળકને તપાસતાજ સારણગાંઠ અને વધરાવળની ખબર પડી જાય છે, તેના માટે કોઈ વિશેષ તપાસની જરૂર હોતી નથી. સોનોગ્રાફી કરાવવાનો ફાયદો એટલોજ છે કે એક બાજુ સારણગાંઠ હોય તેવા બાળકને સામેની બાજુએ રસ્તો ખુલ્લો છે કે નહીં તે ખબર પડે.
બાળકોને સારણગાંઠના આૅપરેશનમાં ફક્ત આ ખુલ્લો રહી ગયેલો રસ્તો જ બંધ કરવાનો હોય છે. તેમાં મોટા માણસોની જેમ જાળી મૂકવાની જરૂર હોતી નથી. સારણગાંઠનું આૅપરેશન જા ન કરવામાં આવે તો ૧૦% થી ૧૫% બાળકોમાં આંતરડું ફસાવાની શક્યતા રહેલી છે જે એક સીરિયસ પ્રોબ્લેમ છે. સારણગાંઠનું આૅપરેશન નિદાન બાદ બને તેટલું વહેલું કરાવવું જાઈએ. આથી વિપરીત બાળક ૧ વર્ષનું થાય ત્યાં સુધી વધરાવળ આપમેળે મટવાની શક્યતા રહેલી છે. •
HINDI
हर्निया और हाइड्रोसील
हर्निया और हाइड्रोसील एक आम्ा बि्ाम्ारी है जो २% ब्ाच्चों म्ों देखी जाती है। बच्चों में हर्निया और हाइड्रोसील का कारण मार्ग की आशंका है जिसके साथ वृषण पेट से निकल कर अंडकोश में आते हैं। ग्ाभ्ार् म्ों ब्ाच्चे के विकास के दौरान पेट के संकुचित म्ाग्ार् से आँत और पानी अंडकोष की थैली म्ों उतरता है, जिससे हर्निया और अंडकोष वृद्धि (हाइड्रोसील) की सम्ास्या होती है।
हर्निया और हाइड्रोसील की पहचान केवल चिकित्सीय परीक्षण द्वारा की जा सकती है। इसके लिए कोई विशेष जांच की आवश्यकता नहीं है। हालांकि, विपरीत दिशा में ट्रैक्ट की पेटेंसी को देखने के लिए अल्ट्रासाउंड स्कैन किया जा सकता है। इनगुनल हर्निया की पहचान होते ही बच्चे की आयु या उसके वजन की परवाह किये बिना जल्द से जल्द इसकी सर्जरी की जानी चाहिए। यदि हर्निया का इलाज समय पर न किया जाए तो आँतों में रूकावट या ऐंठन जैसी जटिलताएँ हो सकती है। साम्ान्यतः हर्निया से विपरीत, हाइड्रोसील १ वर्ष की उम्ा्र तक अपने आप ठीक हो जाता है, लेकिन १ वर्ष की उम्ा्र के ब्ाद ब्ाच्चे म्ों हाइड्रोसील की सम्ास्या रहने पर सर्जरी कराना आवश्यक है। सर्जरी (हर्नियोटॉमी) द्वारा पेटेंट स्थान को बंद कर दिया जाता है। वयस्कों की भांति बच्चों में जाली लगाने की आवश्यकता नहीं होती है। यह प्रक्रिया आमतौर पर एक दिन की देखभाल में की जाती है, जहाँ बच्चे को सुबह अस्पताल में भर्ती किया जाता है और शाम को घर भेज दिया जाता है। •
Imperforate Anus / Anorectal Malformation
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is an Imperforated anus / Anorectal anomaly?
This is a disorder affecting the anus and the rectum, the last part of the digestive system. After food has been digested it passes through the small bowel into the large bowel. The faeces (stools) are stored in the rectum until the muscles receive a message from the brain to empty the bowel. The faeces then pass out through the anus.
There are two types of anorectal anomaly – low anorectal anomaly and high anorectal anomaly. A low anorectal anomaly is where the anus is closed over, in a slightly different position or narrower than usual. A high anorectal anomaly is where the bowel has a closed end and does not connect with the anus or it connects with another part of the body through a passage called a fistula.
An anorectal anomaly can be associated with other problems, but the doctor will examine your child closely to check if this is the case.
What are the symptoms of an anorectal anomaly?
Symptoms vary according to the type of anorectal anomaly. They are classified into two types (high and low) depending on where the bowel ends.
If your child has a low anorectal anomaly, faeces cannot be removed from the body as usual, and so builds up in the bowel. Your child will not be able to pass meconium – the dark faeces passed in the first few days of life. The build up of faeces in the bowel can cause a swollen abdomen and vomiting.
Low Anorectal Malformations
If your child has a high anorectal anomaly without a fistula, he or she will not be able to pass meconium and will develop similar symptoms.
Anorectal Malformation without fistula
If your child has a high anorectal anomaly with a fistula, the faeces will be able to pass out of the body, usually through the vagina in girls or through the urethra in boys.


Anorectal Malformation without fistula
How is an anorectal anomaly diagnosed?
An anorectal anomaly is usually diagnosed soon after birth, on examination, or when the baby fails to pass meconium. The doctor may suggest scans to give a clearer picture of the type of anorectal anomaly and whether there is a fistula.
What causes an anorectal anomaly and how common is it?
An anorectal anomaly happens when the bowel does not form properly while the baby is developing in the womb. We do not know exactly what caused this, but it was not due to anything that happened during pregnancy.
About one in 3,000 babies are born with an anorectal anomaly, with more boys than girls affected.
What treatments are available and are there any alternatives?
The treatment depends on the type of anorectal anomaly. All types of anorectal anomaly will need an operation under general anaesthetic – usually an ‘anoplasty’ if your child has a low anorectal anomaly or a series of operations if your child has a high anorectal anomaly.
The first operation is to create a loop stoma (an artificial way of disposing of waste matter) usually in the days after birth.
The second is a ‘pull-through’ operation to join the bowel to a newly created anus. This usually happens when your child is a few months old and has gained weight.
The final stage is to close up the stoma. This happens when your child’s bowel and anus is working well a few weeks after the second operation. The three operations are usually completed by the time your child is six months old. There are no alternatives to these operations, as your child needs to be able to pass faeces to prevent it building up in the bowel, which could lead to discomfort and infection.
What does the operation involve?
Anoplasty – the surgeon will open up the anus (if it was closed over), move the anus (if it was in a slightly different place to usual) or widen the anus (if it was narrower than usual).
Creation of loop stoma – the surgeon will bring the bowel to an artificial opening in your child’s abdomen (stoma).
‘Pull-through’ operation – the surgeon will create a new anus and then separate the bowel from the fistula (if there is one) and bring it down to join the newly created anus. He or she will then close up the fistula. Your child will continue to use the stoma so that the bowel and anus can rest and heal.
Closure of loop stoma – the surgeon will disconnect the the bowel from the stoma and close it to form a fully working bowel.
What happens afterwards?
Your child will come back to the ward to recover. We will keep your child as comfortable as possible, by giving regular pain relieving medications. For the first few days, the pain relief will usually be given through a ‘drip’ and then, when your child is more comfortable, in the form of medicines to be swallowed.
For the first few days, your child will need a ‘drip’ of fluids until he or she feels like eating and drinking again. This will also allow the bowel to rest and start to heal. After a while, you can start to feed your child again, starting with small amounts, and increasing the amount as he or she tolerates it.
If your child has had a new anus created, you may be asked to stretch (dilate) it using a probe called a dilator. The doctor will show you how to do this before you go home. You will need to start with a small size dilator and gradually increase the size until the anus is the right size
If your child has had the stoma and mucous fistula created, the nurses will teach you how to look after them both. We will make sure you feel confident before you go home.
What is the outlook for children with anorectal anomaly?
The outlook for children with anorectal anomaly depends on the type of abnormality. Your child may need extra bowel training at a later stage to learn when and how to empty his or her bowels. He or she may also need some extra help in the form of enemas or washouts, but these will be explained to you if they are needed. However, some children continue to have bowel problems for many years after the operations, but this depends on the original severity of the anorectal anomaly.
Your child will need regular check ups with your doctor at the hospital. These happen regularly until your child is a teenager.
Some girls who have had an anorectal anomaly may be better having a caesarean section rather than normal childbirth. This will put less strain on the operation site and is less likely to cause problems in the future.
Publications on the subject : M.R.I. in A.R.M.
GUJARATI
સંડાસની જગ્યા ન હોવી – મળમાર્ગ ન હોવો
દર ૩૦૦૦ એ એક બાળક આ ખોડ સાથે જન્મ લેતું હોય છે. છોકરાંઓમાં આ ખોડ વધુ જાવામાં આવતી હોય છે. આ ખોડ થવાનું કોઈ ચોક્કસ કારણ જાણી શકાયું નથી અને તે ડિલિવરી પહેલાં માતાની સોનોગ્રાફી દ્વારા જાણી શકાતી નથી. આ ખોડ બે પ્રકારની હોય છે. ૧. હાઈ ૨. લો.
૧) ‘હાઈ’ વેરાઈટી : આ ખોડમાં બાળકનાં મળમાર્ગનું આંતરડું પેશાબના રસ્તા સાથે અને બેબીમાં યોનિમાર્ગ સાથે જાડાયેલું હોય છે. આ કેસમાં બાળકને જન્મ પછી તરત આૅપરેશન કરી પેટ પર મળ માટે ટેમ્પરરી રસ્તો કરવો પડે છે. આને કોલોસ્ટોમી કહેવાય છે. બાળક ૩-૫ માસનું થાય ત્યારે પેશાબ સાથેનું કનેક્શન દૂર કરી મળમાર્ગ યોગ્ય જગ્યાએ બનાવવાનું ઓપરેશન કરવામાં આવે છે. ત્યાર બાદ કોલોસ્ટોમીને બંધ કરી દેવામાં આવે છે. સીલેક્ટેડ કેસમાં આ ત્રણેય આૅપરેશન એક જ સ્ટેજમાં કરી શકાય છે.
૨) ‘લો’ વેરાઈટી : આ કેસમાં આંતરડાને પેશાબનાં રસ્તા સાથે કોઈ જાડાણ હોતું નથી. આ કેસમાં પેટે કોલોસ્ટોમી કરવાની જરૂર પડતી નથી અને એક જ આૅપરેશન દ્વારા બાળક સાજું થઈ જતું હોય છે. આ ખોડ સાથે બીજી ખોડ-ખાપણ નથી તે જાણવા માટે એક્ષરે, સોનોગ્રાફી અને ઈકોકાર્ડીયોગ્રાફીની તપાસ થાય છે.
સચોટ આૅપરેશન અને યોગ્ય કાળજી મળે તો આ બાળકો બીજા બાળકોની જેમ નોર્મલ જીવન જીવી શકે છે. •
HINDI
मल मार्ग का न होना
हर ३००० बच्चों में एक बच्चा इस विसंगति के साथ जन्म लेता है। प्रसूति से पूर्व सोनोग्ा्राफी के द्वारा भी इसका पता लगाना कठीन होता है। यह विसंगति दो प्रकार की होती है। (१) ‘लो’ (कम) विसंगति, (२) ‘हाई’ (उच्च) विसंगति।
‘लो’ (कम) प्रकार ः गुदा मार्ग अपने निर्धारित आकार या उचित स्थान पर स्थित नहीं होता है अथवा गुदा मार्ग पूर्णरूप से बंद होता है।
‘हाई’ (उच्च) प्रकार ः गुदा मार्ग पूर्णरूप से बंद होता है और वह शरीर के अन्य अंग के साथ एक मार्ग के द्वारा जुड़ा होता है जिसे फिस्च्युला कहा जाता है।
इसका पता जन्म के तुरंत बाद जांच के उपरांत अथवा जब बच्चा अपना प्रथम मलत्याग नहीं कर पाता तब चलता है। बच्चे में इस प्रकार की विसंगति के साथ किसी अन्य प्रकार की विसंगति तो नहीं है इसकी पुष्टि करने के लिए एक्स-रे, सोनोग्ा्राफी और इकोकार्डियोग्ा्राफी द्वारा जांच की आवश्यकता होती है।
‘लो’ विसंगतिः ऐसे में गुदासंधान (एनोप्लास्टी) की आवश्यकता होती है।
‘हाई’ विसंगतिः इसमें बच्चे पर त्रि-स्तरीय सर्जरी की आवश्यकता होती है। कुछ चुनिंदा मामलों में केवल एक-स्तरीय ऑपरेशन भी किया जा सकता है।
गुदा एवं मलाशय संबंधी विसंगति के संबंध में बच्चे का दृष्टिकोण विसंगति के प्रकार और उसकी तीव्रता पर निर्भर करता है। बाद में, बच्चे को अपने पेट को कब और कैसे साफ करना चाहिए इस बात के प्रशिक्षण की आवश्यकता हो सकती है। उसे अपने पेट को साफ करने के लिए जुलाब दिए जाने की आवश्यकता भी हो सकती है। यह विसंगति वाली लड़कियों में सामान्य प्रसूति के बजाय सीजेरियन सेक्शन अधिक उपयुक्त होता है। इससे उनके ऑपरेशन के स्थान पर कम तनाव पड़ेगा और भविष्य में किसी प्रकार की समस्या होने की संभावना कम होती है।•
Intersex / Disorders of Sexual Differentiation / Ambiguous Genitalia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
INTERSEX / DISORDERS OF SEXUAL DIFFERENTIATION / AMBIGUOUS GENITALIA
At conception, a fetus’s gender is already determined based on the 23rd pair of chromosomes it inherits from the parents. Females have two X chromosomes and males have an X and a Y chromosome. The sexual organs of males and females develop from the same fetal tissue. The main factor controlling the next step is male hormones. The presence of male sex hormones causes male organs to develop and the absence of male hormones causes female organs to develop. Without enough male hormones, a genetic male will develop ambiguous genitalia. Likewise, a genetic female will develop ambiguous genitalia if male hormones are present.
Characteristics of ambiguous genitalia in genetic females:
- An enlarged clitoris which appears to be a small penis
- A concealed vagina
Characteristics of ambiguous genitalia in genetic males:
- Microphallus
- Severe degree of hypospadias
- Bilateral undescended testes
What is the long-term outlook for a child with ambiguous genitalia?
Intersex is a major social challenge also. A complete and thorough investigation with in-depth counselling of the family is mandatory to manage these children. ●
GUJARATI
ઇન્ટરસેક્સ
બાળકનું લીંગ માતા-પિતામાંથી મળેલ સેક્સ ક્રોમોઝોમ્સ પર નિર્ભર છે. સ્ત્રીઓ માં XX ક્રોમોઝોમ્સ અને પુરૂષોમાં XY ક્રોમોઝોમ્સ હોય છે. બાળકની જનેન્દ્રિયો નો વિકાસ ગર્ભ દરમ્યાન થયેલ હોરમોન્સની અસરથી જ થાય છે. હોરમોન્સની થોડી પણ ચૂક/ વધુ અસર/ઓછી અસરના કારણે ઇન્ટરસેક્સના પ્રોબ્લેમ ઉભા થાય છે.
ઇન્ટરસેક્સ એક મોટી મેડીકલ અને સોશીયલ ચેલેન્જ છે. બાળકના જન્મ સમયે જા નીચે જણાવેલ ચિન્હો દેખાય તો ડાક્ટરે તેને બાબો/બેબી જાહેર કરવાની ઉતાવળ કરવી ના જાઈએ. આવા બાળકોને બાળકોના સર્જન દ્વારા તપાસ અને રીપોર્ટ કરાવવા જરૂરી હોય છે. આજના જમાનામાં એન્ડોસ્કોપી અને લેપ્રોસ્કોપી આ બાળકોના લિંગના સચોટ નિદાન અને તેની યોગ્ય સારવાર માટે ખૂબ જ મદદરૂપ થાય છે.
ઇન્ટરસેક્સના ચિન્હો :
(૧) બાળકીઓ (XX) માં ઇન્ટરસેક્સના ચિન્હો :
– યોનિમાર્ગની ઉપર ભગ્નનો આકાર લિંગ જેવો હોવો
– યોનિમાર્ગ બંદ હોવો/ન હોવો
(૨) બાબાઓ (XY) માં ઇન્ટરસ્ક્સના ચિન્હો :
– બાળકી જેવી જનેન્દ્રિયો હોવી.
– પેશાબનો માર્ગ લિંગની નીચે/પાછળ હોવો.
– લિંગ નો ભાગ ખૂબ જ નાનો હોવો અને પેશાબનો રસ્તો ખોટી જગ્યાએ હોવો.
– વૃષણની બંન્ને ગોળી વૃષણ કોથળીમાં ન હોવી. •
HINDI
इंटरसैक्स/यौन भेदभाव का विकार/अस्पष्ट जननांगता
गर्भधारण के समय से ही, अपने माता-पिता से विरासत में प्राप्त २३वें गुणसूत्र के आधार पर भ्ा्रूण का लिंग निश्चित हो जाता है। कन्या में दो ङ्ग गुणसूत्र होते हैं और पुरूष बालक में एक ङ्ग और एक Y गुणसूत्र होता है। पुरूषों और महिलाओं के जनन अंगों का विकास एक ही भ्ा्रूण मांस-तंतु से होता है। अगले चरण को नियंत्रित करनेवाले मुख्य कारक पुरूष हार्मोन है। पुरूष अंगों के विकास का कारण पुरूष जनन हार्मोन की उपस्थिति है और इनकी अनुपस्थिति महिला जनन अंग विकसित करता है। अपर्याप्त पुरूष हार्मोन के कारण आनुवांशिक पुरूष में अस्पष्ट जननांगता का विकास होता है। इसी प्रकार, पुरूष हार्मोन की उपस्थिति के कारण आनुवांशिक महिला में अस्पष्ट जननांगता का विकास होता है।
आनुवांशिक महिलाओं में अस्पष्ट जननांगता के लक्षणः
१. बढ़ा हुआ भगशेफ (Clitoris), जो लघु शिश्न (Penis) सा प्रतीत होता है।
२. छुपा योनि।
आनुवांशिक पुरूषों में अस्पष्ट जननांगता के लक्षणः
१. गैर पहचान योग्य (अथवा अस्पष्ट) पुरूष गुप्तांग।
२. अनुपस्थित जननपिंड के साथ गंभीर अधोमूत्रमार्गता।
३. एक बहुत ही छोटा शिश्न जिसका मूत्रमार्ग अंडकोश की थैली के पास खुला हो।
४. दोनों ही अंडकोशों का अनुपस्थित होना और अंडकोश की थैली का अविकसित होना।
इंटरसैक्स एक प्रमुख सामाजिक चुनौती भी है। ऐसे बच्चों के उपचार के लिए परिवारवाले से बारीकी से परामर्श करने के साथ गहन जांच अनिवार्य है। कई बार, एक निश्चित निदान पर पहुंचने के लिए बहुविशिष्ट दृष्टिकोण आवश्यक होता है। अस्पष्ट जननांगता के साथ जन्मे कुछ बच्चों के जनन अंग सामान्य होते हैं जो उन्हें प्रजननक्षम जीवन व्यापन करने की अनुमति प्रदान करते हैं। अन्य कुछ प्रजननक्षम नहीं होते हैं अथवा वे गर्भधारण करने में कठिनाई का अनुभव करते हैं। कभी-कभार बाद के जीवनकाल में उनके जननअंग में गांठ हो जाने का खतरा होता है।•
Jejunal Atresia
The intestines form early in pregnancy as a long straight tube. Before the tenth week of pregnancy, they develop into the separate organs making up the digestive system. Occasionally, the intestines are not completely connected or blocked (atresia). Sometimes there is a partial blockage (web) inside the intestine.
Any part of the intestines can be affected by atresia or stenosis. Duodenal Atresia is one type. This occurs in around one in 6,000 births where the duodenum is closed off rather than being a tube. If the jejunum or ileum are affected, this is called ‘small bowel atresia’.
Small bowel atresia is more common than duodenal atresia. We do not know how exactly how many babies are born with small bowel atresia each year but we do know that it affects boys and girls equally. It is more common in twins or multiple births and babies born prematurely or with low birthweight.
Colonic atresia, affecting the large bowel, is very rare.
Small bowel atresia affects two areas of the small bowel – the jejunum and the ileum. The jejunum is the section of small bowel after the duodenum and is where the majority of nutrients are absorbed. The ileum is the main part of the small bowel, making up over half of its entire length, and connects to the large bowel. The blockage can affect any part of the ileum or jejunum.
What causes small bowel atresia?
More research is needed into the causes of small bowel atresia but currently doctors think that it is caused by reduced blood supply to sections of the bowel as the baby is developing in the womb. It is unlikely that it is caused by anything you did or did not do during pregnancy.
What are the signs and symptoms of small bowel atresia?
Many babies born with small bowel atresia appear well at birth but when they start to feed, they start to have nausea and vomiting and their vomit may be green. Their abdomen may appear swollen but soft and their skin may develop a yellow tinge (jaundice).
All newborn babies have meconium in their bowel. This is the dark green stool passed in the first day of life. Babies born with small bowel atresia may not pass any meconium at all or only a small amount. Not passing meconium does not prove that a baby has small bowel atresia but it may suggest it. Some babies with small bowel atresia pass meconium as expected.
How is small bowel atresia diagnosed?
When a baby with small bowel atresia is developing in the womb, they are may be surrounded by much more amniotic fluid than usual (polyhydramnios). Small bowel atresia can sometimes be suggested during pregnancy using an ultrasound scan.
After the baby is born, small bowel atresia is usually diagnosed when there are signs of an obstruction, such as vomiting, green bile and a swollen abdomen. An x-ray scan may show a blockage. Occasionally, doctors may suggest using a contrast scan and/or enema instead or as well as an x-ray.
Contrast scans and enemas use a thick, white liquid called barium or a clear liquid (contrast), both of which show up well on x-rays. The contrast cannot pass through the atresia suggests that atresia can be a cause.
How can small bowel atresia be treated?
Small bowel atresia is repaired in an operation under general anaesthetic. The operation to repair the atresia can is usually carried out using open surgery. Sometimes a laparoscopic surgery (key hole procedure) may help diagnose the problem so that it can be repaired using open surgery.
Are there any alternatives?
No. Small bowel atresia always requires surgical treatment to allow your baby to feed.
What happens before the operation?
Your baby will be transferred to the hospital soon after birth.
If your child is dehydrated, they will need a ‘drip’ of fluids for a while before the operation. Your child will also need a nasogastric tube, which is passed up the nose, down the foodpipe and into the stomach. This will drain off the stomach and bowel contents and ‘vent’ any air that has built up, which will make your child more comfortable.
When your child is stable, the surgeon will explain about the operation in more detail. Sometimes the atresia is suspected but may not be the only possible cause of the blockage. The surgeon will explain this to you.
What does the operation involve?
The surgeon will look at the bowel to determine the level of the blockage. If it is an atresia, this section is removed and the cut ends are joined together (anastomosis). This provides a clear passage for food and fluid to travel through your child’s intestine. The remainder of the small intestine will be checked for further atresias and treated if identified.
If it is not possible or safe to join the two ends together during the same procedure, the surgeon may bring the end of the intestine to an artificial opening (stoma) in the abdomen to form an ileostomy.
Are there any risks?
All surgery carries a small risk of bleeding during or after the operation. There is a chance that the area where the two ends of bowel were joined could start to leak, allowing bowel contents to escape into the abdomen. This is usually treated with antibiotics, but a second operation may be needed to check the leaking portion.
All abdominal surgery carries the risk of strictures forming. These are areas of scar tissue that can narrow the intestines, leading to obstruction. If your child vomits green bile and has a swollen abdomen, they should be reviewed urgently by a doctor.
It can take a while after the operation for the bowel to start working properly so your child may need to be fed intravenously using total parenteral nutrition (TPN) for a while. This affects many children.
What happens after the operation?
While your child’s intestines recover and start to work, they may be fed through a tube into their veins (total parenteral nutrition or TPN). This will gradually be replaced by breast or bottled milk, given through the naso-gastric tube when your child is able to tolerate this. As your baby recovers, you will be able to feed them from the breast or bottle. Over time, the drips and monitors will be removed one by one.Most children stay in hospital for one to two weeks, but occasionally a longer stay is needed.
What happens next?
The outlook depends on the amount of damage to the bowel. Adhesions can form after any abdominal surgery and can cause further problems such as blockage or pain. This however is quite rare and may sometimes require another operation to separate the adhesions.
Jaundice (Surgical Jaundice)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
JAUNDICE AND THE SURGEON
Jaundice in the neonatal age is a common physiological phenomenon. It increases on the 3rd or 4th day of life and gradually regresses. The child becomes normal by the 3rd week of life. This is common in premature children, children with sepsis or blood group incompatibility. This is diagnosed with blood tests and if necessary, the child is treated with phototherapy.
However, if the jaundice continues beyond the 1st month of life and the child has dark yellow urine and white or chalky stools, it should raise a red flag. The child’s bilirubin level needs to be checked and further work up is necessary.
Cells within the liver produce liquid called bile which helps in digestion. The network of channels which help carry bile from the liver to the intestines is called the biliary system.
Sometimes children may have a cyst / cysts in the biliary system. This is called choledochal cyst. It may cause symptoms like pain, jaundice or may be picked up incidentally on an ultrasound scan. The treatment of this cyst is surgical excision followed by reconstruction of the biliary tree.
Biliary atresia is a rare disease of the liver and bile ducts that occurs in infants. When a baby has biliary atresia, bile flow from the liver to the gallbladder is blocked. This causes the bile to be trapped inside the liver causing damage and scarring of the liver cells (cirrhosis) and eventually liver failure. There are many investgiations that can be done to diagnose biliary atresia. However, only laparoscopic cholangiography can help diagnose biliary atresia with certainty . Liver biopsy can also be done laparoscopically which can help identify the degree of damage to the liver. Surgical reconstruction of the biliary tree is done for biliary atresia. Best results are expected when surgery is done before 3 months age. •
GUJARATI
બાળકમાં કમળો અને સર્જન
નવજાત શીશુમાં કમળો થવો એ ખૂબ જ સામાન્ય બાબત છે. આ જન્મ નાં ૩-૪ દિવસે થાય છે અને પછી ધીમે ધીમે ઘટવા માંડી ૨૦ દિવસ સુધીમાં બાળક નોર્મલ થઈ જાય છે. અધૂરા માસે જન્મેલા બાળકોમાં, ઇન્ફેક્શન વાળા બાળકોમાં, માતા સાથે બ્લડ ગ્રુપની અસમાનતા વાળા બાળકોમાં આ વધુ જાવામાં આવે છે. આ કમળાને ફિઝ્યોલોજિકલ કમળો કહેવામાં આવે છે. નવજાત બાળકમાં કમળો એક મહિનાથી વધુ ચાલે, સંડાસ સફેદ અથવા આછું પીળું થાય અને પેશાબ વધુ પડતો પીળો હોય તો લોહી ચેક કરાવી કમળાનું પ્રમાણ જાણવું જાઈએ.
લીવરના કોષમાંથી પીત્ત નામનું પ્રવાહી બને છે જે પાચનક્રિયામાં મદદરૂપ થાય છે. લીવરમાંથી પીત્તને આંતરડામાં પહોંચાડતી નળીઓ ને “બિલિયરી સીસ્ટમ” કહે છે.
બાળકમાં આ પીત્તની નળીઓની જન્મજાત ગાંઠને “કોલીડોકલ સીસ્ટ” કહે છે. આ ગાંઠના કારણે બાળકને દુઃખાવો અને કમળો થઈ શકે છે. યોગ્ય સમયે આૅપરેશન આ બીમારીનો ઇલાજ છે.
ઘણાં બાળકોમાં જન્મજાત પિત્તની નળીઓ (બિલીયરી સીસ્ટમ) બની હોતી નથી. આ બિમારી બિલિયરી એટ્રેઝિયા કહેવાય છે.
આ બીમારીના કારણે પિત્તનો લીવરમાં ભરાવો થવાથી લીવરને નુકશાન થાય છે. આ બીમારી માટે બાળક ૩ મહિનાની ઉંમરનું થાય તે પહેલા આૅપરેશન કરી આંતરડામાંથી પિત્તનો રસ્તો બનાવવો પડે છે. બિલિયરી એટ્રેઝિયાના નિદાન માટે ઘણા ટેસ્ટ કરી શકાય છે, પરંતુ “લેપ્રોસ્કોપીક કોલેંજયોગ્રાફી” એક જ એવી તપાસ છે જે ૧૦૦% ખાત્રીથી જણાવી શકે કે બાળકને બિલિયરી એટ્રેઝિયા છે કે નહી. ●
HINDI
बच्चों में पीलीया और सर्जन
बच्चों में पीलीया की बीमारी को दो भागों में विभाजित किया गया है।
१) नवजात शिशु से लेकर १ माह की आयु तक
२) १ माह से अधिक की आयु वाला बच्चा
नवजात शिशु को पीलीया होना एक आम बात है। यह बीमारी बच्चे के जन्म के ३-४ दिनों में होती है और बाद में धीरे-धीरे कम होने लगती है। २० दिन में बच्चा सामान्य हो जाता है। इसे फिजीयोलोजिकल पीलीया कहते हैं। यह पीलीया समय से पहले जन्मे बच्चे, असमान ब्लड ग्ा्रूप और संक्रमण वाले बच्चे को होता है। पीलीया का स्तर यदि बढ़ जाए तो बच्चे को अस्पताल में भर्ती कर फोटोथेरापी और खून में पीलीया के स्तर की जाँच कराना आवश्यक होता है।
बच्चों में पीलीया और सर्जन
१) नवजात बच्चे में यदि पीलीया एक महीने से अधिक रहता है और मल सफेद या हल्के पीले रंग का हो और पेशाब का रंग अत्यधिक पीले रंग का हो तो खून की जाँच कर पीलीया के स्तर के बारे में पता लगा लेना चाहिए।
२) बीलीयरी एट्रेझीया नामक रोग के कारण पित्त की नलियाँ न बनने की वजह से पीलीया बढ़ता जाता है। मल सफेद रंग का होता है और बच्चे का जीगर बड़ा होने लगता है। यह एक गंभीर बीमारी है और बच्चे की आयु २ माह की होने तक इसका ऑपरेशन करा लेना आवश्यक है।
जन्म से पहले या जन्म के बाद बच्चे के जीगर (लीवर) के नीचे यदि कोई गांठ हो (कोलेडोकल सीस्ट) तो जाँच करा कर उचित समय पर ऑपरेशन करने की आवश्यकता होती है। •
Kidney Stones
Kidney (or renal) stones are clusters of tiny crystals that can form in the kidneys. Most clusters are too small to cause any problems and pass out of the body in the urine.
Sometimes, the clusters can clump together to form bigger clusters, which may eventually become big enough to block the filtering units in the kidney. Sometimes, they pass out of the kidney down the ureter and out in the urine without causing any problems, but if they are big they may block the ureter or lodge in the bladder.
Kidney stones are much more common in adults than in children. Children who have kidney stones will be checked thoroughly to rule out or confirm an underlying condition causing the problem. This could include a structural abnormality with the urinary system or a problem with the metabolism.
What causes kidney stones?
The urinary system consists of the kidneys, ureters, the bladder and urethra. The kidneys filter the blood to remove waste products and produce urine. The urine flows from the kidneys down through the ureters to the bladder, where it is stored until we go to the toilet. It passes through another tube called the urethra to the outside when urinating.
The kidneys contain millions of tiny filtering units called glomeruli. As blood passes through the tubes in the glomerulus, waste products pass through the walls of the tubes to form urine. Blood cells and other things such as protein cannot pass through the walls because they are too big.
The urine contains lots of different substances, which do not cause any problems when the urine is weak and the amount of each substance is balanced.
However, when the urine becomes too concentrated, often due to dehydration, the proportion of these substances in the urine increases, which can make crystals form. They can also form if the amount of these substances increases because the body is making more of them than it should or not removing them normally.
In rare situations, kidney stones can develop after urinary infections. Some children are more at risk of kidney stones, for instance, children who were born prematurely or those who have very limited mobility, such as those confined to wheelchair..
What are the signs and symptoms of kidney stones?
Some kidney stones do not cause any symptoms at all, particularly if they are very small and not causing a blockage. However, kidney stones can be painful and cause blood in the urine (haematuria) and generally feelings of being unwell, such as a high temperature and vomiting. If the stone passes out of the kidney into the ureter, it can cause severe pain.
Kidney stones can cause an infection. Signs of an infection include a high temperature, vomiting and/or diarrhoea and urine that is pink or cloudy. Studies have shown that pain is not experienced in approximately half of young children with stones.
How are kidney stones normally diagnosed?
Apart from the history which is derived from asking you questions about the problem, various imaging scans may be needed to confirm the diagnosis, see where the kidney stones are located and their size. Anultrasound scan is usually the first test to help make the diagnosis, although other scans may be needed as well. Urine tests will be needed to show whether there is an infection and to measure the chemicals that cause stones. Blood tests will show how well the kidneys are working.
How are kidney stones normally treated?
This depends on their size and location. Smaller stones can be broken up using sound waves (lithotripsy). Some stones that are stuck in the ureter can be removed using an endoscope, a tube containing a small camera, a light and a laser device to break up the stone. Most other stones are removed using surgery through a small cut. The final decision as to how to remove the stone will vary from child to child and the number and size of stone and whether there are other problems related to the kidney or its drainage system that has caused the stone to form.
Children with lots of stones or stones in both kidneys usually need several procedures to clear the stones. It is important to drink plenty of fluids to stop them forming again. Some children may need to reduce their salt intake and, rarely, other medicines or measures may be necessary.
Key Hole Surgery or Minimally Invasive Surgery
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is keyhole surgery or Minimally Invasive Surgery ?
Keyhole surgery, or laparoscopic surgery as it is also known, is a method of carrying out an operation without having to make a large incision. Many different types of operations can now be carried out using keyhole surgery. This type of surgery reduces the length of time your child needs to stay in hospital and leaves little scarring.
What are the advantages of keyhole surgery?
Children tend to recover more quickly after keyhole surgery and have fewer side effects. There is little scarring after keyhole surgery which becomes more important as your child grows older and becomes more self-conscious. One side effect of ‘open’ surgery – minimised with keyhole surgery – is ‘adhesions’. This is where internal organs stick together and form bands of scar tissue, which can be painful and cause obstruction. Adhesions have been proven to occur less often in adults after keyhole surgery, and the risk of adhesions in children after keyhole surgery is thought to be less as well.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. After an anaesthetic, children sometimes feel sick and vomit, may have a headache, sore throat or feel dizzy. These effects are short-lived. Any surgery carries a small risk of infection or bleeding.
After the operation, some older children may complain of shoulder pain. Your child may also feel some crackling under the skin because the carbon dioxide sometimes escapes into the tissue just under the skin. These side effects are usually short-lived and do not require any specialized care.
There is always a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision instead.
Are there any alternatives to keyhole surgery?
All operations carried out as keyhole surgery can also be carried out using ‘open’ surgery, that is, with a larger incision.
What does the operation involve?
Your child will be given a general anaesthetic and will be asleep during the operation. Once your child is asleep, the surgeon inserts a small tube called a cannula into your child’s tummy button. A telescope, with a miniature video camera mounted on it, is inserted into this tube to project a very high quality video image onto a television screen. The abdomen is then inflated with carbon dioxide to create space in which the surgeon can operate. The operation is performed by inserting specialized instruments which are passed through small hollow tubes which are inserted through separate very small incisions. There may be two or more small incisions required to perform the operation. Once the operation is over, the surgeon will stitch up the inside of the holes and your child will be taken to the recovery room to wake up from the anaesthetic.
What happens after the operation?
After the operation, your child will return to recover.
Your child may also have a naso-gastric tube, which is a tube passed through the nose into the stomach, so that he or she can be given feeds or medicines easily. Your child may also have an intravenous (into a vein) infusion of fluids as he or she may not feel like eating and drinking after the operation.
You may be able to feel a few lumps under the skin by the wound sites, which are stitches inside the body. This is nothing to worry about and the stitches will dissolve on their own in about three months.
GUJARATI
દૂરબીન વડે પેટનાં ઓપરેશન (લેપ્રોસ્કોપી અને થોરેકોસ્કોપી)
લેપ્રોસ્કોપી:
“લેપ્રોસ્કોપી” એટલે પેટ પર નાના છિદ્રો દ્વારા દૂરબીન અને સાધનો મુકી પેટનાં વિવિધ આૅપરેશન કરવા. બાળકોમાં અને નવજાત શિશુઓમાં આ ટેકનિકથી ફ્ક્ત ૩ મીમી અથવા ૫ મી.મી.નાં નાના કાણાથી આૅપરેશન કરવામાં આવે છે. આધુનિક કેમેરા અને લાઈટની મદદથી ટી.વીમાં મોટી ઈમેજ જાઇ આવા આૅપરેશન ખૂબ જ સારી અને ચોક્કસાઇ પૂર્વક થાય છે.
લેપ્રોસ્કોપીની ટેકનિક શીખવા માટે બાળકોનાં સર્જનએ ચોક્કસ પ્રકારની ટ્રેનિંગ લેવી પડે છે અને તેના માટે સ્પેશ્યલ સાધનોની જરૂર પડે છે.
નવજાત બાળકો અને મોટા બાળકોમાં લેપ્રોસ્કોપીના મુખ્ય આૅપરેશન આ પ્રમાણે છેઃ
– એપેન્ડીક્સ
– ઇન્દ્રની ગોળી પેટમાં હોય (અનડીસેન્ડેડ ટેસ્ટીસ)
– પેટમાં ગાંઠ હોવી.
– અંડાશય(ઓવરી)માં ગાંઠ
– લીવરની ગાંઠ
– મેકલ્સ ડાયવરટીક્યુલમ
– કિડની નળીનાં આૅપરેશન
– ઉદરપટલનાં હર્નીયા
– સારણ ગાંઠ
આ સિવાય બીજા અનેક આૅપરેશન લેપ્રોસ્કોપી દ્વારા બાળકોમાં થાય છે. લેપ્રોસ્કોપીના આૅપરેશનથી બાળકને દુઃખાવો ખૂબ જ ઓછો થાય છે. લોહીની જરૂર નથી પડતી અને પેટ પર ગંદા કાપા નથી પડતાં. બાળક નું હાÂસ્પટલમાં થતું રોકાણ પણ ઓછું થઈ જાય છે.
આધુનિક મેડિકલ સાયન્સ અને ટેžનોલોજીની આ એક અદ્ભૂત શોધ છે. •
થોરેકોસ્કોપી:
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો (ડુપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
दूरबीन से पेट की सर्जरी (लेप्रोस्कोपी और थोरेकोस्कोपी )
लेप्रोस्कोपी:
‘लेप्रोस्कोपी’ सर्जरी की एक पद्धति है, जिसमें कोई बड़ा चीरा किये बिना पेट में छोटे छेद करके दूरबीन और अन्य उपकरणों द्वारा पेट के विभिन्न प्रकार के ऑपरेशन किये जाते हैं। इस तकनीक में नवजात शिशु और बड़े बच्चों के ऑपरेशन मात्र ३ और ५ मिलीमीटर के छेद करके किया जाता है।
इस प्रक्रिया में बच्चें को बेहोश करने के बाद बाल सर्जन बच्चे के पेट में छेद करके एक छोटी ट्यूब डालते हैं, जिसपर एक आधुनिक कैमरा और लाइट लगी हुई होती है, जिसकी मदद से टी.वी में बड़ी इमेज दिखाई देती है और बड़ी ही सावधानीपर्वूक ऑपरेशन किया जाता है। इस सर्जरी में दो या अधिक छोटे छेद करके ऑपरेशन किया जाता है। इस तकनीक के लिए बाल सर्जन को विशेष प्रकार की ट्रेनिंग लेनी पड़ती है और इसमें विशेष उपकरणों का इस्तेमाल करने की आवश्यकता है।
नवजात बच्चों और बड़े बच्चों में लेप्रोस्कोपी ऑपरेशन मुख्य रूप से नीचे दिये गये रोगों के लिए किया जाता हैः
१. ऐपेन्डिक्स
२. अनडीसेन्डेड टेस्टीस
३. पेट के अंदर गांठ होने के कारण
४. अंडाशय में गांठ, लीवर में गांठ
५. मेकल्स डायवरटीक्युलम
थोरेकोस्कोपी:
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३ मिलीमीटरऔर ५ मिलीमीटर के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (एंपियेमा)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की श्वसनीजन्य पुटी [Bronchogenic Cyst] और जलस्फोट पुटी [ Hydatid Cyst])
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Key Hole Surgery (Laparoscopy / Minimally Invasive Surgery)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is laparoscopic or keyhole surgery?
Keyhole surgery, or laparoscopic surgery as it is also known, is a method of carrying out an operation without having to make a large incision. Many different types of operations can now be carried out using keyhole surgery. This type of surgery reduces the length of time your child needs to stay in hospital and leaves little scarring.
What are the advantages of keyhole surgery?
Children tend to recover more quickly after keyhole surgery and have fewer side effects. There is little scarring after keyhole surgery which becomes more important as your child grows older and becomes more self-conscious. One side effect of ‘open’ surgery – minimised with keyhole surgery – is ‘adhesions’. This is where internal organs stick together and form bands of scar tissue, which can be painful and cause obstruction. Adhesions have been proven to occur less often in adults after keyhole surgery, and the risk of adhesions in children after keyhole surgery is thought to be less as well.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. After an anaesthetic, children sometimes feel sick and vomit, may have a headache, sore throat or feel dizzy. These effects are short-lived. Any surgery carries a small risk of infection or bleeding.
After the operation, some older children may complain of shoulder pain. Your child may also feel some crackling under the skin because the carbon dioxide sometimes escapes into the tissue just under the skin. These side effects are usually short-lived and do not require any specialized care.
There is always a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision instead.
Are there any alternatives to keyhole surgery?
All operations carried out as keyhole surgery can also be carried out using ‘open’ surgery, that is, with a larger incision.
What does the operation involve?
Your child will be given a general anaesthetic and will be asleep during the operation. Once your child is asleep, the surgeon inserts a small tube called a cannula into your child’s tummy button. A telescope, with a miniature video camera mounted on it, is inserted into this tube to project a very high quality video image onto a television screen. The abdomen is then inflated with carbon dioxide to create space in which the surgeon can operate. The operation is performed by inserting specialized instruments which are passed through small hollow tubes which are inserted through separate very small incisions. There may be two or more small incisions required to perform the operation. Once the operation is over, the surgeon will stitch up the inside of the holes and your child will be taken to the recovery room to wake up from the anaesthetic.
What happens after the operation?
After the operation, your child will return to recover.
Your child may also have a naso-gastric tube, which is a tube passed through the nose into the stomach, so that he or she can be given feeds or medicines easily. Your child may also have an intravenous (into a vein) infusion of fluids as he or she may not feel like eating and drinking after the operation.
You may be able to feel a few lumps under the skin by the wound sites, which are stitches inside the body. This is nothing to worry about and the stitches will dissolve on their own in about three months.
GUJARATI
દૂરબીન વડે પેટનાં ઓપરેશન (લેપ્રોસ્કોપી અને થોરેકોસ્કોપી)
લેપ્રોસ્કોપી:
“લેપ્રોસ્કોપી” એટલે પેટ પર નાના છિદ્રો દ્વારા દૂરબીન અને સાધનો મુકી પેટનાં વિવિધ આૅપરેશન કરવા. બાળકોમાં અને નવજાત શિશુઓમાં આ ટેકનિકથી ફ્ક્ત ૩ મીમી અથવા ૫ મી.મી.નાં નાના કાણાથી આૅપરેશન કરવામાં આવે છે. આધુનિક કેમેરા અને લાઈટની મદદથી ટી.વીમાં મોટી ઈમેજ જાઇ આવા આૅપરેશન ખૂબ જ સારી અને ચોક્કસાઇ પૂર્વક થાય છે.
લેપ્રોસ્કોપીની ટેકનિક શીખવા માટે બાળકોનાં સર્જનએ ચોક્કસ પ્રકારની ટ્રેનિંગ લેવી પડે છે અને તેના માટે સ્પેશ્યલ સાધનોની જરૂર પડે છે.
નવજાત બાળકો અને મોટા બાળકોમાં લેપ્રોસ્કોપીના મુખ્ય આૅપરેશન આ પ્રમાણે છેઃ
– એપેન્ડીક્સ
– ઇન્દ્રની ગોળી પેટમાં હોય (અનડીસેન્ડેડ ટેસ્ટીસ)
– પેટમાં ગાંઠ હોવી.
– અંડાશય(ઓવરી)માં ગાંઠ
– લીવરની ગાંઠ
– મેકલ્સ ડાયવરટીક્યુલમ
– કિડની નળીનાં આૅપરેશન
– ઉદરપટલનાં હર્નીયા
– સારણ ગાંઠ
આ સિવાય બીજા અનેક આૅપરેશન લેપ્રોસ્કોપી દ્વારા બાળકોમાં થાય છે. લેપ્રોસ્કોપીના આૅપરેશનથી બાળકને દુઃખાવો ખૂબ જ ઓછો થાય છે. લોહીની જરૂર નથી પડતી અને પેટ પર ગંદા કાપા નથી પડતાં. બાળક નું હાÂસ્પટલમાં થતું રોકાણ પણ ઓછું થઈ જાય છે.
આધુનિક મેડિકલ સાયન્સ અને ટેžનોલોજીની આ એક અદ્ભૂત શોધ છે. •
થોરેકોસ્કોપી:
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો (ડુપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
दूरबीन से पेट की सर्जरी (लेप्रोस्कोपी और थोरेकोस्कोपी )
लेप्रोस्कोपी:
‘लेप्रोस्कोपी’ सर्जरी की एक पद्धति है, जिसमें कोई बड़ा चीरा किये बिना पेट में छोटे छेद करके दूरबीन और अन्य उपकरणों द्वारा पेट के विभिन्न प्रकार के ऑपरेशन किये जाते हैं। इस तकनीक में नवजात शिशु और बड़े बच्चों के ऑपरेशन मात्र ३ और ५ मिलीमीटर के छेद करके किया जाता है।
इस प्रक्रिया में बच्चें को बेहोश करने के बाद बाल सर्जन बच्चे के पेट में छेद करके एक छोटी ट्यूब डालते हैं, जिसपर एक आधुनिक कैमरा और लाइट लगी हुई होती है, जिसकी मदद से टी.वी में बड़ी इमेज दिखाई देती है और बड़ी ही सावधानीपर्वूक ऑपरेशन किया जाता है। इस सर्जरी में दो या अधिक छोटे छेद करके ऑपरेशन किया जाता है। इस तकनीक के लिए बाल सर्जन को विशेष प्रकार की ट्रेनिंग लेनी पड़ती है और इसमें विशेष उपकरणों का इस्तेमाल करने की आवश्यकता है।
नवजात बच्चों और बड़े बच्चों में लेप्रोस्कोपी ऑपरेशन मुख्य रूप से नीचे दिये गये रोगों के लिए किया जाता हैः
१. ऐपेन्डिक्स
२. अनडीसेन्डेड टेस्टीस
३. पेट के अंदर गांठ होने के कारण
४. अंडाशय में गांठ, लीवर में गांठ
५. मेकल्स डायवरटीक्युलम
थोरेकोस्कोपी:
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३ मिलीमीटरऔर ५ मिलीमीटर के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (एंपियेमा)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की श्वसनीजन्य पुटी [Bronchogenic Cyst] और जलस्फोट पुटी [ Hydatid Cyst])
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Laparoscopy or Key Hole Surgery
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is laparoscopic or keyhole surgery?
Keyhole surgery, or laparoscopic surgery as it is also known, is a method of carrying out an operation without having to make a large incision. Many different types of operations can now be carried out using keyhole surgery. This type of surgery reduces the length of time your child needs to stay in hospital and leaves little scarring.
What are the advantages of keyhole surgery?
Children tend to recover more quickly after keyhole surgery and have fewer side effects. There is little scarring after keyhole surgery which becomes more important as your child grows older and becomes more self-conscious. One side effect of ‘open’ surgery – minimised with keyhole surgery – is ‘adhesions’. This is where internal organs stick together and form bands of scar tissue, which can be painful and cause obstruction. Adhesions have been proven to occur less often in adults after keyhole surgery, and the risk of adhesions in children after keyhole surgery is thought to be less as well.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. After an anaesthetic, children sometimes feel sick and vomit, may have a headache, sore throat or feel dizzy. These effects are short-lived. Any surgery carries a small risk of infection or bleeding.
After the operation, some older children may complain of shoulder pain. Your child may also feel some crackling under the skin because the carbon dioxide sometimes escapes into the tissue just under the skin. These side effects are usually short-lived and do not require any specialized care.
There is always a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision instead.
Are there any alternatives to keyhole surgery?
All operations carried out as keyhole surgery can also be carried out using ‘open’ surgery, that is, with a larger incision.
What does the operation involve?
Your child will be given a general anaesthetic and will be asleep during the operation. Once your child is asleep, the surgeon inserts a small tube called a cannula into your child’s tummy button. A telescope, with a miniature video camera mounted on it, is inserted into this tube to project a very high quality video image onto a television screen. The abdomen is then inflated with carbon dioxide to create space in which the surgeon can operate. The operation is performed by inserting specialized instruments which are passed through small hollow tubes which are inserted through separate very small incisions. There may be two or more small incisions required to perform the operation. Once the operation is over, the surgeon will stitch up the inside of the holes and your child will be taken to the recovery room to wake up from the anaesthetic.
What happens after the operation?
After the operation, your child will return to recover.
Your child may also have a naso-gastric tube, which is a tube passed through the nose into the stomach, so that he or she can be given feeds or medicines easily. Your child may also have an intravenous (into a vein) infusion of fluids as he or she may not feel like eating and drinking after the operation.
You may be able to feel a few lumps under the skin by the wound sites, which are stitches inside the body. This is nothing to worry about and the stitches will dissolve on their own in about three months.
GUJARATI
દૂરબીન વડે પેટનાં ઓપરેશન (લેપ્રોસ્કોપી અને થોરેકોસ્કોપી)
લેપ્રોસ્કોપી:
“લેપ્રોસ્કોપી” એટલે પેટ પર નાના છિદ્રો દ્વારા દૂરબીન અને સાધનો મુકી પેટનાં વિવિધ આૅપરેશન કરવા. બાળકોમાં અને નવજાત શિશુઓમાં આ ટેકનિકથી ફ્ક્ત ૩ મીમી અથવા ૫ મી.મી.નાં નાના કાણાથી આૅપરેશન કરવામાં આવે છે. આધુનિક કેમેરા અને લાઈટની મદદથી ટી.વીમાં મોટી ઈમેજ જાઇ આવા આૅપરેશન ખૂબ જ સારી અને ચોક્કસાઇ પૂર્વક થાય છે.
લેપ્રોસ્કોપીની ટેકનિક શીખવા માટે બાળકોનાં સર્જનએ ચોક્કસ પ્રકારની ટ્રેનિંગ લેવી પડે છે અને તેના માટે સ્પેશ્યલ સાધનોની જરૂર પડે છે.
નવજાત બાળકો અને મોટા બાળકોમાં લેપ્રોસ્કોપીના મુખ્ય આૅપરેશન આ પ્રમાણે છેઃ
– એપેન્ડીક્સ
– ઇન્દ્રની ગોળી પેટમાં હોય (અનડીસેન્ડેડ ટેસ્ટીસ)
– પેટમાં ગાંઠ હોવી.
– અંડાશય(ઓવરી)માં ગાંઠ
– લીવરની ગાંઠ
– મેકલ્સ ડાયવરટીક્યુલમ
– કિડની નળીનાં આૅપરેશન
– ઉદરપટલનાં હર્નીયા
– સારણ ગાંઠ
આ સિવાય બીજા અનેક આૅપરેશન લેપ્રોસ્કોપી દ્વારા બાળકોમાં થાય છે. લેપ્રોસ્કોપીના આૅપરેશનથી બાળકને દુઃખાવો ખૂબ જ ઓછો થાય છે. લોહીની જરૂર નથી પડતી અને પેટ પર ગંદા કાપા નથી પડતાં. બાળક નું હાÂસ્પટલમાં થતું રોકાણ પણ ઓછું થઈ જાય છે.
આધુનિક મેડિકલ સાયન્સ અને ટેžનોલોજીની આ એક અદ્ભૂત શોધ છે. •
થોરેકોસ્કોપી:
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો (ડુપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
दूरबीन से पेट की सर्जरी (लेप्रोस्कोपी और थोरेकोस्कोपी )
लेप्रोस्कोपी:
‘लेप्रोस्कोपी’ सर्जरी की एक पद्धति है, जिसमें कोई बड़ा चीरा किये बिना पेट में छोटे छेद करके दूरबीन और अन्य उपकरणों द्वारा पेट के विभिन्न प्रकार के ऑपरेशन किये जाते हैं। इस तकनीक में नवजात शिशु और बड़े बच्चों के ऑपरेशन मात्र ३ और ५ मिलीमीटर के छेद करके किया जाता है।
इस प्रक्रिया में बच्चें को बेहोश करने के बाद बाल सर्जन बच्चे के पेट में छेद करके एक छोटी ट्यूब डालते हैं, जिसपर एक आधुनिक कैमरा और लाइट लगी हुई होती है, जिसकी मदद से टी.वी में बड़ी इमेज दिखाई देती है और बड़ी ही सावधानीपर्वूक ऑपरेशन किया जाता है। इस सर्जरी में दो या अधिक छोटे छेद करके ऑपरेशन किया जाता है। इस तकनीक के लिए बाल सर्जन को विशेष प्रकार की ट्रेनिंग लेनी पड़ती है और इसमें विशेष उपकरणों का इस्तेमाल करने की आवश्यकता है।
नवजात बच्चों और बड़े बच्चों में लेप्रोस्कोपी ऑपरेशन मुख्य रूप से नीचे दिये गये रोगों के लिए किया जाता हैः
१. ऐपेन्डिक्स
२. अनडीसेन्डेड टेस्टीस
३. पेट के अंदर गांठ होने के कारण
४. अंडाशय में गांठ, लीवर में गांठ
५. मेकल्स डायवरटीक्युलम
थोरेकोस्कोपी:
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३ मिलीमीटरऔर ५ मिलीमीटर के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (एंपियेमा)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की श्वसनीजन्य पुटी [Bronchogenic Cyst] और जलस्फोट पुटी [ Hydatid Cyst])
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Lymphatic Malformation
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Lymphatic malformations: (Also read Cystic Hygroma)
A lymphatic malformation is an area in the body containing clear fluid, called lymph. A lymphatic malformation appears as a lump just under the skin, often in the neck or armpit, although they can develop anywhere in the body.
The lump can enlarge the area of the body, for instance, if it appears in the lip area, it can enlarge the lip dramatically. Small surface lymphatic malformations can look like small bubbles under the skin.
Lymphatic System:
The lymphatic system forms part of the immune system that identifies and fights off invaders, such as bacteria and viruses. There is a network of vessels within the body through which lymph circulates. Lymph nodes are located in the neck, armpits and groin areas and filter the lymph fluid. When bacteria are found in the lymph fluid while it is being filtered, the lymph nodes release immune cells to fight the infection.
How is a lymphatic malformation diagnosed?
Lymphatic malformations are clearly noticeable. Diagnostic tests such as ultrasound scans, CT scans or MRI Scans may be required to confirm the diagnosis and also to understand the extent of the lymphatic malformation.
What causes lymphatic malformations?
A lymphatic malformation occurs when the lymph vessels fail to form correctly during the first few weeks of pregnancy.
Can they be prevented?
No, as they occur so early in pregnancy, usually before it is confirmed, they cannot be prevented. The effects of the lymphatic malformation however can be reduced or prevented. Lymphatic malformations often swell and become tender or painful when infected. If infections develop, they should be identified and treated promptly.
When might a lymphatic malformation need treatment?
There are circumstances when treatment might be needed.
Location of the malformation
If a lymphatic malformation is in a place where it could interfere with breathing or feeding when it swells, it may need to be treated. This tends to affect lymphatic malformations in the neck area and those in or around the mouth, for instance, affecting the tongue.
Recurrent infections
If a child develops infections frequently and they are not controlled by antibiotics, other options for treatment using sclerotherapy or surgery may be considered.
Appearance
Lymphatic malformations, if large, can be visibly disfiguring and cause problems with unwanted attention at school.
How can lymphatic malformations be treated?
There are three main options for treatment: sclerotherapy, compression and surgical removal. Often they are used in combination, for example, sclerotherapy followed by compression or surgery followed by compression.
Sclerotherapy
Sclerotherapy is a procedure carried out by an interventional radiologist, who blocks the lymphatic vessels by injecting a special substance into them through the skin under general anaesthetic. Once a vessel has been blocked, it shrinks and becomes less noticeable. It may take several sclerotherapy sessions for the malformation to be completely treated and even then, it might grow again.
Compression
Specially made compression garments should help swollen areas and reduce discomfort if worn for 8 to 12 hours a day. Garments are either made to measure or ready made. They need to be replaced regularly as the child grows or the garment wears out. They will also need to be washed daily and dried at room temperature. Compression garments can be helpful in making sport and exercise more comfortable as they support the malformation and reduce swelling.
Surgical removal
Sometimes, particularly if the lymphatic malformation is quite small and is causing problems with function or appearance, it can be removed safely in an operation. Detailed scans will be needed to plan the operation. There will be an amount of scarring after the operation, as with all surgery.
What is the outlook for children with a lymphatic malformation?
Like the options available for treatment, this depends on the size and location of the malformation. Many children treated at this howpital are now leading normal lives, attending schools and college and working.
GUJARATI
લિમ્ફેન્જયોમા
બાળકનું શરીર બે કોષમાંથી આકાર લેતું હોય છે. આમાંથી ચેતાઓ, ધમનીઓ અને લિમ્ફેટીક નામની ગ્રંથિઓના કોષ પણ છૂટા પડતા હોય છે. લિમ્ફેટીક નામની નળીઓ બનાવતા કોષ જે નોર્મલ કોષથી છુટા પડીને ગાંઠ બનાવે તેને લિમ્ફેન્જયોમા કહેવામાં આવે છે. હિમેન્જયોમા એટલે કે લોહીની નળીઓની ગાંઠથી વિપરીત લિમ્ફેન્જયોમા તેની જાતે ક્યારેય મટતું નથી તેના માટે આપરેશન જરૂરી હોય છે. આપરેશન દરમિયાન જા ગાંઠ સંપૂર્ણપણે ન નીકળે તો ભવિષ્યમાં આ રીતની ગાંઠ ફરી થવાની શક્યતા રહે છે. હિમેન્જયોમાની જેમ જ લિમ્ફેન્જયોમા પણ શરીરના કોઈ પણ બાહ્ય અથવાતો આંતરિક અવયવ કે વિભાગમાં થઈ શકે છે. સામાન્ય પણે તો તે ગળામાં અથવા બગલમાં વધુ જાવા મળે છે. •
HINDI
लिम्फेंजीयोमा
बालक का शरीर दो कोशिकाओं में से आकार प्राप्त करता है। इसमें नसें, धमनियाँ और लिम्फेटिक नामक ग्ा्रंथियों की कोशिकाएं अलग हो जाती है। लिम्फेटिक नामक नलिकाएं बनाने वाली कोशिकाएं सामान्य कोशिकाओं से अलग होकर जो गांठ बनाती है उसे लिम्फेंजीयोमा कहा जाता है। हिमेंजीयोमा अर्थात खून की नलिकाओं की गांठ के विपरीत लिम्फेंजीयोमा कभी भी अपने आप ठीक नहीं होता है और उसके लिए ऑपरेशन जरूरी हो जाता है। ऑपरेशन के दौरान यदि गांठ पूरी तरह से नहीं निकाल ली जाती तो भविष्य में गांठ फिर से उभर आने की संभावना बनी रहती है। हिमेंजीयोमा की भान्ति लिम्फेंजीयोमा भी शरीर के किसी भी बाहरी अथवा अंदरुनी भाग में हो सकता है। •
Lymph node enlargement
INFORMATION ALSO AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Everyone has lymph glands. They are in many areas of the body, including the neck, under the arms and in the groin (at the top of each leg). There are also lymph glands in the abdomen, chest and pelvis. Lymph glands are also known as lymph nodes.
Lymph glands become enlarged when the body is fighting an infection, such as a cold. Enlarged lymph glands are particularly common in children as their body takes time to build up immunity to infection.
What causes swollen lymph glands?
Lymph glands swell as part of the body’s response to infection.
Lymph glands are connected by vessels with branches right through the body, similar to the blood circulation system. Rather than carrying blood, these vessels carry a clear liquid called lymph, which contains a high number of white blood cells.
Together with other organs (the spleen, tonsils, adenoids and thymus gland), they form what’s known as the lymphatic system. It has several functions but one of its key roles is fighting infection.
When the body is fighting an infection, the number of white blood cells multiplies rapidly. Some of these cells will go to the lymph gland nearest the infection, which produces enlargement of the lymph glands.
Children often have infections as it takes time for them to build immunity to the viruses and bacteria in the environment. Children who have recently started playgroup or nursery are especially prone because they are coming into contact with a large group of children of the first time.
What are the signs and symptoms of enlarged lymph glands?
The lymph glands will appear swollen. They will also be uncomfortable.
Children frequently get upper respiratory tract infections, such as an ear or throat infection. This means that swollen glands in the neck are particularly common.
How are enlarged lymph glands normally diagnosed?
A child’s doctor will feel their glands to check if they are swollen.
How are enlarged lymph glands treated?
Most cases of enlarged lymph glands are from infection. Once the infection is gone, the glands will get smaller and less tender over time.
If the glands are particularly large, the doctor will check the child for any other symptoms or an underlying cause.
What happens next?
In most cases, enlarged lymph glands are not serious and the condition is common. Following an infection, it is normal for them to take some time for the swelling to go down.
Enlarged lymph glands rarely indicate a more serious problem. Sometimes it is a sign of cancer, such as lymphoma, but this is rare.
GUJARATI
ગળામાં થતી ગાંઠો
ગળામાં થતી ગાંઠો બે પ્રકારની હોય છેઃ
૧. જન્મ જાત ગાંઠઃ
૧) થાઇરોગ્લોસલ સીસ્ટ : ગળાનાં મધ્ય ભાગમાં થતી ગાંઠ થાયરોઇડ ગ્રંથિની ડેવલપમેન્ટની ક્ષતિના કારણે થાય છે. આૅપરેશન કરવાથી જ મટે છે.
૨) ડરમોઈડ સીસ્ટ : આ પણ ગળાનાં મધ્યભાગમાં થતી ગાંઠ છે. જે ઓપરેશનથી મટે છે.
૩) સીસ્ટીક હાઇગ્રોમા : લીમ્ફેટીક નળીઓની બનાવટની ખામીના કારણે, પાણી ભરેલી ગાંઠ ગળામાં ગમે તે જગ્યાએ થાય છે. આવી ગાંઠ સાઈઝમાં નાની અથવા આત્યંત મોટી હોય છે. યોગ્ય સમયે ઓપરેશન કરાવવું જરૂરી છે.
૪) બ્રેન્કયલ સીસ્ટ : આ ગાંઠ ગળાની સાઈડમાં જાવા મળતી હોય છે. ધણીવાર તે નાના છિદ્રનાં રૂપમાં હોય છે. (જેને સાઇનસ કહે છે.)
૫) સરવાઇકલ મેનીન્ગોમાઇલોસીલ : ગળાની પાછળ બરાબર કરોડના મણકા પર થતી જન્મજાત ગાંઠ છે અને આૅપરેશન કરવાથી સંપૂર્ણ સા૨ું થઈ જાય છે.
૨. જન્મ પછી થતી ગળાની ગાંઠો :
૧) લીમ્ફનોડની ગાંઠ : આ ગાંઠ ગળામાં જાવા મળે છે અને તે એક કરતા વધુની સંખ્યામાં અને જુદી જુદી જગ્યાએ પણ હોય છે.
લીમ્ફગ્લેન્ડ – માથા, નાક, કાન, ગળામાં થતા ઇન્ફેક્શનની વેડ ઘાલવાથી થાય છે અને બરાબર દવા કરવાથી મટે છે.
૨) ટી.બી.ની ગાંઠ : ગળામાં ટી.બી.ની ગાંઠ ૧/૨ણી સામાન્ય બીમારી છે. ચોક્કસ નિદાન બાયોપ્સી દ્બા૨ા કરાવી યોગ્ય દવાઓ આપવાથી મટી જાય છે.
૩) કેન્સરની ગાંઠ : બાળકોમાં ગળામાં લીમ્ફોમા નામના કેન્સરને લીધે ગાંઠ થતી હોય છે. તેનું જરૂરી નિદાન બાયોપ્સી વડે કરાવી, દવાઓથી મટાડી શકાય છે. •
HINDI
गले की गांठे
१. जन्मजात गांठ
१) थाइरोग्लोसल सीस्टः गले के मध्य भाग में होनेवाली यह गांठ थाइरोइड ग्ा्रंथी के दोषपूर्ण विकास के कारण होती है और यह केवल ऑपरेशन के द्वारा ही ठीक की जा सकती है।
२) डरमोइड सीस्टः यह भी गले के मध्य भाग में होनेवाली एक गांठ है जो ऑपरेशन के द्वारा ही ठीक की जा सकती है।
३) सीस्टिक हाइग्ा्रोमाः लीम्फेटिक नलिकाओं की बनावट में दोष के कारण, पानी भरी एक गांठ गले के भीतर कहीं भी हो सकती है। यह गांठ आकार में या तो अत्यंत छोटी होती है या अत्यंत बड़ी होती है। उचित समय पर इसका ऑपरेशन कराना आवश्यक है।
४) ब्रेंकीयल सीस्टः यह गले के एक ओर दिखाई देनेबाली गांठ है। कई बार यह एक छोटे से छेद के रूप में होती है (जिसे साइनस कहते हैं)।
५) सरवाइकल मेनींगोमाइलोसीलः गरदन के पिछले हिस्से में ठीक रीढ़ पर होनेवाली जन्मजात गांठ होती है और ऑपरेशन के द्वारा पूर्णरूप से ठीक हो जाती है।
२. जन्म के बाद होनेवाली गले की गांठ
१) लीम्फनोड की गांठः इस प्रकार की गांठ गले के एक ओर देखी जा सकती है।
२) टी.बी. की गांठः गले में टी.बी. की गांठ होना एक सामान्य बीमारी है। सही निदान, बायोप्सी के उपरांत उचित दवाइयों से ठीक हो जाती है।
३) कैंसर की गांठः यह बच्चों के गले में लीम्फोमा नामक कैंसर के कारण होनेवाली गांठ है। इसे आवश्यक निदान, बायोप्सी तथा उचित दवाइयों से ठीक किया जा सकता है।•
Lymphangioma
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Lymphangiomas (Lymphatic malformations; Also read Cystic Hygroma)
A lymphatic malformation is an area in the body containing clear fluid, called lymph. A lymphatic malformation appears as a lump just under the skin, often in the neck or armpit, although they can develop anywhere in the body.
The lump can enlarge the area of the body, for instance, if it appears in the lip area, it can enlarge the lip dramatically. Small surface lymphatic malformations can look like small bubbles under the skin.
Lymphatic System:
The lymphatic system forms part of the immune system that identifies and fights off invaders, such as bacteria and viruses. There is a network of vessels within the body through which lymph circulates. Lymph nodes are located in the neck, armpits and groin areas and filter the lymph fluid. When bacteria are found in the lymph fluid while it is being filtered, the lymph nodes release immune cells to fight the infection.
How is a lymphatic malformation diagnosed?
Lymphatic malformations are clearly noticeable. Diagnostic tests such as ultrasound scans, CT scans or MRI Scans may be required to confirm the diagnosis and also to understand the extent of the lymphatic malformation.
What causes lymphatic malformations?
A lymphatic malformation occurs when the lymph vessels fail to form correctly during the first few weeks of pregnancy.
Can they be prevented?
No, as they occur so early in pregnancy, usually before it is confirmed, they cannot be prevented. The effects of the lymphatic malformation however can be reduced or prevented. Lymphatic malformations often swell and become tender or painful when infected. If infections develop, they should be identified and treated promptly.
When might a lymphatic malformation need treatment?
There are circumstances when treatment might be needed.
Location of the malformation
If a lymphatic malformation is in a place where it could interfere with breathing or feeding when it swells, it may need to be treated. This tends to affect lymphatic malformations in the neck area and those in or around the mouth, for instance, affecting the tongue.
Recurrent infections
If a child develops infections frequently and they are not controlled by antibiotics, other options for treatment using sclerotherapy or surgery may be considered.
Appearance
Lymphatic malformations, if large, can be visibly disfiguring and cause problems with unwanted attention at school.
How can lymphatic malformations be treated?
There are three main options for treatment: sclerotherapy, compression and surgical removal. Often they are used in combination, for example, sclerotherapy followed by compression or surgery followed by compression.
Sclerotherapy
Sclerotherapy is a procedure carried out by an interventional radiologist, who blocks the lymphatic vessels by injecting a special substance into them through the skin under general anaesthetic. Once a vessel has been blocked, it shrinks and becomes less noticeable. It may take several sclerotherapy sessions for the malformation to be completely treated and even then, it might grow again.
Compression
Specially made compression garments should help swollen areas and reduce discomfort if worn for 8 to 12 hours a day. Garments are either made to measure or ready made. They need to be replaced regularly as the child grows or the garment wears out. They will also need to be washed daily and dried at room temperature. Compression garments can be helpful in making sport and exercise more comfortable as they support the malformation and reduce swelling.
Surgical removal
Sometimes, particularly if the lymphatic malformation is quite small and is causing problems with function or appearance, it can be removed safely in an operation. Detailed scans will be needed to plan the operation. There will be an amount of scarring after the operation, as with all surgery.
What is the outlook for children with a lymphatic malformation?
Like the options available for treatment, this depends on the size and location of the malformation. Many children treated at this howpital are now leading normal lives, attending schools and college and working.

 Large Lymphangio-Hemangiomas
Large Lymphangio-Hemangiomas

 Lymphangiomas in the neck
Lymphangiomas in the neck
 Large Lymphangioma in the neck
Large Lymphangioma in the neck
 Lymphangioma over the arm
Lymphangioma over the arm
 Abdominal Lymphangioma
Abdominal Lymphangioma
GUJARATI
લિમ્ફેન્જયોમા
બાળકનું શરીર બે કોષમાંથી આકાર લેતું હોય છે. આમાંથી ચેતાઓ, ધમનીઓ અને લિમ્ફેટીક નામની ગ્રંથિઓના કોષ પણ છૂટા પડતા હોય છે. લિમ્ફેટીક નામની નળીઓ બનાવતા કોષ જે નોર્મલ કોષથી છુટા પડીને ગાંઠ બનાવે તેને લિમ્ફેન્જયોમા કહેવામાં આવે છે. હિમેન્જયોમા એટલે કે લોહીની નળીઓની ગાંઠથી વિપરીત લિમ્ફેન્જયોમા તેની જાતે ક્યારેય મટતું નથી તેના માટે આપરેશન જરૂરી હોય છે. આપરેશન દરમિયાન જા ગાંઠ સંપૂર્ણપણે ન નીકળે તો ભવિષ્યમાં આ રીતની ગાંઠ ફરી થવાની શક્યતા રહે છે. હિમેન્જયોમાની જેમ જ લિમ્ફેન્જયોમા પણ શરીરના કોઈ પણ બાહ્ય અથવાતો આંતરિક અવયવ કે વિભાગમાં થઈ શકે છે. સામાન્ય પણે તો તે ગળામાં અથવા બગલમાં વધુ જાવા મળે છે. •
HINDI
लिम्फेंजीयोमा
बालक का शरीर दो कोशिकाओं में से आकार प्राप्त करता है। इसमें नसें, धमनियाँ और लिम्फेटिक नामक ग्ा्रंथियों की कोशिकाएं अलग हो जाती है। लिम्फेटिक नामक नलिकाएं बनाने वाली कोशिकाएं सामान्य कोशिकाओं से अलग होकर जो गांठ बनाती है उसे लिम्फेंजीयोमा कहा जाता है। हिमेंजीयोमा अर्थात खून की नलिकाओं की गांठ के विपरीत लिम्फेंजीयोमा कभी भी अपने आप ठीक नहीं होता है और उसके लिए ऑपरेशन जरूरी हो जाता है। ऑपरेशन के दौरान यदि गांठ पूरी तरह से नहीं निकाल ली जाती तो भविष्य में गांठ फिर से उभर आने की संभावना बनी रहती है। हिमेंजीयोमा की भान्ति लिम्फेंजीयोमा भी शरीर के किसी भी बाहरी अथवा अंदरुनी भाग में हो सकता है। •
Lip (Cleft Lip)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is a cleft lip repair?
Cleft lip repair is an operation to reconstruct the shape of the lip . If there is a cleft palate as well, then the front half (anterior) of the palate is also repaired. The earliest we do the operation is when babies are approximately three months of age. Babies are usually in hospital for about 3-4 days after the operation.
Bilateral Cleft Lip

Unilateral Cleft Lip

Unilateral Cleft Lip
What does the operation involve?
The operation involves joining the tissues that have not joined before birth. The surgeon may use an operating microscope to allow the small structures to be accurately joined. The operation usually takes from one to two hours, depending on the extent of the cleft.
What anaesthetic is used?
Your baby is given a general anaesthetic by an anaesthetist who specializes in giving anaesthetics to babies and children.
Are there any risks?
There is a small risk of infection following the operation, but your baby will be given an antibiotic injection during the operation, and continue to take antibiotics afterwards in the form of medicine. Every anaesthetic carries a risk of complications, but this is very small.
Your baby’s mouth will be sore after the operations, partly due to the operation itself, but also because the surgeon will need to move it about to repair the lip. The nurses will give pain relief medicine, so that he or she is not uncomfortable, particularly when feeding.
When can my baby feed?
We are happy for your baby to feed as soon as he or she is awake after the anaesthetic. The first feed may be difficult, partly because the lip is numb from the operation.
What happens afterwards?
When your baby has returned to the ward, he or she may be offered fluids that may be taken more easily from a spoon or syringe. If your baby is reluctant to drink it may be necessary to give extra fluid through the drip. The drip will be removed once he or she is drinking well again. It is important to give your baby some cooled, boiled water to drink after each feed and medicine to keep the inside of the mouth clean.
Soon after the operation there may be some bleeding but this usually stops quickly. Only very rarely will any further measures be necessary to stop the bleeding. Your child’s lip may look swollen and bruised for the first few days after the operation, but this will soon go down.
A course of antibiotics will be prescribed to reduce the risk of infection. You will need to continue giving this antibiotic medicine for a few days after leaving hospital to complete the course.
Unilateral Cleft Lip (After surgery)

Bilateral Cleft Lip (After Surgery)
When you get home…
By the time your child goes home he or she should be getting back to a normal feeding pattern. It is important to make sure your child is drinking enough. His or her lip may be swollen after the operation and the shape of his or her mouth may be different, but your child will soon adapt. You will be called to hospital for removal of the stitches on the 7th day following surgery.
GUJARATI
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું દર છસો એ એક બાળકમાં જાવામાં આવે છે. ઘણીવાર બાળકનો ફક્ત હોંઠ જ કપાયેલો હોય છે. જ્યારે ઘણીવાર હોંઠ, તાળવું અને પેઢું ત્રણે કપાયેલા હોય છે. માતા અથવા પિતામાં જા કપાયેલો હોંઠ અને ફાટેલું તાળવું હોય તો તેમનાં બાળકોમાં પણ આ ખોડ આવવાની શક્યતા બીજા બાળકો કરતાં વધારે રહેલ છે. ફાટેલું તાળવું હોવાથી બાળક સ્તનપાન નથી કરી શકતું તેથી આવા બાળકોને એક વિશેષ પ્રકારની બોટલ અથવા વાટકી અને ચમચીથી દૂધ પીવડાવવું જાઈએ. સ્તનપાન કરાવવાથી અથવા સાદી દૂધની બાટલીઓથી ઘણીવાર બાળકને આંતરાશ જઈ બાળકની જિંદગીને જાખમ પણ ઊંભું થતું હોય છે. કપાયેલા હોંઠનું આૅપરેશન ત્રણ મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાનું આૅપરેશન નવ થી બાર મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાના આૅપરેશન પછી બાળકોને ઘણીવાર વાંકાચૂકા દાંતની સારાવાર કરવાની જરૂર પડે છે. સ્પીચ થેરાપીની પણ જરૂર પડી શકે છે. •
HINDI
कटा होंठ और फटा तालु
कटा होंठ और फटा तालु हर ६०० में से एक बच्चे में देखा गया है। कई बार बालक का केवल होंठ ही कटा हुआ होता है। जबकि कभी-कभी होंठ, तालु और मसूड़े तीनों ही फटे हुए होते हैं। यदि माता या पिता में से किसी को भी कटे होंठ या फटे हुए तालु की समस्या है तो, उनके बच्चों में अन्य बच्चों के अपेक्षा यह दोष होने की संभावना अधिक रहती है। कटे होंठ या फटे तालु के साथ जन्मे शिशु को स्तनपान करने में तकलीफ होती है। अतः ऐसे बालक को विशेष प्रकार की बोतल या कटोरी-चम्मच से दूध पिलाना पड़ता है। सामान्य स्तनपान अथवा दूध की बोतल से दूध पिलाने पर कई बार दूध बच्चे के फेफडे में जाने की संभावना है और बच्चे की जान को खतरा पैदा कर सकता है। कटे होंठ का ऑपरेशन तीन महीने की उम्र में किया जाता है। फटे तालु का ऑपरेशन नौ से बारह महीने की आयु में किया जाता है। फटे तालु के कारण कई बार दांतों का उपचार अर्थात टेढ़े-मेढ़े दांतों के उपचार की आवश्यकता होती है। स्पीच थेरापी की भी आवश्यकता हो सकती है।•
Large Head (Hydrocephalus)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is hydrocephalus?
Hydrocephalus occurs when either too much cerebrospinal fluid (CSF) is produced (very rare) or when it is stopped from circulating or being re-absorbed. The CSF builds up within the ventricles (cavities) of the brain resulting in increased pressure on the brain. In babies, this also causes the head to enlarge.
CSF is a watery liquid that surrounds the brain and spinal cord, acting as a ‘cushion’. It also supplies nutrients to the brain.
What causes hydrocephalus?
The most common causes are:
- Congenital – This means that your child was born with hydrocephalus. Children born with spina bifida often develop hydrocephalus. This does not mean that all children with hydrocephalus also have spina bifida.
- Prematurity – Hydrocephalus can occur as a complication of being born too early, and when there has been bleeding in the brain.
- Meningitis – Hydrocephalus can occur as a complication of meningitis as the infection may cause a problem with reabsorption of CSF.
- As a complication from a brain tumour – this does not mean children with hydrocephalus develop brain tumours.
- Unknown – In many cases, we do not know what caused the hydrocephalus.
A child with massive hydrocephalus
MRI Scan of a child with hydrocephalus because of a brain tumour
How is hydrocephalus diagnosed?
It is usually diagnosed by an increasing head circumference in infants, an ultrasound scan, a CT scan or sometimes an MRI scan.
How is hydrocephalus treated?
If hydrocephalus is not treated, your child’s head would get larger and the pressure on the brain would interfere with his or her development. In severe cases, this can result in permanent brain damage or visual problems. The aim of treatment is to reduce the pressure on the brain by draining the CSF away.
The fluid is drained away using a ‘shunt’, which is a long tube made of silicone. It is inserted in to the ventricles in an operation and drains the CSF away to the abdomen. The shunt contains a valve so that the fluid can only drain away from the head at the desired rate.
The operation
Part of your child’s hair, behind the ear, will be shaved and he or she will have an incision (cut) there in a horseshoe shape and a small incision on his or her abdomen.
Your child will have this operation under a general anaesthetic. The operation takes about 45 min to an hour. At the time of surgery fluid that is drained from the brain will be sent to the laboratory for examination.
What happens after the operation?
Close observation will be needed following surgery. Most children are able to take oral feeds the same evening of the operation. The usual stay in hospital is four to six days.
To begin with, the area around the top of the shunt may be slightly raised, but as the swelling settles and your child’s hair grows back you will not notice this. As your child grows, the area will become less prominent.
Going home
Your child may have dissolvable stitches or they may have stitches that need to be removed seven days after the operation.
Complications of a shunt
There can be complications to having a shunt inserted, of which you should be aware. The most common could be either an infection or a blocked shunt.
Symptoms of Infection
The symptoms of an infection in the shunt may include:
- Headache
- Irritability
- High temperature (over 37°C)
- Not feeding well
- Possibly vomiting
- Possibly drowsy
Symptoms of a blocked shunt
In babies:
- A bulging fontanelle (soft part of the top of the head)
- Vomiting
- Crying and irritability
- Becoming sleepy (less responsive)
- Looking pale
- Increased head size
In toddlers and children:
- Headache
- Vomiting
- Tiredness
- Drowsy
- Looking pale
GUJARATI
માથું મોટું હોવું
બાળકનું માથું મોટું હોવું એક ચિંતાનો વિષય જરૂર છે, અને તેનાં માટે ડાક્ટરની સલાહ જરૂરી છે. જન્મથીજ ડાક્ટર માથું અને છાતીના માપનો રેકોર્ડ રાખે છે અને તેને સ્ટાન્ડર્ડ ચાર્ટ સાથે સરખાવે છે. તેના પ્રમાણે સતત વધતાં માથા માટે જરૂરી તપાસ કરાવવી પડે છે.
માથું મોટું થવાનું સૌથી મુખ્ય કારણ નવજાત બાળકોના મગજની અંદર આવેલ પાણી (C.S.F.) નો ભરાવો છે. જેને હાઈડ્રોકેફલસ કહે છે. આમાં બાળકનું માથું નિયમિત ગતિથી વધ્યાં કરે છે. બીજા કારણોમાં બાળકને જન્મ પછી બ્રેન હેમરેજ થયું હોય તો પણ માથું મોટું થાય છે. જ્વલ્લે જ બાળકને બ્રેન કેન્સર જેવી બીમારીથી માથું મોટું થઈ શકે છે.
હાઈડ્રોકેફલસ સૌથી સામાન્ય કારણ છે. અને તેનું સચોટ નિદાન નાના બાળકોમાં સોનોગ્રાફી દ્વારા અને મોટા બાળકોમાં સી.ટી.સ્કેન અથવા એમ.આર.આઈ.થી થઈ શકે છે.
બાળકોનાં સર્જન આવા કેસમાં એક શંટ મૂકવાની સલાહ આપે છે જેમાં એક પાતળી ટ્યુબ દ્વારા માથાના વધારાના પાણીને પેટમાં ડાયવર્ટ કરાય છે. આ ટ્યુબને વી.પી. શંટ કહે છે.તેનું રેગ્યુલર ચેકઅપ કરાવતાં રહેવું જરૂરી છે. •
HINDI
बडा सिर (जल शीर्ष)
बच्चे के सिर का बड़ा होना चिंता का विषय जरुर है और इसके लिए डॉक्टर से परामर्श जरुरी है। बच्चे के जन्म लेते ही डॉक्टर उसके सिर तथा छाती के माप का रिकार्ड रखते है और उसकी तुलना मानक चार्ट से करते रहते हैं। अगर सिर के माप में निरंतर वृद्धि हो तो जाँच आवश्यक होती है।
इसका प्रमुख कारण नवजात शिशु के मस्तिष्क में जल भराव (C.S.F.) जिसे हाइड्रोसीफेलस कहते हैं। इसमें बच्चे का माथा नियमित गति से बढ़ता रहता है। इसका दूसरा कारण जन्म के समय बच्चे को ब्रेन हेमरेज होना भी हो सकता है। ब्रेन कैंसर जैसी बीमारी के कारण सिर का बड़ा हो जाना बच्चों में कम ही पाया जाता है।
हाइड्रोसीफेलस एक सर्वसामान्य कारण है। बच्चों के मामले में इसका सटीक निदान सोनोग्राफी के द्वारा तथा वयस्कों में सी.टी. स्कैन अथवा एम.आर.आई के द्वारा किया जाता है।
बालरोग सर्जन ऐसे मामलों में एक सादा सा शंट लगाने की सलाह देते हैं। इस प्रक्रिया में एक नलीका के माध्यम से माथे का पानी पेट में डायवर्ट किया जाता है। इस नलिका को वी.पी. शंट कहते हैं। इस में नियमित चेकअप की आवश्यकता होती है। •
Mitrofanoff Procedure
What is a Mitrofanoff and why might my child need one?
The Mitrofanoff procedure creates a channel into the bladder through which a catheter (thin, plastic tube) can be inserted to empty the bladder of urine, instead of passing urine through the urethra. This channel – which looks like an extra belly button – is usually referred to as a ‘Mitrofanoff’, and is created in an operation under general anaesthetic.
Children who are incontinent (wet) may benefit from this procedure. It allows the bladder to be emptied several times a day, reducing the chance of the bladder leaking urine. It can be psychologically easier and physically less uncomfortable to insert a catheter into the Mitrofanoff rather than the urethra. It can also allow older children to lead a more normal life. The Mitrofanoff procedure is often used for children with bladder problems due to spina bifida, bladder exstrophy or bladder obstruction (posterior urethral valves).
What does the operation involve?
The surgeon will disconnect your child’s appendix from its usual position on the large intestine and open it up to form a tube. He or she will then connect one end to a small incision (cut) in your child’s bladder and the other end to another small incision in your child’s abdomen. The surgeon will also create a ‘valve’ where the tube joins the bladder, which squeezes shut as the bladder fills with urine. This will reduce the chance of urine leaking from the Mitrofanoff.
If your child has already had his or her appendix removed or if it is not suitable, the surgeon may need to use a piece of the small intestine to create the channel. The usual hospital stay is about seven days.
Are there any risks?
All treatments carry an element of risk, but this must be balanced against the quality of life without treatment. All surgery carries a risk of bleeding during or after the operation. Every anaesthetic carries a risk of complications, but this is very small. After an anaesthetic, your child may feel sick and vomit. He or she may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe.
Are there any alternatives?
Your child could catheterise using the urethra, which some children find quite difficult. Another alternative is to do nothing, and allow your child to remain wet.
What happens afterwards?
For the first day or two, he or she will have a drip giving fluids and medication, until the bowel starts to recover. The drip will be removed when your child starts eating and drinking again.
The surgeon will have inserted a catheter into the Mitrofanoff to keep it open. This should stay in place for three to four weeks after the operation.
Meningomyelocele
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is spinal dysraphism?
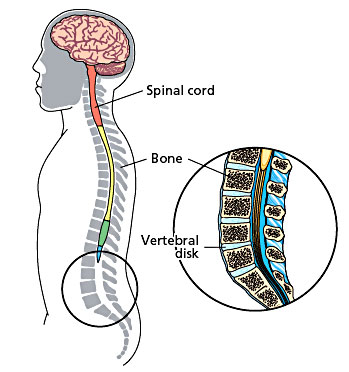
In early development, the brain and spinal cord start as a tube-like structure called the ‘neural tube’ that is open at either end. These openings close within the first weeks of pregnancy, and the neural tube continues to grow and fold, eventually forming the brain and spinal cord.
If the tube fails to close properly, this results in a group of problems called ‘neural tube defects’. Spinal dysphraism is the term used to describe what happens when the spinal column (backbone) fails to form properly. This happens very early in pregnancy, before the end of the fourth week. There are two types of spinal dysphraism: open, also called spina bifida aperta or myelomeningocele, or closed, also called spina bifida occulta.
The open myelomeningocele type accounts for 75 per cent of all cases of spina bifida. In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
Open Neural Tube Defects
In closed spinal dysphraism, the spinal cord (a tube-like structure containing nerves) and its coverings do not protrude through the back unlike in the open type. On its own, closed spinal dysphraism is unlikely to cause any problems, and many people have the condition without ever knowing it. However, it can be associated with other conditions that could lead to problems with movement and bladder control.
Closed Neural Tube Defect
Many children have a ‘tethered cord’, which is the term used when the lower end of the spinal cord is attached to the lower bones of the spinal column rather than hanging freely as it should. Normally the spinal column grows more quickly than the spinal cord, so that by the time the baby is born, the spinal cord has moved higher up the spinal column. If the cord is tethered, the spinal cord and nerves are stretched, reducing their ability to carry messages to and from the brain and causing pain. Growth spurts can stretch the spinal cord and nerves, causing problems with leg movement and bladder and bowel control.
What are the symptoms of closed spinal dysphraism?
In many people, there may be no symptoms at all. However, a birthmark, hairy patch or dermal sinus in the lower back area may lead doctors to suspect that a child has closed spinal dysphraism. Other children may develop repeated bouts of meningitis for which no cause can be found or may have problems keeping dry (urinary incontinence) that cannot be explained. If it not diagnosed until early childhood, the first sign might be weakness or unevenness of the legs or talipes (clubfeet) affecting one of both limbs. Back or leg pain might be a problem too. If these symptoms are due to a tethered cord they may get worse as the child grows. Treatment by surgery tends to be suggested only when a child shows signs that his or her condition is getting worse, for instance, movement becomes more problematic or urinary incontinence is making everyday life more difficult or painful.
How is closed spinal dysphraism diagnosed?
Initial suspicions may be raised through clinical examination but imaging scans are used to confirm the extent of the problem. Ultrasound or magnetic resonance imaging scans are the usual methods used.
How is closed spinal dysphraism treated?
If there are clinical symptoms that are getting worse, these may be reduced using surgery to release the tethered cord. This relieves pressure on the spinal cord and nerves and can improve leg symptoms in many cases. It is less successful in improving bladder and bowel problems but usually stops them getting any worse over time.
What does the operation involve?
At surgery, the surgeon will release the spinal cord from where it is tethered so that it can move as the child grows. If possible, the surgeon will reduce the size of a lipoma to relieve pressure on the spinal cord. After the operation, the incision on your child’s back will be closed and covered with a dressing.
Are there any risks?
The operation to detach a tethered cord is very specialized due to the complex arrangements of nerves in the area. There is always a risk that the nerves, or the spinal cord itself, could be damaged in the operation but if the surgeon believes that this may happen, he or she will stop the procedure.
The aim of the operation is to stop your child’s symptoms from them getting any worse. There is no guarantee that this operation will remove your child’s symptoms or even improve them. This operation tends to improve leg symptoms more frequently than bladder and bowel symptoms.
What is the outlook for children with closed spinal dysphraism?
Orthopaedic problems
In some cases, children may have developed leg and foot problems as a result of the closed spinal dysphraism. These can include clawing of the toes or very high arches, which in turn can lead to tightening of the Achilles tendon at the heel. This can affect one leg or both and if it is severe, we may refer your child to an orthopaedic surgeon for further treatment.
Where a child has scoliosis as a result of the closed spinal dysphraism, further treatment by an orthopaedic spinal surgeon may be required. Sometimes however, treatment of the dysphraism may reduce or even improve the progression of the spine curvature.
Bladder and bowel control
The nerves that control bladder and bowel function are contained in the lower portion of the spinal cord and so can be affected by closed spinal dysphraism. The degree to which bladder and bowel control is affected depends on the severity of the defect.
Problems associated with the bladder are largely due to incomplete emptying, which is caused by the messages from the bladder not being transmitted to the brain well enough. Incomplete emptying of the bladder can lead to urinary tract infections (UTIs) and backflow of urine towards the kidneys (reflux), sometimes severe enough to damage the kidney. Signs of bladder problems include: urinary incontinence or dribbling, recurrent infections, bedwetting at night, needing to urinate frequently or having difficulties potty training. Bowel incontinence (soiling) is a less common problem, and rarely occurs if there are no bladder control problems. Early diagnosis and treatment can help reduce these problems but rarely solve them completely.
Movement
Closed spinal dysphraism can lead to muscle wastage on one side, affecting the buttocks and calf. This is caused by the muscles on one side being used more and therefore becoming stronger than the other, due to the stretching of the nerves leading away from the spinal cord when the cord is tethered. This can result in numbness, unbalanced walking, painless skin lesions, stiffness and pain in the lower limbs and back, sometimes relieved with odd postures or lying down. The physiotherapist will advise you about strengthening these muscles and improving their function as much as possible.
What about future pregnancies?
There is now evidence that an adequate intake of folic acid can dramatically reduce the risk of neural tube defects occurring in future pregnancies. If you are planning a further pregnancy, we recommend that you take 4mg of folic acid each day for at least three months before conception and for the first three months of pregnancy. This dose is higher than the standard recommendation for women who have not previously had a child with spina bifida. If you have any concerns about future pregnancies, please feel free to contact us.
What is a myelomeningocele?
In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
How is myelomeningocele treated?
Without the protective covering of skin, the spinal cord will become further damaged, spinal fluid often leaks from the area and there is a very high risk of infection. Surgery is usually recommended within the first few days of life. The aim of surgery at this stage is to put the spinal cord back into the spinal canal and repair the defect in the back so that the area is covered with normal, healthy skin.
The physiotherapist will see your child after the operation. He or she will assess how much strength your child has in each muscle group and measure his or her sense of feel. When taken together, muscle strength, sensation and reflexes give us a picture of how well the messages are getting from the brain to the arms and legs via the spinal cord. The physiotherapist will also give advice on how to position and handle your child to stretch out tight muscles and to help with normal development.
Once your baby is recovering well, you will both be able to go home. We will need you to come back to the hospital between 10 and 14 days after the operation so that we can check the operation site, carry out an ultrasound scan of your baby’s head and measure his or her head circumference. The child is followed up on a regular basis.
What problems can myelomeningocele cause?
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Bladder function
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Hydrocephalus
The circulation of cerebrospinal fluid (CSF) is often disturbed in children with myelomeningocele. Either at birth or in the days and weeks following surgery, fluid may start to build up within the brain. This is called hydrocephalus and can result in increased pressure in the brain. If this occurs, an operation to place a shunt tube to divert the excess fluid from the brain to the abdomen is needed. This operation is needed in about 60 per cent of children with myelomeningocele.
Mobility
Myelomeningocele affects each child differently, and how each child moves around will vary too. Some children will need splints or walking aids, and others may move around more easily in a wheelchair. Your doctor will speak to you about how your child’s condition will affect their mobility.
What is the outlook for children with myelomeningocele?
The outlook for children with myelomeningocele has improved dramatically in recent decades. Intellectual prognosis is very good for the majority of children, most of whom will go on to full time education. Recreational and employment opportunities are better now than at any time in the past. However, this is a multidisciplinary approach and team work with parental support is a must for a good outcome.
GUJARATI
બરડા પરની ગાંઠ
સ્પાઇના બાઇફીડા કરોડરજ્જુની જન્મજાત ખોડ છે જેમાં કરોડનાં મણકાં ખુલ્લા રહી જાય છે. આ કારણે કરોડરજ્જુની નસો અને તેનાં પરનાં આવરણો કરોડનાં મણકાંની બહાર આવે છે. આ ખોડ નવજાત બાળકનાં બરડા પર ગાંઠના રૂપમાં આવે છે. સામાન્ય રીતે આવી ગાંઠ કરોડનાં મણકાંના કોઈપણ ભાગ-ગરદન, છાતી, કમર અને કમરનાં નીચેના ભાગમાં હોઈ શકે છે.
કરોડરજ્જુ અને તેની નસોનો વિકાસ ખામીયુક્ત હોવાનાં કારણે બાળકનાં બંને પગ ઓછા યા વધુ પ્રમાણમાં લકવાગ્રસ્ત હોઈ શકે છે અને ઘણી વાર પેશાબ-સંડાસ કંટ્રોલ કરતાં સ્નાયુ પણ નબળાં હોય છે. સ્નાયુઓની આ ખામી બરડાંની ગાંઠનું આૅપરેશન કરવાથી પણ સારી નથી કરી શકાતી અને બાળકને તેની સાથે જીવતાં શીખવું પડે છે.
સ્પાઇનાં બાઇફીડાવાળા ૫૦% થી ૬૦% બાળકોને માથામાં પાણી ભરાવાની શક્યતા પણ રહે છે. જેને હાઈડ્રોકેફલસ કહે છે. આને શંટ આૅપરેશન દ્વારા સા૨ું કરી શકાય છે. •
HINDI
पीठ पर गांठ (न्यूरल ट्यूब में दोष)
स्पाइना बाईफीडा रीड की हड्डी का जन्मजात दोष है, जिसमें रीड़ की हड्डी के मनकें खुले रह जाते हैं। इससे रीड की हड्डी की नसें और उसका ऊपरी भाग रीड की हड्डी के मनकों से बाहर निकल आता है। यह दोष नवजात शिशु की पीठ पर एक गांठ के रूप में उभर कर दिखाई देता है। सामान्य रूप से यह गांठ रीड़ की हड्डी के मनकें के किसी भी हिस्से – गरदन, छाती, कमर और कमर के नीचले हिस्से में हो सकती है।
रीड की हड्डी और उसकी नसों का विकास दोषपूर्ण होने के कारण बच्चे के पैरों की मांसपेशियाँ कमजोर हो सकती है, जिससे उसके शरीर का थोड़ा या अधिक हिस्सा लकवा ग्रस्त होता है। मल-मूत्र पर भी उसका नियंत्रण नहीं रहता। इस प्रकार का न्यूरोलोजिकल दोष पीठ की गांठ के ऑपरेशन से भी ठीक नहीं किया जा सकता और बच्चे को इस रोग के साथ जीना सीखना पड़ता है।
स्पाईना बाईफीड़ा रोग से ग्रस्त ५०% से ६०% बच्चों के सिर में पानी का भराव होने की संभावना होती है, जिसे हाइड्रोकेफेलस कहते हैं। शंट ऑपरेशन से इसे ठीक किया जा सकता है। •
Malrotation
What is malrotation?
Malrotation is an abnormality of the bowel, which happens while the baby is developing in the womb.
Early in pregnancy, the bowel is a long straight tube leading from the stomach to the rectum. The bowel then moves into the umbilical cord temporarily while it develops into the large and small bowel.
Around the tenth week of pregnancy, the bowel moves back into the abdomen and coils up to fit into the limited space there. If the bowel does not coil up in the correct position, this is called malrotation.
What is volvulus?
This is a complication of malrotation and occurs when the bowel twists so the blood supply to that part of the bowel is cut off.
What are the symptoms of malrotation and volvulus?
Malrotation may not have any symptoms. Many people are never diagnosed with malrotation because it causes no problems. However, bands of tissue (adhesions), which block the first part of the small bowel (duodenum), can develop. This means food cannot easily pass through the duodenum to the rest of the bowel for digestion.
The symptoms of volvulus are usually the first sign of malrotation. They include sudden bouts of crying and pulling the legs into the body, which then stop suddenly. This is caused by cramps, as the bowel cannot push food and liquid past the twisted section of bowel. Vomiting is another symptom of volvulus, as your child is unable to digest food as usual.
If the condition is not treated, the child will become dehydrated which can be life-threatening. the symptoms of dehydration may appear in phases, and include lethargy and reduced urine output.
What causes malrotation and volvulus and how common are they?
We do not know exactly what causes malrotation and volvulus, but it is not due to anything that happened during pregnancy. Malrotation affects about one in every 2,500 to 3,000 babies, and boys and girls in equal numbers.
How is malrotation and volvulus diagnosed?
Malrotation and volvulus are usually diagnosed using x-rays. A barium x-ray may also be useful as it shows the feeds being unable to pass the twisted part of the bowel. The doctor may also suggest an ultrasound scan to get an indirect evidence.
How are they treated and are there any alternatives?
Adhesions and volvulus are usually treated in an operation under general anaesthetic. They both require emergency treatment as the bowel can die off from lack of blood-supply, which would stop it functioning properly and can also lead to problems with infection. The effects of the adhesions and volvulus, like dehydration due to the lack of fluids being absorbed, can become serious quite quickly in children, and so there are no alternatives to the operation.
What happens before the operation?
If your child is dehydrated, he or she will need a ‘drip’ of fluids for a while before the operation. Your child will also need a nasogastric tube, which is passed up the nose, down the food-pipe and into the stomach. This will drain off the stomach and bowel contents and ‘vent’ any air that has built up, which will make your child more comfortable.
What does the operation involve?
The operation is called a Ladd procedure. The surgeon will straighten out the twisted bowel and separate any adhesions. If the bowel looks healthy, the surgeon will coil it back into the abdomen. Usually the surgeon will also remove the appendix during this operation, as it is often on the wrong side of the body in malrotation, which could cause problems in diagnosing appendicitis later in life.
In a complicated condition the surgeon will remove any parts of the bowel where tissue has died. The amount can vary, but the surgeon will leave as much of the bowel as possible. If the surgeon has to remove a large part of the intestine, he or she may need to create an artificial way of disposing of waste matter, called a ‘stoma’.
Are there any risks?
All surgery carries a small risk of bleeding during or after the operation. Every anaesthetic carries a risk of complications, but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications.
What happens afterwards?
For the first few days, your child will need to be fed through a tube into his or her veins so the stomach and bowel can start to heal. After a while, you can start to feed your child again, starting with small amounts, and increasing the amount as he or she tolerates it.
When you go home
The stitches used during the operation will dissolve on their own so there is no need to have them removed. If possible, keep the operation site clean and dry for two to three days to let the operation site heal properly. If your child needs to have a bath, do not soak the area until the operation site has settled down.
What is the outlook for children with malrotation and volvulus?
The outlook depends on how quickly the malrotation and volvulus are diagnosed as this in turn can influence the amount of damage to the bowel.
Meckel’s Diverticulum
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Meckel’s diverticulum is one of the most common congenital digestive system disorders – congenital means that the disorder was present at birth. When your child’s small intestine was developing, a small pouch formed consisting of tissue from elsewhere in the body. Usually the pouch – also known as Meckel’s diverticulum – is formed from tissue similar to that found in the pancreas or stomach.
In many cases, Meckel’s diverticulum does not cause any problems. Up to two per cent of the population will have a Meckel’sdiverticulum.
What causes Meckel’s diverticulum?
We do not really know why this pouch forms during pregnancy. The intestines form early in pregnancy as a long straight tube – before the tenth week they grow and bend to develop into the separate organs making up the digestive system. The Meckel’s diverticulum occurs at this point of bending, and is a leftover bit of development.
What are the signs and symptoms of Meckel’s diverticulum?
Many people will be unaware that they have this pouch in their small intestine as it causes no problems at all. However, in a small proportion of children, the pouch releases acid like the stomach which over time can cause ulcers to develop in the small intestine. These can worsen and bleed which shows as large amount of painless blood in the stools. It can also leak the liquid inside the small intestine into the abdomen, leading to a serious infection called peritonitis.
The pouch can also twist leading to a condition called volvulus. Twisting can cause the blood supply to the intestine to be cut off, which can be a life threatening condition. It can also fold inwards leading to a condition called intussusception. Symptoms of volvulus and intussusception can include sudden bouts of crying and pulling the legs into the body which then stop suddenly.
As little or no food or liquid can pass the twisted or blocked portion, your child may also pass little or no faeces (stools). This causes cramps, as the bowel cannot push food and liquid past the twisted section of bowel. The twisting also cuts off the blood supply to the bowel, which can lead to the tissues in the bowel becoming inflamed and starting to die.
Vomiting, especially green vomit is another symptom of volvulus and intussusception, as your child is unable to digest food as usual. If the condition is not treated, your child will become dehydrated which can be life threatening. The symptoms of dehydration may appear in phases and include lethargy, reduced urine output and dehydration.
How is Meckel’s diverticulum diagnosed?
If your child has a blockage an x-ray or ultrasound scan will be used to identify the affected part of the intestine.
Sometimes a test called a Meckel’s scan is used to show your child’s intestine and whether it contains a certain type of tissue that can cause bleeding. The scan works by injecting a substance called an isotope into your child’s veins, which then travels through the blood supply to the intestine. A series of pictures are taken while the isotope is passing through the intestine. This scan may not always identify the pouch.
Laparoscopy is diagnostic and therapeutic (curative) for Meckel’s diverticulum. This involves inserting a small telescope and camera inside your child’s abdomen. Meckel’s diverticulum may also be discovered incidentally during another procedure like an appendicectomy.
How is Meckel’s diverticulum treated?
If the Meckel’s diverticulum is causing problems, your child will need an operation to correct it. The Meckel’s diverticulum is cut at its base where it is attached to the small intestine and the defect is then closed with stiches. Some times if the base is very wide, 1 – 2 cm of the small intestine segment along with the Meckel’s diverticulum may be needed to be removed and the rest of the intestine reconnected with stiches.
What happens next?
Immediately after the operation, your child will be kept fasted so the stomach and bowel can start to heal. Once the bowel starts to work, the child can start to feed your child again, starting with small amounts, and increasing the amount as tolerated.
Outlook:
The outlook depends on how quickly the problem was diagnosed and treated as this in turn can influence the amount of damage to the bowel.
 Meckel’s Diverticulum
Meckel’s Diverticulum
 Perforation caused in Meckel’s Diverticulum
Perforation caused in Meckel’s Diverticulum
 Meckel’s Diverticulum (At Laparoscopy)
Meckel’s Diverticulum (At Laparoscopy)
 Meckel’s Diverticulum causing obstruction of intestine (At Laparoscopy)
Meckel’s Diverticulum causing obstruction of intestine (At Laparoscopy)
 Meckel’s Diverticulum (At Laparoscopy)
Meckel’s Diverticulum (At Laparoscopy)
 Torsion caused in Meckel’s Diverticulum
Torsion caused in Meckel’s Diverticulum
GUJARATI
મેકલ્સ ડાયવર્ટીક્યુલમ
આ આંતરડાની એક જન્મજાત ખોડ છે. જેમાં લગભગ ૨ ઈંચ જેટલું આંતરડું નાના આંતરડાના વધારાના ભાગ તરીકે મોટા આંતરડાથી લગભગ ર ફૂટ દૂર જાવામાં આવે છે. આવી ખોડ ર% જેટલાં લોકોમાં હોય છે. નાના આંતરડાનાં આ ભાગને મેકલ્સ નામના સર્જનનાં નામ પરથી “મેકલ્સ ડાયવર્ટીક્યુલમ” કહે છે.
મેકલ્સ ડાયવર્ટીક્યુલમ ઘણી બધી તકલીફો કરી શકે છે જેવી કે :
૧) ઇન્ફેક્શન થવું : એપેન્ડીસાઇટીસ જેવી બીમારી લાગે.
૨) પરફોરેશન (કાણું પડી જવું) થઈ પેટમાં ઇન્ફેક્શન કરવું.
૩) ચાંદી પડી સખત લોહી મળ માર્ગે જવુંં.
૪) આંતરડામાં બ્લોકેજ કરવું.
૫) ઇન્ટુસસેપ્શન થવું : નાનું આંતરડું મોટા આંતરડામાં જઈ ઇમરજન્સી ઊભી કરે.
નિદાન કઈ રીતે કરવુંઃ
૧) સોનોગ્રાફી અથવા સાદા એક્સ-રેમાં ખબર ન પડે.
૨) સીટી સ્કેનમાં પણ જ્વલ્લે જ ખબર પડે છે.
૩) બ્લીડીંગ થાય ત્યારે ન્યુÂક્લયર સ્ટડીથી ખબર પડે.
૪) લેપ્રોસ્કોપીથી ૧૦૦% નિદાન થાય છે. એપેન્ડીક્સના આૅપરેશન માટે કરવામાં આવતી લેપ્રોસ્કોપી દરમ્યાન આ ખોડનું નિદાન થતું હોય છે.
વારંવાર પેટનો દુઃખાવો અથવા ઉપર બતાવ્યા પ્રમાણે કોમ્પ્લીકેશન થાય તો આૅપરેશનથી જ જિંદગી બચી શકે છે. •
HINDI
मेकल्स डायवर्टीक्युलम
यह आंतों का एक जन्मजात विकार है। इसमें छोटी आंत में लगभग २” अतिरिक्त हिस्सा उभर आता है, जो बड़ी आंत से लगभग २ फीट की दूरी पर होता है। यह विकार २% लोगों में पाया जाता है। छोटी आंत के इस भाग को मेकल्स नामक सर्जन के नाम पर से “मेकल्स डायवर्टीक्युलम” कहा गया है।
मेकल्स डायवर्टीक्युलम के कारण बहुत सी समस्याएं हो सकती है, जैसाकिः-
१) संक्रमण : एपेंडीसाइटीस जैसी बीमारी दिखती है।
२) परफोरेशन (छेद का होना) के कारण पेट में संक्रमण हो सकता है।
३) आंतों में छाला होने के कारण मल मार्ग से रक्त स्त्राव हो सकता है।
४) आंतो में अवरोध पैदा हो सकता है।
५) इंटुससेप्शन होनाः छोटा आंत बड़े आंत में घुस कर आपातस्थिति उत्पन्न करता है।
निदान कैसे करें :
१) सोनोग्राफी अथवा सामान्य एक्स-रे से पता नहीं चलता।
२) सीटी स्केन में भी शायद ही नजर आता है।
३) रक्त स्त्राव होने पर न्युक्लीयर स्टडी से पता चलता है।
४) लेप्रोस्कोपी से १००% निदान होता है।
बार-बार पेट दर्द अथवा उपरोक्त जटीलताएं दिखाई दे तो ऑपरेशन द्वारा ही जान बचाई जा सकती है।•
Mesenteric Lymphadenopathy
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
RECURRENT ABDOMINAL PAIN & MESENTERIC LYMPHADENOPATHY
Recurrent abdominal pain is a common and vexing problem in children especially between 2 and 10 years. Abdominal pain which causes disturbance in sleep, school drop outs and hindrance in day to day activities of the child needs medical attention. It is mandatory to get the child checked up by a doctor and get an ultrasound scan done if necessary.
Ultrasound scan is a common and non invasive investigation which does not have any radiation exposure. It can pick up pathologies that are not visible on the outside or may not be apparent on clinical examination. One of the most common things that is picked up on ultrasound scan is enlarged mesenteric lymph nodes. The most common cause of this is intestinal infections or appendicitis. Rarely they can be due to tuberculosis or malignancy. In a well child, the size of these glands may be monitored by ultrasound scan on a monthly basis. If the size of the glands persist to 1.5 cm or larger and if there are multiple glands in the abdomen, a laparoscopic biopsy of the mesenteric lymph nodes may be helpful to arrive at a scientific diagnosis. ●
GUJARATI
પેટનો દુઃખાવો અને પેટની ગાંઠો
બાળકોમાં (ખાસ કરીને ૨ થી ૧૦ વર્ષની ઉંમરનાં બાળકોમાં) પેટનો દુઃખાવો વારંવાર થવો તે એક સામાન્ય પણ જટિલ પ્રોબ્લેમ છે.
અવારનવાર પેટમાં દુઃખાવો જેનાથી બાળકની ઊંઘ બગડતી હોય, સ્કૂલમાંથી પાછા આવવું પડતું હોય અથવા તેની રોજિંદી પ્રવૃત્તિમાં અડચણ આવે તો તેવા સંજાગોમાં બાળકની ડાક્ટરી તપાસ અનિવાર્ય બને છે. સામાન્ય તપાસમાં ચિન્હો ન જણાતાં લેબોરેટરી તપાસ અને રેડિયોલોજી ટેસ્ટ કરાવવા પડે છે.
સોનોગ્રાફી એક સામાન્ય અને હાનિરહિત તપાસ છે. પેટમાં દુઃખાવાની તપાસ દરમ્યાન આંતરડાની આજુબાજુમાં ગાંઠો હોવાનું નિદાન સોનોગ્રાફીમાં થતું હોય છે. આ થવાનું મુખ્ય કારણ આંતરડાનું ઇન્ફેક્શન અથવા એપેન્ડીક્સનો સોજા છે. ઘણીવાર ટી.બી. અને કેન્સરની શરૂઆત પણ આ ગાંઠોનું કારણ હોય છે. આવા સમયે આ ગાંઠોની સાઈઝ ૧ મહિનાનાં અંતરે બે-ત્રણ સોનોગ્રાફીની તપાસ કરાવી માપવામાં આવે છે. ૧.૫ સેમી. અથવા મોટી સાઈઝની એક થી વધુ ગાંઠો આવે તો લેપ્રોસ્કોપી દ્વારા આૅપરેશન કરી પેટની સંપૂર્ણ તપાસ થાય છે અને એક અથવા વધુ ગાંઠો કાઢી તેની બાયપ્સી દ્વારા સચોટ નિદાન કરાવવું પડે છે. ૯૦% ગાંઠો સામાન્ય ઇન્ફેક્શનના કારણે હોય છે અને તે ચિંતાનું કારણ હોતી નથી. •
HINDI
पेट दर्द एवं पेट में गाँठ
बच्चों में बार-बार पेट दर्द की शिकायत आम है, विशेष रूप से २ से १० वर्ष की आयु के बच्चों में यह समस्या रहती है। पेट दर्द के कारण बच्चे की नींद खराब होना, स्कूल से बार-बार छुट्टी लेना और बच्चे के दैनिक क्रियाकलापों में बाधा होना, इन स्थितियों में डॉक्टर से पामर्श लेना जरूरी है। आवश्यकता पड़ने पर सोनोग्राफी करानी चाहिए।
सोनोग्राफी एक समान्य और हानिरहित जाँच है जिसमें विकिरण का प्रभाव नहीं पड़ता। सोनोग्राफी करने से पेट के भीतर दर्द होने के कारण, आँतों के आसपास गाँठों के होने का पता लगाया जाता है। आँतों का इंफेक्शन या एपेन्डिक्स की सूजन इसका सबसे प्रमुख कारण है, जिसकी पहचान सोनोग्राफी से की जा सकती है। इन गाँठों के होने का कारण टी.बी या कैंसर के होने की शुरूआत भी हो सकती है। ऐसी स्थिति में एक महीने के अंतराल पर दो-तीन सोनोग्राफी से जाँच करके इन गाँठों के आकार को मापा जाता है। १.५ से.मी या उससे बड़ी आकार की एक या अधिक गाँठें होने पर लेप्रोस्कोपी करके पेट की संपूर्ण जाँच की जाती है। इसमें बायोप्सी से गाँठ के अंश को निकाल कर जाँच द्वारा रोग की पक्की पहचान की जाती है। ९०% गाँठें सामान्य इन्फेक्शन के कारण होती है, जो चिंता का विषय नहीं हैं। •
Minimally Invasive Surgery (Key Hole Surgery)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is laparoscopic or keyhole surgery?
Keyhole surgery, or laparoscopic surgery as it is also known, is a method of carrying out an operation without having to make a large incision. Many different types of operations can now be carried out using keyhole surgery. This type of surgery reduces the length of time your child needs to stay in hospital and leaves little scarring.
What are the advantages of keyhole surgery?
Children tend to recover more quickly after keyhole surgery and have fewer side effects. There is little scarring after keyhole surgery which becomes more important as your child grows older and becomes more self-conscious. One side effect of ‘open’ surgery – minimised with keyhole surgery – is ‘adhesions’. This is where internal organs stick together and form bands of scar tissue, which can be painful and cause obstruction. Adhesions have been proven to occur less often in adults after keyhole surgery, and the risk of adhesions in children after keyhole surgery is thought to be less as well.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. After an anaesthetic, children sometimes feel sick and vomit, may have a headache, sore throat or feel dizzy. These effects are short-lived. Any surgery carries a small risk of infection or bleeding.
After the operation, some older children may complain of shoulder pain. Your child may also feel some crackling under the skin because the carbon dioxide sometimes escapes into the tissue just under the skin. These side effects are usually short-lived and do not require any specialized care.
There is always a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision instead.
Are there any alternatives to keyhole surgery?
All operations carried out as keyhole surgery can also be carried out using ‘open’ surgery, that is, with a larger incision.
What does the operation involve?
Your child will be given a general anaesthetic and will be asleep during the operation. Once your child is asleep, the surgeon inserts a small tube called a cannula into your child’s tummy button. A telescope, with a miniature video camera mounted on it, is inserted into this tube to project a very high quality video image onto a television screen. The abdomen is then inflated with carbon dioxide to create space in which the surgeon can operate. The operation is performed by inserting specialized instruments which are passed through small hollow tubes which are inserted through separate very small incisions. There may be two or more small incisions required to perform the operation. Once the operation is over, the surgeon will stitch up the inside of the holes and your child will be taken to the recovery room to wake up from the anaesthetic.
What happens after the operation?
After the operation, your child will return to recover.
Your child may also have a naso-gastric tube, which is a tube passed through the nose into the stomach, so that he or she can be given feeds or medicines easily. Your child may also have an intravenous (into a vein) infusion of fluids as he or she may not feel like eating and drinking after the operation.
You may be able to feel a few lumps under the skin by the wound sites, which are stitches inside the body. This is nothing to worry about and the stitches will dissolve on their own in about three months.
GUJARATI
દૂરબીન વડે પેટનાં ઓપરેશન (લેપ્રોસ્કોપી અને થોરેકોસ્કોપી)
લેપ્રોસ્કોપી:
“લેપ્રોસ્કોપી” એટલે પેટ પર નાના છિદ્રો દ્વારા દૂરબીન અને સાધનો મુકી પેટનાં વિવિધ આૅપરેશન કરવા. બાળકોમાં અને નવજાત શિશુઓમાં આ ટેકનિકથી ફ્ક્ત ૩ મીમી અથવા ૫ મી.મી.નાં નાના કાણાથી આૅપરેશન કરવામાં આવે છે. આધુનિક કેમેરા અને લાઈટની મદદથી ટી.વીમાં મોટી ઈમેજ જાઇ આવા આૅપરેશન ખૂબ જ સારી અને ચોક્કસાઇ પૂર્વક થાય છે.
લેપ્રોસ્કોપીની ટેકનિક શીખવા માટે બાળકોનાં સર્જનએ ચોક્કસ પ્રકારની ટ્રેનિંગ લેવી પડે છે અને તેના માટે સ્પેશ્યલ સાધનોની જરૂર પડે છે.
નવજાત બાળકો અને મોટા બાળકોમાં લેપ્રોસ્કોપીના મુખ્ય આૅપરેશન આ પ્રમાણે છેઃ
– એપેન્ડીક્સ
– ઇન્દ્રની ગોળી પેટમાં હોય (અનડીસેન્ડેડ ટેસ્ટીસ)
– પેટમાં ગાંઠ હોવી.
– અંડાશય(ઓવરી)માં ગાંઠ
– લીવરની ગાંઠ
– મેકલ્સ ડાયવરટીક્યુલમ
– કિડની નળીનાં આૅપરેશન
– ઉદરપટલનાં હર્નીયા
– સારણ ગાંઠ
આ સિવાય બીજા અનેક આૅપરેશન લેપ્રોસ્કોપી દ્વારા બાળકોમાં થાય છે. લેપ્રોસ્કોપીના આૅપરેશનથી બાળકને દુઃખાવો ખૂબ જ ઓછો થાય છે. લોહીની જરૂર નથી પડતી અને પેટ પર ગંદા કાપા નથી પડતાં. બાળક નું હાÂસ્પટલમાં થતું રોકાણ પણ ઓછું થઈ જાય છે.
આધુનિક મેડિકલ સાયન્સ અને ટેžનોલોજીની આ એક અદ્ભૂત શોધ છે. •
થોરેકોસ્કોપી:
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો (ડુપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
दूरबीन से पेट की सर्जरी (लेप्रोस्कोपी और थोरेकोस्कोपी )
लेप्रोस्कोपी:
‘लेप्रोस्कोपी’ सर्जरी की एक पद्धति है, जिसमें कोई बड़ा चीरा किये बिना पेट में छोटे छेद करके दूरबीन और अन्य उपकरणों द्वारा पेट के विभिन्न प्रकार के ऑपरेशन किये जाते हैं। इस तकनीक में नवजात शिशु और बड़े बच्चों के ऑपरेशन मात्र ३ और ५ मिलीमीटर के छेद करके किया जाता है।
इस प्रक्रिया में बच्चें को बेहोश करने के बाद बाल सर्जन बच्चे के पेट में छेद करके एक छोटी ट्यूब डालते हैं, जिसपर एक आधुनिक कैमरा और लाइट लगी हुई होती है, जिसकी मदद से टी.वी में बड़ी इमेज दिखाई देती है और बड़ी ही सावधानीपर्वूक ऑपरेशन किया जाता है। इस सर्जरी में दो या अधिक छोटे छेद करके ऑपरेशन किया जाता है। इस तकनीक के लिए बाल सर्जन को विशेष प्रकार की ट्रेनिंग लेनी पड़ती है और इसमें विशेष उपकरणों का इस्तेमाल करने की आवश्यकता है।
नवजात बच्चों और बड़े बच्चों में लेप्रोस्कोपी ऑपरेशन मुख्य रूप से नीचे दिये गये रोगों के लिए किया जाता हैः
१. ऐपेन्डिक्स
२. अनडीसेन्डेड टेस्टीस
३. पेट के अंदर गांठ होने के कारण
४. अंडाशय में गांठ, लीवर में गांठ
५. मेकल्स डायवरटीक्युलम
थोरेकोस्कोपी:
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३ मिलीमीटरऔर ५ मिलीमीटर के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (एंपियेमा)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की श्वसनीजन्य पुटी [Bronchogenic Cyst] और जलस्फोट पुटी [ Hydatid Cyst])
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Minimally Invasive Surgery / Key Hole Surgery
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is keyhole surgery or Minimally Invasive Surgery ?
Keyhole surgery, or laparoscopic surgery as it is also known, is a method of carrying out an operation without having to make a large incision. Many different types of operations can now be carried out using keyhole surgery. This type of surgery reduces the length of time your child needs to stay in hospital and leaves little scarring.
What are the advantages of keyhole surgery?
Children tend to recover more quickly after keyhole surgery and have fewer side effects. There is little scarring after keyhole surgery which becomes more important as your child grows older and becomes more self-conscious. One side effect of ‘open’ surgery – minimised with keyhole surgery – is ‘adhesions’. This is where internal organs stick together and form bands of scar tissue, which can be painful and cause obstruction. Adhesions have been proven to occur less often in adults after keyhole surgery, and the risk of adhesions in children after keyhole surgery is thought to be less as well.
Are there any risks?
Every anaesthetic carries a risk of complications but this is very small. Your child’s anaesthetist is an experienced doctor who is trained to deal with any complications. After an anaesthetic, children sometimes feel sick and vomit, may have a headache, sore throat or feel dizzy. These effects are short-lived. Any surgery carries a small risk of infection or bleeding.
After the operation, some older children may complain of shoulder pain. Your child may also feel some crackling under the skin because the carbon dioxide sometimes escapes into the tissue just under the skin. These side effects are usually short-lived and do not require any specialized care.
There is always a chance that keyhole surgery will not be possible for your child. Sometimes the surgeon will not be able to carry out an operation using the keyhole method for technical reasons or because of unexpected findings. If this is the case, the surgeon will carry out the operation using a larger incision instead.
Are there any alternatives to keyhole surgery?
All operations carried out as keyhole surgery can also be carried out using ‘open’ surgery, that is, with a larger incision.
What does the operation involve?
Your child will be given a general anaesthetic and will be asleep during the operation. Once your child is asleep, the surgeon inserts a small tube called a cannula into your child’s tummy button. A telescope, with a miniature video camera mounted on it, is inserted into this tube to project a very high quality video image onto a television screen. The abdomen is then inflated with carbon dioxide to create space in which the surgeon can operate. The operation is performed by inserting specialized instruments which are passed through small hollow tubes which are inserted through separate very small incisions. There may be two or more small incisions required to perform the operation. Once the operation is over, the surgeon will stitch up the inside of the holes and your child will be taken to the recovery room to wake up from the anaesthetic.
What happens after the operation?
After the operation, your child will return to recover.
Your child may also have a naso-gastric tube, which is a tube passed through the nose into the stomach, so that he or she can be given feeds or medicines easily. Your child may also have an intravenous (into a vein) infusion of fluids as he or she may not feel like eating and drinking after the operation.
You may be able to feel a few lumps under the skin by the wound sites, which are stitches inside the body. This is nothing to worry about and the stitches will dissolve on their own in about three months.
GUJARATI
દૂરબીન વડે પેટનાં ઓપરેશન (લેપ્રોસ્કોપી અને થોરેકોસ્કોપી)
લેપ્રોસ્કોપી:
“લેપ્રોસ્કોપી” એટલે પેટ પર નાના છિદ્રો દ્વારા દૂરબીન અને સાધનો મુકી પેટનાં વિવિધ આૅપરેશન કરવા. બાળકોમાં અને નવજાત શિશુઓમાં આ ટેકનિકથી ફ્ક્ત ૩ મીમી અથવા ૫ મી.મી.નાં નાના કાણાથી આૅપરેશન કરવામાં આવે છે. આધુનિક કેમેરા અને લાઈટની મદદથી ટી.વીમાં મોટી ઈમેજ જાઇ આવા આૅપરેશન ખૂબ જ સારી અને ચોક્કસાઇ પૂર્વક થાય છે.
લેપ્રોસ્કોપીની ટેકનિક શીખવા માટે બાળકોનાં સર્જનએ ચોક્કસ પ્રકારની ટ્રેનિંગ લેવી પડે છે અને તેના માટે સ્પેશ્યલ સાધનોની જરૂર પડે છે.
નવજાત બાળકો અને મોટા બાળકોમાં લેપ્રોસ્કોપીના મુખ્ય આૅપરેશન આ પ્રમાણે છેઃ
– એપેન્ડીક્સ
– ઇન્દ્રની ગોળી પેટમાં હોય (અનડીસેન્ડેડ ટેસ્ટીસ)
– પેટમાં ગાંઠ હોવી.
– અંડાશય(ઓવરી)માં ગાંઠ
– લીવરની ગાંઠ
– મેકલ્સ ડાયવરટીક્યુલમ
– કિડની નળીનાં આૅપરેશન
– ઉદરપટલનાં હર્નીયા
– સારણ ગાંઠ
આ સિવાય બીજા અનેક આૅપરેશન લેપ્રોસ્કોપી દ્વારા બાળકોમાં થાય છે. લેપ્રોસ્કોપીના આૅપરેશનથી બાળકને દુઃખાવો ખૂબ જ ઓછો થાય છે. લોહીની જરૂર નથી પડતી અને પેટ પર ગંદા કાપા નથી પડતાં. બાળક નું હાÂસ્પટલમાં થતું રોકાણ પણ ઓછું થઈ જાય છે.
આધુનિક મેડિકલ સાયન્સ અને ટેžનોલોજીની આ એક અદ્ભૂત શોધ છે. •
થોરેકોસ્કોપી:
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો (ડુપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
दूरबीन से पेट की सर्जरी (लेप्रोस्कोपी और थोरेकोस्कोपी )
लेप्रोस्कोपी:
‘लेप्रोस्कोपी’ सर्जरी की एक पद्धति है, जिसमें कोई बड़ा चीरा किये बिना पेट में छोटे छेद करके दूरबीन और अन्य उपकरणों द्वारा पेट के विभिन्न प्रकार के ऑपरेशन किये जाते हैं। इस तकनीक में नवजात शिशु और बड़े बच्चों के ऑपरेशन मात्र ३ और ५ मिलीमीटर के छेद करके किया जाता है।
इस प्रक्रिया में बच्चें को बेहोश करने के बाद बाल सर्जन बच्चे के पेट में छेद करके एक छोटी ट्यूब डालते हैं, जिसपर एक आधुनिक कैमरा और लाइट लगी हुई होती है, जिसकी मदद से टी.वी में बड़ी इमेज दिखाई देती है और बड़ी ही सावधानीपर्वूक ऑपरेशन किया जाता है। इस सर्जरी में दो या अधिक छोटे छेद करके ऑपरेशन किया जाता है। इस तकनीक के लिए बाल सर्जन को विशेष प्रकार की ट्रेनिंग लेनी पड़ती है और इसमें विशेष उपकरणों का इस्तेमाल करने की आवश्यकता है।
नवजात बच्चों और बड़े बच्चों में लेप्रोस्कोपी ऑपरेशन मुख्य रूप से नीचे दिये गये रोगों के लिए किया जाता हैः
१. ऐपेन्डिक्स
२. अनडीसेन्डेड टेस्टीस
३. पेट के अंदर गांठ होने के कारण
४. अंडाशय में गांठ, लीवर में गांठ
५. मेकल्स डायवरटीक्युलम
थोरेकोस्कोपी:
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३ मिलीमीटरऔर ५ मिलीमीटर के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (एंपियेमा)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की श्वसनीजन्य पुटी [Bronchogenic Cyst] और जलस्फोट पुटी [ Hydatid Cyst])
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Nephrectomy
What is a nephrectomy?
A nephrectomy is an operation to remove a kidney. The child generally needs to stay in hospital for up to 2-3 days.
Why does my child need to have this operation?
Your child will need this operation because a kidney is not working properly. This could cause infections which may damage the other kidney, and makes it more likely that your child will have high blood pressure at some point in their life. Being left with one kidney should not cause your child any problems.
What does the operation involve?
The surgeon will remove your child’s damaged kidney through a cut (incision) in his or her side. The operation takes between one to one-and-a-half hours.
Nowadays, this operation can also be done with the help of laparoscopy of minimally invasive surgery. This involves three small 5 mm holes on the side of the child and the kidney is removed without any cuts. When done laparoscopically, the hospital stay and pain in reduced.
Kidney with pus (Pyonephrosis)

Multicystic Dysplastic Kidney

Obstructed Nonfunctioning Duplex kidney


Kidney removed by Laparoscopy

Post operative scars after Laparoscopic Nephrectomy
What happens after the operation?
Your child will be brought back to the ward to recover. He or she will be able to eat and drink soon after the operation.
Your child may have a tube (catheter) coming out of the bladder to drain away urine. This is usually removed two days after the operation and then you will be able to go home. Sutures are dissolvable and so you do not need to have them removed.
What are the risks of a nephrectomy?
All surgery carries a small risk of bleeding during or after the operation. After an anaesthetic some children may feel sick and vomit. They may have a headache, sore throat or feel dizzy. These side effects are usually short-lived and not severe.
Usually, there is only a small amount of bleeding, but occasionally a child may need to be given extra blood in the form of a transfusion.
When you get home
You should encourage, but not force, your child to drink.
The child may required pain relief medications if he has pain. The doctor will ask you to come for follow up examination a week after surgery.
Nose Bleed (Epistaxis)
Nose bleeds are when the small fragile blood vessels in the nose break. This will cause the nose to bleed. It is a common condition, especially in young children. Children who have frequent nosebleeds should be checked for underlying conditions by a doctor.
What causes nose bleeds?
Nosebleeds are pretty common, especially in young children. This is because the blood vessels in the nasal lining are close to the surface and quite fragile. They can rupture easily.
A bump or bang on the nose can often result in a nosebleed. Young children often play very physical games, whether it’s rushing around on the playground at nursery or school or tumbling about at home. Bumps on the nose can be pretty common.
If a child picks their nose or blows it too vigorously, this can also start a nosebleed.
Sometimes even a violent sneeze can damage the nasal blood vessels, and trigger a nose bleed.
While nosebleeds are rarely dangerous, very occasionally, a nosebleed can indicate a more serious underlying problem like a head injury.
What are the signs and symptoms of nose bleeds?
If a child has a nosebleed after suffering from a bump on the head, it’s important to look carefully for other signs that might indicate an underlying injury.
If the child has any of the following symptoms emergency medical advice should be sought:
• confusion
• drowsiness
• nausea and vomiting
• losing fluid through their nose that is thin and watery
How are nose bleeds treated?
If a child has a nose bleed, the recommended course of action is:
• Ask the child to sit down with their head tilted forward.
• Get them to breathe through their mouth.
• Put a bowl under the nose and give them tissues or a cloth.
• Ask them to pinch the front, soft part of their nose for 10 minutes – or pinch it for them if it is a young child.
• If tolerated, apply an ice pack to the affected area
• After 10 minutes, release the pressure – if the bleeding has not stopped, reapply the pressure for up to two further periods of 10 minutes.
• Once the bleeding stops gently clean the area.
Do not tilt the child’s head backwards. This will not stop the bleeding and can cause blood to trickle down their throat. This can make them vomit or choke and affect their ability to breathe.
When to ask for medical help about nose bleeds ?
If the bleeding does not stop after 30 minutes, it’s best to take the child down to your local hospital or seek medical advise.
Frequent nosebleeds
Some children do seem more prone than others to frequent nosebleeds. If a child does seem to suffer from them more than twice a week, it’s advisable to see a doctor.
It’s important in the first instance to rule out an underlying bleeding disorder.The doctor may recommend blood tests.
Another more common explanation for frequent nosebleeds is that the child may have picked their nose causing blood vessels in the septum, the cartilage which divides the nostrils, to bleed.
The doctor can also check for any signs of infection. If there is any infection, the doctor will probably prescribe a course of ointment with antibiotic and anti-inflammatory properties.
A child who has a deviated septum is more likely to suffer from nosebleeds. A deviated septum means that the septum is slightly bent, usually as a result of injury (for instance a sports injury or an injury sustained during birth). The deviated septum causes abnormal airflow through the nose which causes the lining of the septum to dry out and bleed easily.
What happens next?
Most children, even those who suffer from frequent nosebleeds, tend to outgrow it. Nosebleeds can also happen in adult life but it is less common.
Neck Glands
INFORMATION ALSO AVAILABLE IN ENGLISH, GUJARATI AND HINDI
There are two types of swellings in the neck:
Congenital Swellings (Since Birth):
a) Tyroglossal Cyst: This swelling occurs in the midline of the neck and is due to a developmental defect during the formation of the thyroid gland. Surgery is a must for this swelling.
 Thyroglossal Cyst
Thyroglossal Cyst
b) Dermoid Cyst: This swelling also happens in the midline of the neck. They are also seen at many other sites in the body. Surgery is also required for these swellings.
 Dermoid Cyst
Dermoid Cyst
c) Cystic Hygroma: These swellings occur as a result of a developmental anomaly of the lymphatics. They look like cysts filled with water and are commonly seen in any part of the neck. They can vary from being very small to massive in size. Surgery is curative for these swellings.
 Cystic Hygroma in the neck
Cystic Hygroma in the neck
d) Branchial cyst: These swellings are found on the side of the neck. They are sometimes also seen like a small punctum which is called a Branchial Sinus
 Branchial Cyst in the neck
Branchial Cyst in the neck
e) Cervical Meningocele: These swellings are seen behind the neck in the midline. They are present since birth and surgery is curative.
 Cervical Meningomyelocele
Cervical Meningomyelocele
Acquired Swellings (After Birth) :
a) Lymph nodes: They can be single or multiple. They may be seen over different sites in the neck. Common cause of lymph node enlargement is secondary to an infective process in the head and neck region.


b) Tuberculous nodes (Koch’s nodes): Tuberculous nodes are not uncommon. A confirmed diagnosis can be acheived by biopsy of the node. Regular medications can almost always cure this problem.

c) Malignant nodes (Cancers): The most commonly seen malignant nodes in the neck in children are lymphomas. Confirmation of diagnosis can be done by biopsy of the nodes. Regular chemotherapy can be curative in most of these cases.
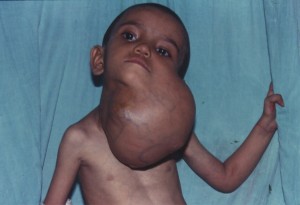
Lymph Glands in the Neck:
Everyone has lymph glands. They are in many areas of the body, including the neck, under the arms and in the groin (at the top of each leg). There are also lymph glands in the abdomen, chest and pelvis. Lymph glands are also known as lymph nodes.
Lymph glands become enlarged when the body is fighting an infection, such as a cold. Enlarged lymph glands are particularly common in children as their body takes time to build up immunity to infection.
What causes swollen lymph glands?
Lymph glands swell as part of the body’s response to infection.
Lymph glands are connected by vessels with branches right through the body, similar to the blood circulation system. Rather than carrying blood, these vessels carry a clear liquid called lymph, which contains a high number of white blood cells.
Together with other organs (the spleen, tonsils, adenoids and thymus gland), they form what’s known as the lymphatic system. It has several functions but one of its key roles is fighting infection.
When the body is fighting an infection, the number of white blood cells multiplies rapidly. Some of these cells will go to the lymph gland nearest the infection, which produces enlargement of the lymph glands.
Children often have infections as it takes time for them to build immunity to the viruses and bacteria in the environment. Children who have recently started playgroup or nursery are especially prone because they are coming into contact with a large group of children of the first time.
What are the signs and symptoms of enlarged lymph glands?
The lymph glands will appear swollen. They will also be uncomfortable.
Children frequently get upper respiratory tract infections, such as an ear or throat infection. This means that swollen glands in the neck are particularly common.
How are enlarged lymph glands normally diagnosed?
A child’s doctor will feel their glands to check if they are swollen.
How are enlarged lymph glands treated?
Most cases of enlarged lymph glands are from infection. Once the infection is gone, the glands will get smaller and less tender over time.
If the glands are particularly large, the doctor will check the child for any other symptoms or an underlying cause.
What happens next?
In most cases, enlarged lymph glands are not serious and the condition is common. Following an infection, it is normal for them to take some time for the swelling to go down.
Enlarged lymph glands rarely indicate a more serious problem. Sometimes it is a sign of cancer, such as lymphoma, but this is rare.
GUJARATI
ગળામાં થતી ગાંઠો
ગળામાં થતી ગાંઠો બે પ્રકારની હોય છેઃ
૧. જન્મ જાત ગાંઠઃ
૧) થાઇરોગ્લોસલ સીસ્ટ : ગળાનાં મધ્ય ભાગમાં થતી ગાંઠ થાયરોઇડ ગ્રંથિની ડેવલપમેન્ટની ક્ષતિના કારણે થાય છે. આૅપરેશન કરવાથી જ મટે છે.
૨) ડરમોઈડ સીસ્ટ : આ પણ ગળાનાં મધ્યભાગમાં થતી ગાંઠ છે. જે ઓપરેશનથી મટે છે.
૩) સીસ્ટીક હાઇગ્રોમા : લીમ્ફેટીક નળીઓની બનાવટની ખામીના કારણે, પાણી ભરેલી ગાંઠ ગળામાં ગમે તે જગ્યાએ થાય છે. આવી ગાંઠ સાઈઝમાં નાની અથવા આત્યંત મોટી હોય છે. યોગ્ય સમયે ઓપરેશન કરાવવું જરૂરી છે.
૪) બ્રેન્કયલ સીસ્ટ : આ ગાંઠ ગળાની સાઈડમાં જાવા મળતી હોય છે. ધણીવાર તે નાના છિદ્રનાં રૂપમાં હોય છે. (જેને સાઇનસ કહે છે.)
૫) સરવાઇકલ મેનીન્ગોમાઇલોસીલ : ગળાની પાછળ બરાબર કરોડના મણકા પર થતી જન્મજાત ગાંઠ છે અને આૅપરેશન કરવાથી સંપૂર્ણ સા૨ું થઈ જાય છે.
૨. જન્મ પછી થતી ગળાની ગાંઠો :
૧) લીમ્ફનોડની ગાંઠ : આ ગાંઠ ગળામાં જાવા મળે છે અને તે એક કરતા વધુની સંખ્યામાં અને જુદી જુદી જગ્યાએ પણ હોય છે.
લીમ્ફગ્લેન્ડ – માથા, નાક, કાન, ગળામાં થતા ઇન્ફેક્શનની વેડ ઘાલવાથી થાય છે અને બરાબર દવા કરવાથી મટે છે.
૨) ટી.બી.ની ગાંઠ : ગળામાં ટી.બી.ની ગાંઠ ૧/૨ણી સામાન્ય બીમારી છે. ચોક્કસ નિદાન બાયોપ્સી દ્બા૨ા કરાવી યોગ્ય દવાઓ આપવાથી મટી જાય છે.
૩) કેન્સરની ગાંઠ : બાળકોમાં ગળામાં લીમ્ફોમા નામના કેન્સરને લીધે ગાંઠ થતી હોય છે. તેનું જરૂરી નિદાન બાયોપ્સી વડે કરાવી, દવાઓથી મટાડી શકાય છે. •
HINDI
गले की गांठे
१. जन्मजात गांठ
१) थाइरोग्लोसल सीस्टः गले के मध्य भाग में होनेवाली यह गांठ थाइरोइड ग्ा्रंथी के दोषपूर्ण विकास के कारण होती है और यह केवल ऑपरेशन के द्वारा ही ठीक की जा सकती है।
२) डरमोइड सीस्टः यह भी गले के मध्य भाग में होनेवाली एक गांठ है जो ऑपरेशन के द्वारा ही ठीक की जा सकती है।
३) सीस्टिक हाइग्ा्रोमाः लीम्फेटिक नलिकाओं की बनावट में दोष के कारण, पानी भरी एक गांठ गले के भीतर कहीं भी हो सकती है। यह गांठ आकार में या तो अत्यंत छोटी होती है या अत्यंत बड़ी होती है। उचित समय पर इसका ऑपरेशन कराना आवश्यक है।
४) ब्रेंकीयल सीस्टः यह गले के एक ओर दिखाई देनेबाली गांठ है। कई बार यह एक छोटे से छेद के रूप में होती है (जिसे साइनस कहते हैं)।
५) सरवाइकल मेनींगोमाइलोसीलः गरदन के पिछले हिस्से में ठीक रीढ़ पर होनेवाली जन्मजात गांठ होती है और ऑपरेशन के द्वारा पूर्णरूप से ठीक हो जाती है।
२. जन्म के बाद होनेवाली गले की गांठ
१) लीम्फनोड की गांठः इस प्रकार की गांठ गले के एक ओर देखी जा सकती है।
२) टी.बी. की गांठः गले में टी.बी. की गांठ होना एक सामान्य बीमारी है। सही निदान, बायोप्सी के उपरांत उचित दवाइयों से ठीक हो जाती है।
३) कैंसर की गांठः यह बच्चों के गले में लीम्फोमा नामक कैंसर के कारण होनेवाली गांठ है। इसे आवश्यक निदान, बायोप्सी तथा उचित दवाइयों से ठीक किया जा सकता है।•
Neck Swellings (Swellings in Neck)
INFORMATION ALSO AVAILABLE IN ENGLISH, GUJARATI AND HINDI
There are two types of swellings in the neck:
Congenital Swellings (Since Birth):
a) Tyroglossal Cyst: This swelling occurs in the midline of the neck and is due to a developmental defect during the formation of the thyroid gland. Surgery is a must for this swelling.
 Thyroglossal Cyst
Thyroglossal Cyst
b) Dermoid Cyst: This swelling also happens in the midline of the neck. They are also seen at many other sites in the body. Surgery is also required for these swellings.
 Dermoid Cyst
Dermoid Cyst
c) Cystic Hygroma: These swellings occur as a result of a developmental anomaly of the lymphatics. They look like cysts filled with water and are commonly seen in any part of the neck. They can vary from being very small to massive in size. Surgery is curative for these swellings.
 Cystic Hygroma in the neck
Cystic Hygroma in the neck
d) Branchial cyst: These swellings are found on the side of the neck. They are sometimes also seen like a small punctum which is called a Branchial Sinus
 Branchial Cyst in the neck
Branchial Cyst in the neck
e) Cervical Meningocele: These swellings are seen behind the neck in the midline. They are present since birth and surgery is curative.
 Cervical Meningomyelocele
Cervical Meningomyelocele
Acquired Swellings (After Birth) :
a) Lymph nodes: They can be single or multiple. They may be seen over different sites in the neck. Common cause of lymph node enlargement is secondary to an infective process in the head and neck region.


b) Tuberculous nodes (Koch’s nodes): Tuberculous nodes are not uncommon. A confirmed diagnosis can be acheived by biopsy of the node. Regular medications can almost always cure this problem.

c) Malignant nodes (Cancers): The most commonly seen malignant nodes in the neck in children are lymphomas. Confirmation of diagnosis can be done by biopsy of the nodes. Regular chemotherapy can be curative in most of these cases.
Lymph Glands in the Neck:
Everyone has lymph glands. They are in many areas of the body, including the neck, under the arms and in the groin (at the top of each leg). There are also lymph glands in the abdomen, chest and pelvis. Lymph glands are also known as lymph nodes.
Lymph glands become enlarged when the body is fighting an infection, such as a cold. Enlarged lymph glands are particularly common in children as their body takes time to build up immunity to infection.
What causes swollen lymph glands?
Lymph glands swell as part of the body’s response to infection.
Lymph glands are connected by vessels with branches right through the body, similar to the blood circulation system. Rather than carrying blood, these vessels carry a clear liquid called lymph, which contains a high number of white blood cells.
Together with other organs (the spleen, tonsils, adenoids and thymus gland), they form what’s known as the lymphatic system. It has several functions but one of its key roles is fighting infection.
When the body is fighting an infection, the number of white blood cells multiplies rapidly. Some of these cells will go to the lymph gland nearest the infection, which produces enlargement of the lymph glands.
Children often have infections as it takes time for them to build immunity to the viruses and bacteria in the environment. Children who have recently started playgroup or nursery are especially prone because they are coming into contact with a large group of children of the first time.
What are the signs and symptoms of enlarged lymph glands?
The lymph glands will appear swollen. They will also be uncomfortable.
Children frequently get upper respiratory tract infections, such as an ear or throat infection. This means that swollen glands in the neck are particularly common.
How are enlarged lymph glands normally diagnosed?
A child’s doctor will feel their glands to check if they are swollen.
How are enlarged lymph glands treated?
Most cases of enlarged lymph glands are from infection. Once the infection is gone, the glands will get smaller and less tender over time.
If the glands are particularly large, the doctor will check the child for any other symptoms or an underlying cause.
What happens next?
In most cases, enlarged lymph glands are not serious and the condition is common. Following an infection, it is normal for them to take some time for the swelling to go down.
Enlarged lymph glands rarely indicate a more serious problem. Sometimes it is a sign of cancer, such as lymphoma, but this is rare.
GUJARATI
ગળામાં થતી ગાંઠો
ગળામાં થતી ગાંઠો બે પ્રકારની હોય છેઃ
૧. જન્મ જાત ગાંઠઃ
૧) થાઇરોગ્લોસલ સીસ્ટ : ગળાનાં મધ્ય ભાગમાં થતી ગાંઠ થાયરોઇડ ગ્રંથિની ડેવલપમેન્ટની ક્ષતિના કારણે થાય છે. આૅપરેશન કરવાથી જ મટે છે.
૨) ડરમોઈડ સીસ્ટ : આ પણ ગળાનાં મધ્યભાગમાં થતી ગાંઠ છે. જે ઓપરેશનથી મટે છે.
૩) સીસ્ટીક હાઇગ્રોમા : લીમ્ફેટીક નળીઓની બનાવટની ખામીના કારણે, પાણી ભરેલી ગાંઠ ગળામાં ગમે તે જગ્યાએ થાય છે. આવી ગાંઠ સાઈઝમાં નાની અથવા આત્યંત મોટી હોય છે. યોગ્ય સમયે ઓપરેશન કરાવવું જરૂરી છે.
૪) બ્રેન્કયલ સીસ્ટ : આ ગાંઠ ગળાની સાઈડમાં જાવા મળતી હોય છે. ધણીવાર તે નાના છિદ્રનાં રૂપમાં હોય છે. (જેને સાઇનસ કહે છે.)
૫) સરવાઇકલ મેનીન્ગોમાઇલોસીલ : ગળાની પાછળ બરાબર કરોડના મણકા પર થતી જન્મજાત ગાંઠ છે અને આૅપરેશન કરવાથી સંપૂર્ણ સા૨ું થઈ જાય છે.
૨. જન્મ પછી થતી ગળાની ગાંઠો :
૧) લીમ્ફનોડની ગાંઠ : આ ગાંઠ ગળામાં જાવા મળે છે અને તે એક કરતા વધુની સંખ્યામાં અને જુદી જુદી જગ્યાએ પણ હોય છે.
લીમ્ફગ્લેન્ડ – માથા, નાક, કાન, ગળામાં થતા ઇન્ફેક્શનની વેડ ઘાલવાથી થાય છે અને બરાબર દવા કરવાથી મટે છે.
૨) ટી.બી.ની ગાંઠ : ગળામાં ટી.બી.ની ગાંઠ ૧/૨ણી સામાન્ય બીમારી છે. ચોક્કસ નિદાન બાયોપ્સી દ્બા૨ા કરાવી યોગ્ય દવાઓ આપવાથી મટી જાય છે.
૩) કેન્સરની ગાંઠ : બાળકોમાં ગળામાં લીમ્ફોમા નામના કેન્સરને લીધે ગાંઠ થતી હોય છે. તેનું જરૂરી નિદાન બાયોપ્સી વડે કરાવી, દવાઓથી મટાડી શકાય છે. •
HINDI
गले की गांठे
१. जन्मजात गांठ
१) थाइरोग्लोसल सीस्टः गले के मध्य भाग में होनेवाली यह गांठ थाइरोइड ग्ा्रंथी के दोषपूर्ण विकास के कारण होती है और यह केवल ऑपरेशन के द्वारा ही ठीक की जा सकती है।
२) डरमोइड सीस्टः यह भी गले के मध्य भाग में होनेवाली एक गांठ है जो ऑपरेशन के द्वारा ही ठीक की जा सकती है।
३) सीस्टिक हाइग्ा्रोमाः लीम्फेटिक नलिकाओं की बनावट में दोष के कारण, पानी भरी एक गांठ गले के भीतर कहीं भी हो सकती है। यह गांठ आकार में या तो अत्यंत छोटी होती है या अत्यंत बड़ी होती है। उचित समय पर इसका ऑपरेशन कराना आवश्यक है।
४) ब्रेंकीयल सीस्टः यह गले के एक ओर दिखाई देनेबाली गांठ है। कई बार यह एक छोटे से छेद के रूप में होती है (जिसे साइनस कहते हैं)।
५) सरवाइकल मेनींगोमाइलोसीलः गरदन के पिछले हिस्से में ठीक रीढ़ पर होनेवाली जन्मजात गांठ होती है और ऑपरेशन के द्वारा पूर्णरूप से ठीक हो जाती है।
२. जन्म के बाद होनेवाली गले की गांठ
१) लीम्फनोड की गांठः इस प्रकार की गांठ गले के एक ओर देखी जा सकती है।
२) टी.बी. की गांठः गले में टी.बी. की गांठ होना एक सामान्य बीमारी है। सही निदान, बायोप्सी के उपरांत उचित दवाइयों से ठीक हो जाती है।
३) कैंसर की गांठः यह बच्चों के गले में लीम्फोमा नामक कैंसर के कारण होनेवाली गांठ है। इसे आवश्यक निदान, बायोप्सी तथा उचित दवाइयों से ठीक किया जा सकता है।•
Neural tube defects
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What is spinal dysraphism?
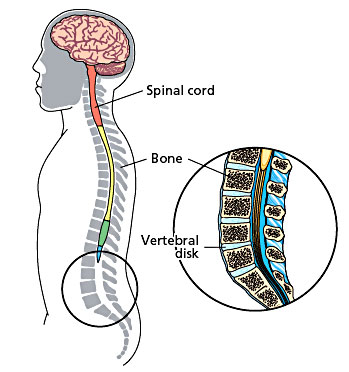
In early development, the brain and spinal cord start as a tube-like structure called the ‘neural tube’ that is open at either end. These openings close within the first weeks of pregnancy, and the neural tube continues to grow and fold, eventually forming the brain and spinal cord.
If the tube fails to close properly, this results in a group of problems called ‘neural tube defects’. Spinal dysphraism is the term used to describe what happens when the spinal column (backbone) fails to form properly. This happens very early in pregnancy, before the end of the fourth week. There are two types of spinal dysphraism: open, also called spina bifida aperta or myelomeningocele, or closed, also called spina bifida occulta.
The open myelomeningocele type accounts for 75 per cent of all cases of spina bifida. In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
Open Neural Tube Defects
In closed spinal dysphraism, the spinal cord (a tube-like structure containing nerves) and its coverings do not protrude through the back unlike in the open type. On its own, closed spinal dysphraism is unlikely to cause any problems, and many people have the condition without ever knowing it. However, it can be associated with other conditions that could lead to problems with movement and bladder control.
Closed Neural Tube Defect
Many children have a ‘tethered cord’, which is the term used when the lower end of the spinal cord is attached to the lower bones of the spinal column rather than hanging freely as it should. Normally the spinal column grows more quickly than the spinal cord, so that by the time the baby is born, the spinal cord has moved higher up the spinal column. If the cord is tethered, the spinal cord and nerves are stretched, reducing their ability to carry messages to and from the brain and causing pain. Growth spurts can stretch the spinal cord and nerves, causing problems with leg movement and bladder and bowel control.
What are the symptoms of closed spinal dysphraism?
In many people, there may be no symptoms at all. However, a birthmark, hairy patch or dermal sinus in the lower back area may lead doctors to suspect that a child has closed spinal dysphraism. Other children may develop repeated bouts of meningitis for which no cause can be found or may have problems keeping dry (urinary incontinence) that cannot be explained. If it not diagnosed until early childhood, the first sign might be weakness or unevenness of the legs or talipes (clubfeet) affecting one of both limbs. Back or leg pain might be a problem too. If these symptoms are due to a tethered cord they may get worse as the child grows. Treatment by surgery tends to be suggested only when a child shows signs that his or her condition is getting worse, for instance, movement becomes more problematic or urinary incontinence is making everyday life more difficult or painful.
How is closed spinal dysphraism diagnosed?
Initial suspicions may be raised through clinical examination but imaging scans are used to confirm the extent of the problem. Ultrasound or magnetic resonance imaging scans are the usual methods used.
How is closed spinal dysphraism treated?
If there are clinical symptoms that are getting worse, these may be reduced using surgery to release the tethered cord. This relieves pressure on the spinal cord and nerves and can improve leg symptoms in many cases. It is less successful in improving bladder and bowel problems but usually stops them getting any worse over time.
What does the operation involve?
At surgery, the surgeon will release the spinal cord from where it is tethered so that it can move as the child grows. If possible, the surgeon will reduce the size of a lipoma to relieve pressure on the spinal cord. After the operation, the incision on your child’s back will be closed and covered with a dressing.
Are there any risks?
The operation to detach a tethered cord is very specialized due to the complex arrangements of nerves in the area. There is always a risk that the nerves, or the spinal cord itself, could be damaged in the operation but if the surgeon believes that this may happen, he or she will stop the procedure.
The aim of the operation is to stop your child’s symptoms from them getting any worse. There is no guarantee that this operation will remove your child’s symptoms or even improve them. This operation tends to improve leg symptoms more frequently than bladder and bowel symptoms.
What is the outlook for children with closed spinal dysphraism?
Orthopaedic problems
In some cases, children may have developed leg and foot problems as a result of the closed spinal dysphraism. These can include clawing of the toes or very high arches, which in turn can lead to tightening of the Achilles tendon at the heel. This can affect one leg or both and if it is severe, we may refer your child to an orthopaedic surgeon for further treatment.
Where a child has scoliosis as a result of the closed spinal dysphraism, further treatment by an orthopaedic spinal surgeon may be required. Sometimes however, treatment of the dysphraism may reduce or even improve the progression of the spine curvature.
Bladder and bowel control
The nerves that control bladder and bowel function are contained in the lower portion of the spinal cord and so can be affected by closed spinal dysphraism. The degree to which bladder and bowel control is affected depends on the severity of the defect.
Problems associated with the bladder are largely due to incomplete emptying, which is caused by the messages from the bladder not being transmitted to the brain well enough. Incomplete emptying of the bladder can lead to urinary tract infections (UTIs) and backflow of urine towards the kidneys (reflux), sometimes severe enough to damage the kidney. Signs of bladder problems include: urinary incontinence or dribbling, recurrent infections, bedwetting at night, needing to urinate frequently or having difficulties potty training. Bowel incontinence (soiling) is a less common problem, and rarely occurs if there are no bladder control problems. Early diagnosis and treatment can help reduce these problems but rarely solve them completely.
Movement
Closed spinal dysphraism can lead to muscle wastage on one side, affecting the buttocks and calf. This is caused by the muscles on one side being used more and therefore becoming stronger than the other, due to the stretching of the nerves leading away from the spinal cord when the cord is tethered. This can result in numbness, unbalanced walking, painless skin lesions, stiffness and pain in the lower limbs and back, sometimes relieved with odd postures or lying down. The physiotherapist will advise you about strengthening these muscles and improving their function as much as possible.
What about future pregnancies?
There is now evidence that an adequate intake of folic acid can dramatically reduce the risk of neural tube defects occurring in future pregnancies. If you are planning a further pregnancy, we recommend that you take 4mg of folic acid each day for at least three months before conception and for the first three months of pregnancy. This dose is higher than the standard recommendation for women who have not previously had a child with spina bifida. If you have any concerns about future pregnancies, please feel free to contact us.
What is a myelomeningocele?
In myelomeningocele, the neural tube has failed to close and the neural tissue is exposed at a place on the baby’s back called the ‘neural placode’. This most commonly happens in the baby’s lower back just above the bottom, but could occur anywhere along the spine. The myelomeningocele will look like a sac sticking out from your baby’s back.
How is myelomeningocele treated?
Without the protective covering of skin, the spinal cord will become further damaged, spinal fluid often leaks from the area and there is a very high risk of infection. Surgery is usually recommended within the first few days of life. The aim of surgery at this stage is to put the spinal cord back into the spinal canal and repair the defect in the back so that the area is covered with normal, healthy skin.
The physiotherapist will see your child after the operation. He or she will assess how much strength your child has in each muscle group and measure his or her sense of feel. When taken together, muscle strength, sensation and reflexes give us a picture of how well the messages are getting from the brain to the arms and legs via the spinal cord. The physiotherapist will also give advice on how to position and handle your child to stretch out tight muscles and to help with normal development.
Once your baby is recovering well, you will both be able to go home. We will need you to come back to the hospital between 10 and 14 days after the operation so that we can check the operation site, carry out an ultrasound scan of your baby’s head and measure his or her head circumference. The child is followed up on a regular basis.
What problems can myelomeningocele cause?
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Bladder function
There are a number of problems that might face a child born with myelomeningocele. However, we want to emphasise that these vary a great deal from child to child and also may show up at different times during a child’s development.
Hydrocephalus
The circulation of cerebrospinal fluid (CSF) is often disturbed in children with myelomeningocele. Either at birth or in the days and weeks following surgery, fluid may start to build up within the brain. This is called hydrocephalus and can result in increased pressure in the brain. If this occurs, an operation to place a shunt tube to divert the excess fluid from the brain to the abdomen is needed. This operation is needed in about 60 per cent of children with myelomeningocele.
Mobility
Myelomeningocele affects each child differently, and how each child moves around will vary too. Some children will need splints or walking aids, and others may move around more easily in a wheelchair. Your doctor will speak to you about how your child’s condition will affect their mobility.
What is the outlook for children with myelomeningocele?
The outlook for children with myelomeningocele has improved dramatically in recent decades. Intellectual prognosis is very good for the majority of children, most of whom will go on to full time education. Recreational and employment opportunities are better now than at any time in the past. However, this is a multidisciplinary approach and team work with parental support is a must for a good outcome.
GUJARATI
બરડા પરની ગાંઠ
સ્પાઇના બાઇફીડા કરોડરજ્જુની જન્મજાત ખોડ છે જેમાં કરોડનાં મણકાં ખુલ્લા રહી જાય છે. આ કારણે કરોડરજ્જુની નસો અને તેનાં પરનાં આવરણો કરોડનાં મણકાંની બહાર આવે છે. આ ખોડ નવજાત બાળકનાં બરડા પર ગાંઠના રૂપમાં આવે છે. સામાન્ય રીતે આવી ગાંઠ કરોડનાં મણકાંના કોઈપણ ભાગ-ગરદન, છાતી, કમર અને કમરનાં નીચેના ભાગમાં હોઈ શકે છે.
કરોડરજ્જુ અને તેની નસોનો વિકાસ ખામીયુક્ત હોવાનાં કારણે બાળકનાં બંને પગ ઓછા યા વધુ પ્રમાણમાં લકવાગ્રસ્ત હોઈ શકે છે અને ઘણી વાર પેશાબ-સંડાસ કંટ્રોલ કરતાં સ્નાયુ પણ નબળાં હોય છે. સ્નાયુઓની આ ખામી બરડાંની ગાંઠનું આૅપરેશન કરવાથી પણ સારી નથી કરી શકાતી અને બાળકને તેની સાથે જીવતાં શીખવું પડે છે.
સ્પાઇનાં બાઇફીડાવાળા ૫૦% થી ૬૦% બાળકોને માથામાં પાણી ભરાવાની શક્યતા પણ રહે છે. જેને હાઈડ્રોકેફલસ કહે છે. આને શંટ આૅપરેશન દ્વારા સા૨ું કરી શકાય છે. •
HINDI
पीठ पर गांठ (न्यूरल ट्यूब में दोष)
स्पाइना बाईफीडा रीड की हड्डी का जन्मजात दोष है, जिसमें रीड़ की हड्डी के मनकें खुले रह जाते हैं। इससे रीड की हड्डी की नसें और उसका ऊपरी भाग रीड की हड्डी के मनकों से बाहर निकल आता है। यह दोष नवजात शिशु की पीठ पर एक गांठ के रूप में उभर कर दिखाई देता है। सामान्य रूप से यह गांठ रीड़ की हड्डी के मनकें के किसी भी हिस्से – गरदन, छाती, कमर और कमर के नीचले हिस्से में हो सकती है।
रीड की हड्डी और उसकी नसों का विकास दोषपूर्ण होने के कारण बच्चे के पैरों की मांसपेशियाँ कमजोर हो सकती है, जिससे उसके शरीर का थोड़ा या अधिक हिस्सा लकवा ग्रस्त होता है। मल-मूत्र पर भी उसका नियंत्रण नहीं रहता। इस प्रकार का न्यूरोलोजिकल दोष पीठ की गांठ के ऑपरेशन से भी ठीक नहीं किया जा सकता और बच्चे को इस रोग के साथ जीना सीखना पड़ता है।
स्पाईना बाईफीड़ा रोग से ग्रस्त ५०% से ६०% बच्चों के सिर में पानी का भराव होने की संभावना होती है, जिसे हाइड्रोकेफेलस कहते हैं। शंट ऑपरेशन से इसे ठीक किया जा सकता है। •
Oesophagoscopy and Gastroscopy
What is an Oesophagoscopy and Gastroscopy?
An oesophagoscopy and gastroscopy is a procedure that allows the doctor to look inside your child’s oesophagus (the tube which goes down into their stomach from their throat, also called the gullet or foodpipe), stomach and duodenum (where the stomach joins the small intestine). To do this test, an endoscope (a thin, flexible tube with a bright light at the end) is passed through your child’s mouth and down into their stomach. This is carried out under general anaesthetic and the procedure lasts for about 30 minutes.
An oesophagoscopy and gastroscopy allows the doctors to find out what is causing your child’s problems without performing a larger operation.
Your child may need an oesophagoscopy and gastroscopy if he or she is having trouble swallowing, persistent vomiting or has previously had an operation on the foodpipe that needs checking. Your child may need dilatation if he or she has a narrowed foodpipe due to scarring from previous operations or illnesses. This may also be needed to take out foreign bodies like coins, safety pins or any other foreign objects that your child may have accidentally swallowed. The procedure also allows the doctors to take a biopsy (small piece of tissue) if needed. This can then be examined closely in the laboratories.
This procedure may also be needed to stretch your child’s foodpipe if it is narrower than usual during the procedure. This is called oesophageal dilatation.
Are there any risks with an OGD?
There is a very small risk that your child’s foodpipe could become damaged while it is being stretched, but this depends on the amount your child’s foodpipe needs stretching. Where possible, the doctors will carry out the dilatation several times on separate occasions, rather than risk stretching the foodpipe too much.

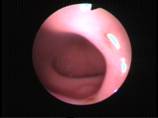

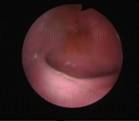
Gastroscopic views of different parts of the oesophagus, stomach and duodenum
What happens afterwards?
After the procedure, the doctor will remove the endoscope and give your child another type of medication to help them wake up. The child will remain sleepy after the procedure and this can last for two to four hours and during this time the child will be observed in hospital. Once your child is awake and sitting up on their own, they will be able to eat and drink.


Two coins stuck in the oesophagus
A swallowed button battery

Swallowed eraser removed
Oesophageal Atresia With Tracheo Oesophageal Fistula
What is oesophageal atresia?
Oesophageal atresia (OA) is a rare condition where a short section at the top of the oesophagus (gullet) is closed off. This means food cannot pass from the throat to the stomach.
What is tracheo-oesophageal fistula?
Tracheo-oesophageal fistula (TOF) is another rare condition, which tends to occur alongside oesophageal atresia. This is where the bottom end of the oesophagus is joined to the trachea (windpipe).
How are OA and TOF diagnosed?
Both OA and TOF tend to be diagnosed soon after birth. The doctor may try to pass a tube through the baby’s nose into the stomach (naso-gastric tube or NG tube), and find that it is not possible.
What causes them?
The causes of Oesophageal atresia are not known. It happens in 1 in 3000 to 1 in 5000 liver births. It is not due to anything that happened during pregnancy. OA and TOF can be associated with other problems like cardiac defects, bone or vertebral defects, anorectal malformations, kidney anomalies. All these will need to be looked for when a child is born with oesophageal atresia.
How are OA and TOF repaired? Are there any other options available?
This requires an operation. There are no other options or alternatives available for this.
What does the operation involve?
To repair the TOF, the surgeon will separate the oesophagus from the trachea and repair the part of the trachea where the oesophagus was originally joined. The method used to repair the OA depends on the distance between the ends of the oesophagus. In most cases, the surgeons will cut the blind end of the oesophagus and then join the two ends together to form a continuous passage from the throat to the stomach.
In rare cases called ‘long gap OA’ where the distance between the ends of the oesophagus are too large for the surgeon to be able to join them straightaway. Also in some children, the lower end of the oesophagus may not be connected with the trachea (pure oesophageal atresia without T.O.Fistula) . In these events a staged operation may be needed.
What happens afterwards?
The child comes back to the intensive care unit. The child may need help with breathing with either oxygen support or in some children with a ventilator. All babies are closely monitored after the operation. Your baby will be connected to monitors to check his or her breathing, heart rate and oxygen levels. He or she will also be given pain relief.
In a day or two, the child is started to be fed through the tube placed through the nose into the stomach. This continues for the next 5-7 days following which a study is done to show whether the repair has healed well. Following this, the child is fed milk orally. Once the doctors are happy that the child is feeding well, he or she is sent home. .
What is the outlook for children with OA and TOF?
If the OA and TOF occur on their own, with no other associated problems, the outlook for children who have them is good, with the majority growing up to live normal lives. The outlook for children with OA and TOF who have other difficulties varies depending on how severe these other problems are.
However, there are a couple of problems which may occur and which you should know about. They tend to happen most often in the first few years after the operation and improve as the child grows older.
The area of the trachea which was attached to the lower end of the oesophagus may become floppy or lax. This is called tracheomalacia. This leads to a distinctive loud ‘barking’ cough which is many a times scary for the parents. However, this tends to improve with age and has little effect on the child’s breathing when older.
Feeding problems may also occur due to the oesophagus narrowing where it was originally repaired. Sometimes it needs widening and this will be done with the help of endoscopes.
Some children who have had OA and TOF develop a problem with gastro-oesophageal reflux when they are older. This is where the contents of the stomach flow back up the oesophagus (gullet) causing pain and irritation. This needs treatment in the form of medications and dietary modifications. Severe and long standing cases or children with associated complications secondary to the gastro-oesophageal reflux may need operative treatment also. The doctor would be explaining details of the same if and when required. More details can be obtained from the ‘gastro oesophageal reflux’ leaflet.
Ovarian Cyst
An ovarian cyst is a pocket of fluid that can develop on an ovary.
Ovarian cysts are very common and can affect girls and women of any age. Ovarian cysts can appear as part of the way the ovary works normally. This type of cyst may not cause symptoms and does not usually need treatment.
However, sometimes cysts can be quite large and cause other problems such as pain. If this happens then surgery may be required to remove the cyst.
The majority of cysts in children and adolescents are benign (non-cancerous).
What causes an ovarian cyst?
The ovaries sit either side of the womb (uterus). Ovarian cysts occur when a pocket of fluid develops on the ovary.
There are two main types of ovarian cyst – functional and pathological.
Functional ovarian cysts are the cysts which develop as part of the way the normal ovary works. They are extremely common. They are harmless and usually disappear without treatment. They are always benign and often go unnoticed. However sometimes they can cause pain. This is usually because they twist or burst (rupture). Sometimes a small amount of bleeding can occur into the middle of the cyst. This is called a haemorrhagic cyst and can be painful.
Pathological ovarian cysts are cysts which are not part of the way the ovary normally works. There are several different types of pathological cyst including dermoid cysts and cystademomas. These cysts can grow and become quite large. As they grow they can cause pain. In addition they can also twist or burst or bleed.The majority of these cysts are benign but very rarely they can be cancerous.
Polycystic ovarian syndrome is when lots of small cysts form on the ovaries. They are caused by a hormonal imbalance and are harmless.
What are the signs and symptoms of an ovarian cyst?
Most ovarian cysts do not present any symptoms. But some can cause symptoms, including:
- sudden, sharp pain (which means the cyst may have burst)
- dull, aching feeling (which means the cyst may be large)
- bloated abdomen
- irregular or heavy periods
- frequent urination
- nausea or vomiting
Any sudden, sharp or persistent pain could be a sign that the ovarian cyst has burst. This can be serious and medical attention may be needed immediately.
How is an ovarian cyst normally diagnosed?
As most ovarian cysts do not present any symptoms, they often go undiagnosed. They may be spotted by chance due to an unrelated condition.
An ultrasound scan will confirm if a cyst is present and how big it is. The ultrasound scan will also be able to see what the inside of the cyst looks like.
Most functional cysts are filled with fluid only. Sometimes evidence of bleeding (haemorrhage) into the cyst can be seen on scan.
Pathological cysts are often a mixture of fluid and solid tissue. The scan can usually tell if there is a possibility that the cyst is cancerous. If there is a possibility that the cyst is cancerous, then more detailed tests such as a CT Scan or MRI scan may be suggested.
In addition a special blood test will be taken to look for “tumour markers”. These are hormones in the blood which can be at higher levels in cancerous cysts.
How is an ovarian cyst normally treated?
Treatment will depend on the size of the cyst, the symptoms presented and what the cyst looks like on ultrasound.
If the cyst is small and functional, then no treatment is needed. The cyst will go away on its own. A repeat scan is usually done in about six to eight weeks time to check the cyst has gone.
If the cyst is large or is causing pain then it may need removing at an operation. The majority of ovarian cysts are removed with laparoscopy or keyhole surgery. This means inserting a small telescope through the abdomen and to look at the cyst and remove it.
The recovery from this operation is usually very quick. In certain cases where the large cyst causes a torsion (twisting) or the ovary leading to gangrene (no blood supply) to the ovary. In such a scenario, the ovary along with the cyst will need to be removed.
If there is any concern that the cyst is cancerous then the ovary will need removing. This is also often done with keyhole surgery however sometimes a small cut will need to be put over the lower abdomen.
What happens next?
If a cyst has been removed at an operation, then laboratory test are done on the cyst to check there are no cancer cells there. If the tests confirm a benign cyst only then no further follow-up is needed. These cysts also rarely affect fertility.
If a cyst is confirmed as cancerous, then further treatment will be needed and the doctor would discuss this in more detail.
GUJARATI
અંડાશયમાં ગાંઠ
બાળકીનાં અંડાશયમાં થતી ગાંઠને ઓવેરીયન સીસ્ટ કહે છે. આ ગાંઠ છોકરીમાં જન્મથી કોઇ પણ ઉંમરે થઇ શકે છે અને પેટનાં નીચેનાં ભાગમાં દુઃખાવો કરે છે.
આ સીસ્ટ ઘણાં પ્રકારની હોય છે. મોટાભાગની સીસ્ટ સીમ્પલ અને હાનિરહિત હોય છે. વધુ પડતાં દુઃખાવા માટે બાળકીની સોનોગ્રાફી કરાવતાં ચોક્કસ નિદાન થાય છે. ઘણા ઓછા કેસમાં અંડાશયમાં કેન્સરની ગાંઠ પણ હોઇ શકે છે.
આધુનિક સર્જરી-લેપ્રોસ્કોપી દ્વારા આવી ગાંઠનું ચોક્કસ નિદાન થાય છે અને તે જ વખતે ગાંઠ કાઢી લેવાય છે. લેપ્રોસ્કોપી ના કારણે બાળકોનાં પેટ ઉપર કોઇ મોટા કાપા પાડવાની જરૂર પડતી નથી. •
HINDI
अंडाशय की गांठ
अंडाशय की गांठ अंडाशय के अंदर प्रवाही से भरी एक थैली होती है। इनमें अधिकतर कोई लक्षण नहीं दिखाई देते और ये हानिकारक नहीं होती हैं। कभी-कभी पेट अथवा कमर के नीचले भाग में दर्द हो सकता है। यदि यह गांठ फट जाती है अथवा अंडाशय में मोड़ उत्पन्न करती है, तो तीव्र दर्द अथवा उल्टी हो सकती है। कूपिक अंडाशय गांठ अंतर्गर्भाशयी काल में हो सकती है और जन्म से पूर्व अल्ट्रासाउंड स्कैन के द्वारा उदर में गांठ के होने का पता लग सकता है।
बच्चों में बड़े आकार की अंडाशय की गांठ के निदान और उपचार के लिए लेप्रोस्कोपी का प्रयोग नैदानिक एवं चिकित्सीय उपकरण के रूप में किया जाता है। बड़ी उदरीय गांठ के साथ जन्मी नवजात बालिका शिशु के मामले में लेप्रोस्कोपी सर्जरी को प्राथमिकता दी जाती है।•
Omphalomesenteric Duct / Vitello Intestinal Duct
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Vitello Intestinal Duct / Omphalomesenteric Duct
In the human embryo, the vitelline duct also known as the omphalomesenteric duct is a long narrow tube that joins the yolk sac to the midgut of the developing fetus. Generally, the duct narrows and disappears by the 9th week of intrauterine life. However, failure of the duct to close is termed as patent vitellointestinal duct or vitellointestinal fistula. This results in discharge of intestinal contents from the umbilicus. Sometimes it may emit foul smelling fluid discharge keeping the umbilicus persistently wet.
It is very difficult to pick up a patent vitello intestinal duct on ultrasound or by any other form of imaging. The only way to diagnose and treat this problem is laparoscopy. If need be, the native segment of the intestine connecting with the vitello-intestinal duct needs to be resected. ●
દૂંટી સાથે જાડાયેલું આંતરડું
આ પણ એક જન્મજાત ખોડ છે, જેમાં બાળકની નાળ કપાયા પછી દૂંટીની રૂઝ આવતી નથી અને દૂંટીમાંથી ચીકાશ, પાણી અને ઘણીવાર મળ જેવું વાસ મારતું પ્રવાહી આવે છે. જ્વલ્લેજ પાતળો સંડાસ પણ દૂંટી વાટે આવે છે.
આ ખોડનું કારણ નાનું આંતરડું દૂંટી સાથે જાડાયેલું રહેવાથી અથવા આંતરડાનો નાનો ભાગ દૂંટીમાં રહી જવાથી થાય છે.
દૂંટીનો મસો છે તેમ માની નિદાનમાં સમય ન બગાડતાં જરૂર પડે બાળકોનાં સર્જનની સલાહ લેવી જરૂરી છે. સોનોગ્રાફી તથા એક્ષ-રે આ પ્રકારની ખોડનાં નિદાનમાં મદદરૂપ થતાં નથી.
આધુનિક બાળસર્જરીની શોધને લીધે આ પ્રકારની ખોડની સારવાર લપ્રોસ્કોપીથી (દૂરબીન વડે ) કરવામાં આવે છે. જરૂર પડે આંતરડાનાં ભાગને પણ કાપીને જાઇન્ટ કરવો પડે છે. •
नाभि के साथ आंत का जुडा होना
मानव भ्रूण में, पीतक वाहिनी, जिसे ओम्फेलोमीसेंट्रीक डक्ट भी कहते हैं, एक लम्बी संकरी नलिका होती है जो अंडे की जर्दी की थैली को विकसित हो रहे भ्रूण के आद्यमध्यांत्र के साथ जोड़ती है। सामन्यतः यह नलिका संकरी होकर अंतर्गर्भाशयी काल के नौवे सप्ताह तक अदृश्य हो जाती है। तथापि, नलिका के बंद न हो सकने की स्थिति को पेटेंट विटीलोइंटेस्टीनल डक्ट अथवा विटीलोइंटेस्टीनल फिस्चुला कहते हैं। इसके परिणाम स्वरूप आंत्र सामग्री का नाभि से रिसाव हो सकता है। कभी-कभी इसमें से दुर्गंधयुक्त रसों का रिसाव हो सकता है, जिस कारण नाभि हमेशा गीली रहेगी।
अल्ट्रासाउंड या अन्य किसी अन्य प्रकार की इमेजिंग के द्वारा पेटेंट विटीलोइंटेस्टीनल डक्ट का पता लगाना कठीन है। लेप्रोस्कोपी ही इस समस्या के निदान और उपचार का एक मात्र तरीका है। यदि आवश्यक हो, विटीलोइंटेस्टनल डक्ट के साथ जुड़े आंत के जन्मज भाग को विभाजित कर दिया जाता है। •
Posterior Urethral Valves
How does the urinary system work?
The urinary system consists of the kidneys, the bladder and ureters. The kidneys filter the blood to remove waste products and form urine. The urine flows from the kidneys down through the ureters to the bladder. Another tube called the urethra takes urine from the bladder to the outside.
What are posterior urethral valves?
Posterior urethral valves (or P.U.Valves for short) are a condition found only in boys. It affects the urethra (the tube which runs from the bladder to the outside). In boys with PUV, the urethra has a blockage in it near the bladder. This makes it difficult for the child to pass urine. As the bladder pushes hard to get the urine out, it causes pressure which may result in urine being pushed back from the bladder into the ureters and kidneys. This causes the kidneys and bladder to swell and may lead to kidney damage.
What are the symptoms of PUV?
There are various symptoms associated with PUV, but they may not affect every child in the same way. The degree of blockage affects the severity of the symptoms. Some symptoms include:
- an enlarged bladder, so that it can be felt through the abdomen as a lump
- urinary tract infections (UTIs)
- difficulty in passing urine
- a weak stream of urine, the child passes urine in drops
- unusually frequent urination
- poor weight gain
How is it diagnosed?
PUV can be diagnosed by a routine ultrasound scan during pregnancy if the bladder, ureters or kidneys are swollen. It can also be diagnosed in a newborn baby if the bladder is swollen and urine dribbles constantly. If the blockage was not severe before or just after birth, the condition can remain undetected until the child has symptoms as above.
The severity of the blockage affects how the condition is diagnosed. Each case will be different, but the following tests are usual:
Ultrasound of the abdomen – this is very similar to the ultrasound scan that most women have during pregnancy. It creates a picture of the organs inside your son’s body and shows how well they are working.
Micturating cystourethrogram (MCUG) – this test shows urine passing from the bladder to the urethra and then to the outside. It will also show if the urine is flowing backwards towards the ureters and kidneys (this is known as reflux).
Cystoscopy – this is a scan which uses a small tube with a camera at the end to examine the inside of the bladder.
Blood tests – these will show how well your child’s kidneys are working and check that there is enough fluid inside the body.
Other tests and scans may be needed to check that other parts of the urinary system are working properly. These can include kidney and bladder function tests.
What causes PUV?
It is not inherited in any recognized way and seems to happen in the early stages of pregnancy when the organs, muscle and other tissue starts to form. It is not due to anything you did or ate during pregnancy.
How rare is it and who is affected?
PUV seems to occur in one in every 8000 births and affects only boys.
How can PUV be treated?
There are several options for treatment, depending on how severely the symptoms are affecting your child:
- The first course of action usually deals with the symptoms and includes putting a catheter (thin, plastic tube) into the bladder to drain away the urine. Any UTIs and fluid imbalance will also be treated with antibiotics and intravenous (IV) fluids, which are delivered directly into a vein.
- Next course of action is to try to remove the parts of the valve which are causing the backflow of urine into the kidneys. This is usually carried out using a cystoscope (a tube with a light on the end) rather than a traditional ‘open’ operation.
What is the outlook for children with PUV?
The outlook depends on how much damage has already occurred in the kidneys. This depends upon the blood test results of the child. Children operated for posterior urethral valves will need long term and regular follow up to check that there is no lasting damage to the urinary system following the problem.
Pleural Effusion (Empyema)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Pleural Effusion (Empyema) is a condition where pus collects in the pleural space (space outside the lung and inside the chest wall, often as a complication of pneumonia.
The lungs and inside of the chest cavity have a smooth covering called the pleura that lets the lungs expand without rubbing on the inside of the chest. The two layers of pleura are usually in close contact with only a small space in between (pleural space) filled with a small amount of pleural fluid acting as lubrication.
This complication of pneumonia usually occurs in three stages. Initially, clear fluid collects up in the pleural space which can then become infected. The fluid thickens and can affect the pleura, causing sections to ‘stick together’ eventually forming ’pockets’– this is called empyema. The infected fluid stops the lungs inflating completely, causing increasing breathing difficulties.
What causes empyema?
Empyema usually develops following pneumonia – various bacteria can cause pneumonia (most common ones are Staphylococcus pneumoniae and Staphylococcus aureus). Empyema seems to becoming more common, particularly in young children aged one to four years. It tends to occur during winter and spring season, when pneumonia and other chest infections are more common. Sometimes tuberculosis may also be a cause of empyema.
What are the signs and symptoms of empyema?
Empyema is usually suspected when a severe bout of pneumonia does not improve with treatment. Children usually show symptoms of being generally unwell with a high temperature. They may find breathing harder than normal, struggling to catch a breath. Their heart rate may also be higher than usual. Some children may describe pain in their chest when breathing.
How is empyema diagnosed?
If empyema is suspected, a chest x-ray may be the first test suggested to confirm or rule out the diagnosis. Chest x-rays will show white areas that suggest fluid. An ultrasound of the chest is more precise at showing the amount of fluid and the exact location and whether there are any pockets. In some cases, the doctor may also ask for a CT Scan of the chest to make sure that the child does not have any structural problems with the lung like a lung abscess which may have caused an empyema.
How is empyema treated?
Empyema previously used to be treated by placing a chest drain in the chest and with intravenous antibiotics as well as medicines to stop the pus clumping together.
However, nowadays with the advance of minimally invasive surgery, Empyema is treated with VATS (Video assisted thoracoscopic surgery) wherein a telescope is inserted into the chest cavity and all the pus is removed under vision. The pus pockets are broken down and washed with antiseptic liquids and a chest drain is placed. The surgery is completed with 2 or 3 5 mm instruments rather than placing a big cut on the chest. Also as the procedure is done undervision, the doctor is sure that the pus has been completely cleared and the child also recovers early.
What happens next?
The outlook for children with empyema is usually good once it has been diagnosed and treated promptly. Long term lung damage is rare. With thoracoscopy, the recovery is just in a few days. Once the lung is completely expanded as seen on follow up x-ray, the chest tube is removed and the child is sent home on oral medications. They will also need regular follow up clinic appointments, usually involving a chest x-ray, to check that the pleura is healing properly without any problems.
 Early Stage of Empyema (At Thoracoscopy)
Early Stage of Empyema (At Thoracoscopy)

 Late Stage of Empyema (At Thoracoscopy)
Late Stage of Empyema (At Thoracoscopy)
 Lungs seen after clearance of Empyema (At Thorascopy)
Lungs seen after clearance of Empyema (At Thorascopy)
 Late Stage Empyema (Needing open surgery)
Late Stage Empyema (Needing open surgery)
GUJARATI
એમપાઈમા
એમપાઇમા ન્યુમોનિયાને કારણે ફેફસાંની બહારના ભાગમાં થતાં પાણી અને પરૂના ભરાવાને કહેવામાં આવે છે. સામાન્ય રીતે ન્યુમોનિયા દવાઓથી સારું થઈ જાય છે પરંતુ બાળકમાં જ્યારે રોગ પ્રતીકારક શક્તિ ઓછી હોય અથવા જંતુઓનો પ્રભાવ વધારે હોય તો ન્યુમોનિયાના એક કામ્પ્લીકેશન તરીકે છાતીમાં ફેફસાંના બહારના ભાગમાં પરૂ અને પાણીનો ભરાવો થાય છે જેને એમપાઇમા કહેવામાં આવે છે. એમપાઇમામાં ફેફસું દબાણમાં આવે જેથી બાળકને શ્વાસ લેવામાં તકલીફ પડે છે અને તાવ પણ ખૂબ જ આવે. પહેલા એમપાઇમાની સારવાર માટે બે પાંસળીઓ વચ્ચે નળી મૂકી પરૂ આપોઆપ બહાર નીકળે અને સુકાય તેની રાહ જાવી પડતી હતી. આ માટે બાળકને ઘણીવાર અઠવાડિયાઓ અને મહિનાઓ સુધી હોસ્પિટલ માં રહેવું પડતું. હવે આધુનિક સાધનો અને લેપ્રોસ્કોપીના આગમન પછી બે પાંસળી વચ્ચે દુરબીન મૂકીને ફેફસાંની બહાર આવેલું બધૂજ પરૂ અને પ્રવાહી સંપૂર્ણપણે સાફ કરવામાં આવે છે. ફેફસું સામાન્ય રીતે ફૂલી જાય તેની ચોકસાઈ કરીને આૅપરેશન થઈ શકે છે. આ આૅપરેશન પછી બાળકને ત્રણ થી પાંચ દિવસ હોસ્પિટલ માં રહેવું પડે છે અને બાળક સંપૂર્ણપણે સ્વસ્થ અને સારુ થઈ જાય છે. આ દુરબીનની ટેક્નીકને થોરેકોસ્કોપી કહે છે. •
HINDI
एमपाइमा (छाती में रसी)
न्युमोनिया के कारण फेफड़ों के बाहरी भाग में उत्पन्न होने वाले पानी और रसी के जमाव को एमपाइमा कहते हैं। सामान्यतः न्युमोनीया दवाइयों से ठीक हो जाता है। लेकिन बच्चे की रोग प्रतिकारक शक्ति कमजोर हो अथवा किटाणुओं का प्रभाव अधिक हो, तो न्युमोनिया की जटीलता के कारण छाती के भीतर फेफड़ों के बाहरी भाग में पानी और मवाद का जमाव हो जाता है, जिसे एमपाइमा कहा जाता है। एमपाइमा के कारण बच्चे के फेफड़ों पर दबाव पड़ता है और तेज़ बुखार भी हो सकता है। पूर्व काल में एमपाइमा के उपचार हेतु दो पसलियों के बीच एक नली रख कर मवाद के अपनेआप सुख जाने की अथवा बाहर रीस जाने की प्रतीक्षा की जाती थी। इसके लिए बच्चे को हफ्तों और कई बार तो महीनों तक अस्पताल में भर्ती होना पड़ता था। लेकिन वर्तमान में आधुनिक उपकरणों के चलते और लेप्रोस्कोपी तकनीक के आने से दो पसलियों के बीच दूरबीन लगाकर फेफड़ों के बाहर का मवाद और प्रवाही को पूरी तरह साफ कर दिया जाता है। इस ऑपरेशन के पश्चात बच्चे को तीन से पाँच दिन अस्पताल में रहना पड़ता है जिसके बाद बच्चा सम्पूर्ण स्वस्थ हो जाता है। दूरबीन की इस टेकनीक को थोरेकोस्कोपी कहा जाता है। •
Phimosis
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
There are a number of conditions that can affect the foreskin (the piece of skin covering the top of the penis). They can affect boys of all ages and are usually easily treated.
The foreskin is the piece of skin that covers the top of the penis.
Conditions that can affect the foreskin include:
• Tight foreskin (Phimosis) – where the foreskin cannot be pulled back to reveal the head of the penis. All boys are born with phimosis. The foreskin retracts spontaneously by the age of 1 ½ to 2 years. A tight foreskin in puberty or adulthood can increase the risk of infection and cause problems with urination.
• Paraphimosis – A condition where the foreskin has retracted but gets trapped, restricting blood flow to the head of the penis. The penis will turn dark purple. Paraphimosis requires immediate medical attention as this condition can cause permanent damage to the penis if not treated early.
• Balanitis – an inflammation of the tip of the penis and foreskin usually caused by chemical irritation, bacterial or fungal infection. The head of the penis will become red, swollen and sore and there may be a thick and lumpy discharge.
What causes foreskin problems?
Foreskin problems can be the result of:
• Poor personal hygiene (not cleaning the head of the penis correctly)
• Infection
• Forcible attempts to retract the foreskin
What are the signs and symptoms of foreskin problems?
The appearance of the foreskin is usually enough to see whether there is a problem.
How are foreskin problems diagnosed?
In the case of paraphimosis (where blood flow is restricted and the penis turns purple), you should visit the hospital immediately as this condition can cause permanent damage to the penis.
How are foreskin problems usually treated?
In the case of infection, a child may be given a course of antibiotics or a steroid cream to reduce inflammation and irritation. The course of treatment may last between two and four weeks, depending on the severity of the strain of infection.
Some children may require a surgical procedure, such as:
• Circumcision – where the foreskin is removed altogether.
• Preputialplasty – where the opening of the penis is widened by an incision without removing the foreskin. The foreskin at the end of the operation would look just like a normal skin.
All of these procedures are carried out under anesthetic
Can foreskin problems be prevented?
Good hygiene is key to preventing problems that can be caused by infection.
In babies and children, the best way to clean the penis is by using water and baby soap. Don’t worry that you are not able to pull back the foreskin at this age – it’s very important not to try to retract a child’s foreskin forcibly, because this may cause damage to the delicate tissues of the penis. It could lead to bleeding, inflammation and the formation of scar tissue.
Once the foreskin begins to retract, the glans will naturally become more visible and easier to clean. It is important to be gentle – the less scrubbing the better. When boys reach adolescence, they should be encouraged to retract and clean their foreskin regularly.
What happens next?
Once treated, a child should not experience any further discomfort and there should be no further impact on his health.


 Acute Balanoposthitis
Acute Balanoposthitis

 Scarred prepuce
Scarred prepuce
 Photograph after circumcison
Photograph after circumcison
 Paraphimosis
Paraphimosis
 Zip Injury over prepuce
Zip Injury over prepuce
GUJARATI
ફાઇમોસીસ
ફાઇમોસીસ એટલે ઇન્દ્રિની ચામડી ઇન્દ્રિ ઊપર ચડી નહીં શકવાની ખોડ. બાળક જ્યારે જન્મે છે ત્યારે ઇન્દ્રિ તેની ખુદની ચામડીથી ઢંકાયેલી હોય છે. સામાન્ય સંજાગોમાં આ ચામડી ઇન્દ્રિ ઉપર ચડી શકતી નથી. કુદરતે આ વ્યવસ્થા એટલા માટે કરેલી છે કે જેથી બાળકના પેશાબની અંદર રહેલ એમોનિયાથી ઇન્દ્રિના મુખ અને પેશાબની નળીને નુકસાન ન થાય. સામાન્ય રીતે ઇન્દ્રિની ચામડી ઇન્દ્રિ ઉપર દોઢ થી બે વર્ષની અંદર આપોઆપ ચડતી થઈ જાય છે. પરંતુ દોઢ વર્ષની ઉંમર પછી પણ જા ચામડી ઇન્દ્રિ ઉપર ન ચડતી હોય તો આ બીમારીને ફાઇમોસીસ કહેવામાં આવે છે. ફાઇમોસીસની બીમારી માટે સુન્નત એટલે કે પેશાબની ચામડીનો આગળનો ભાગ કાઢી નાખવાની સર્જરી કરવામાં આવે છે. આ આૅપરેશન મુસલમાન, યહુદી અને બીજા ધર્મોમાં ધાર્મિક માન્યતાઓથી કરવામાં આવે છે. ચામડી સંપૂર્ણપણે ન કાઢવી હોય તો ‘Prepuceplasty’ નામની પણ એક સર્જરી કરી શકાય જેથી ચામડી ઇન્દ્રિ ઉપર આસાનીથી ચડી શકે અને ઇન્દ્રિનો દેખાવ નોર્મલ ઇન્દ્રિ જેવોજ રહેતો હોય છે. ફાઇમોસીસના કારણે ઘણીવાર ઇન્દ્રિના મૂખ ઉપર અને ઇન્દ્રિની ચામડીની અંદર ઇન્ફેક્શન પણ થાય છે. જેને ‘બેલેનોપોસ્થાઈટીસ’ કહેવામાં આવે છે. •
HINDI
फाइमोसीस
फाइमोसीस अर्थात इंद्रीय की त्वचा का इंद्रीय पर न चढ़ सकना। बच्चा जब जन्म लेता है तब उसकी इंद्रीय त्वचा से ढकी होती है। कुदरत ने यह व्यवस्था इसलिए रखी गई है ताकि बच्चे के मूत्र में उपस्थित अमोनीया के कारण इंद्रीय का मुख और मूत्र नलिका को हानि न होने पाए। सामान्यतया इंद्रीय की त्वचा इंद्रीय के उपर डेढ़ से दो वर्ष के भीतर अपने आप चढ़ती जाती है। लेकिन यदि डेढ़ वर्ष की आयु के बाद भी यदि त्वचा इंद्रीय के ऊपर नहीं चढ़ती है तो इसे फाइमोसीस कहते है। फाइमोसीस की बीमारी के लिए सुन्नत अर्थात इंद्रीय की चमड़ी के आगे के भाग को सर्जरी के द्वारा काट दिया जाता है। मुस्लिम, यहुदी और अन्य कुछ धर्मों में यह ऑपरेशन धार्मिक मान्यताओं के आधार पर किया जाता है। कई बार यदि चमड़ी पूरी तरह से न हटानी हो तो ‘प्रेप्युझ्प्लास्टी’ नामक सर्जरी की जा सकती है, जिससे की चमडी इंद्रीय के उपर आसानी से चढ़ सके और इंद्रीय का आकार सामान्य रहे। फाइमोसीस के कारण कई बार इंद्रीय के मुख पर और इंद्रीय की चमडी के भीतर संक्रमण हो जाता है। इसे ‘बेलेनोपोस्थाइटीस’ कहा जाता है। •
Pyloric Stenosis
Pyloric stenosis is when the passage between the stomach and small bowel (pylorus) becomes narrower. The passage is made up of muscle, which seems to become thicker than usual, closing up the inside of the passage. This stops milk or food passing into the bowel to be digested.
What are the symptoms of pyloric stenosis?
Pyloric stenosis is commonly seen in the first born male child of the family. In most cases, a baby with pyloric stenosis is well until the age of 3-4 weeks following which the child will begin bringing up small amounts of milk after feeding. Over a few days this will become worse until the baby can no longer keep any milk down. This vomiting may become so forceful that the milk may be projected for several feet out of the baby’s mouth. This is called projectile vomiting.
As the milk is lying in the acid in the stomach, it can curdle and become yellow in colour. This also reduces the amount of faeces (stool) passed, as little or no food is reaching the bowel.
If the condition is not treated, the baby will become dehydrated and not gain weight. Signs of dehydration include lethargy, reduced urine output and the soft spot (fontanel) on the top of the head may be sunken.
What causes pyloric stenosis and how common is it?
Pyloric stenosis is a fairly common reason for babies needing an operation and usually develops around four to six weeks after birth. We do not know exactly why pyloric stenosis develops, but it tends to affect more boys than girls, and seems to run in families too.
How is pyloric stenosis diagnosed?
The thickened pyloric muscle can be felt, especially during feeding, as a small, hard lump on the right side of the baby’s stomach. The muscles around the stomach can sometimes be seen straining, moving from left to right as they try to push milk through the pylorus.
Sometimes the doctors may want to confirm the diagnosis using tests and scans. These can include an ultrasound scan or even a contrast swallow and x-ray examination.
How is pyloric stenosis treated?
Pyloric stenosis is usually treated in an operation under general anaesthetic, lasting about 30 minutes. The operation is called a pyloromyotomy. Most are carried out using keyhole surgery (laparoscopically) but occasionally open surgery is suggested.
The effects of pyloric stenosis, like dehydration due to the vomiting, can become serious quite quickly in children, and so there are no alternatives to the operation.
What happens before the operation?
If your child is dehydrated, he or she will need a ‘drip’ of fluids for a while before the operation. This will make sure that your child’s blood contains the right balance of salts and minerals, and treats the dehydration. Your child will have the operation once his or her blood test results are normal.
They will also need a nasogastric tube, which is passed up the nose, down the food-pipe and into the stomach. This will drain off the stomach contents before the operation.
What does the operation involve?
The surgeon will cut through some of the thickened muscle, which widens the passage so that milk and food can pass into the bowel to be digested. If the operation was carried out using keyhole surgery, your child will have three small incisions in the abdomen, which will be closed with dissolvable stitches and skin glue. If your child has had open surgery, there will be a larger incision by the belly button, closed with dissolvable stitches,
What happens afterwards?
Your child will come back to the ward to recover. He or she will have been given pain relief during and after the operation. For the first few hours, your child will continue to have fluids through the drip so that the stomach and bowel can start to heal. After twelve hours or so, we will start to feed your child, starting with small amounts, and increasing the amount as he or she tolerates it. Your child may still have some vomiting but this will improve as the digestive system recovers from the operation. Your child will be able to go home once he or she is feeding well.
What is the outlook for children with pyloric stenosis?
Most pyloric stenosis operations are successful, with the immediate effect of reducing or stopping completely any vomiting after feeds.
Pediatric Anaesthesia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
PEDIATRIC ANAESTHESIA
A major concern of all parents for their child undergoing surgery is anaesthesia. Most of the parents are worried as to how can a small child be anaesthetized and whether the procedure can be done under a local anaesthetic. One of the major concerns is whether the child will recover uneventfully from the anaesthetic.
Anaesthesia is an age old scientific speciality. As with other specialities, pediatric anaesthesia has also advanced over the years. Anaesthesiologists specially trained in the field of pediatric anaesthesia can now safely anaesthetize even new born and premature children.
Operating under local anaesthesia is most of the times not possible in children as the child is not co-operative and gets scared amongst unknown people and enviornment in the operating room.
Maintainence of anaesthesia during surgery is done using the most modern medicines and latest equipments which are safe and have the least side effects. ●
GUJARATI
પીડીઆટ્રીક એનેસ્થેસીઆ
મોટા ભાગનાં મા-બાપને તેમના બાળકનું આૅપરેશન કરાવતાં પહેલા એક જ સવાલ હોય છે. “આટલા નાના બાળકને બેભાન કરી શકાય?”, “બાળકને લોકલ એનેસ્થેશિઆ ના અપાય?”, “બાળક કોમામાં નહીં જાય ને?”
એનેસ્થેશિયાને સામાન્ય ભાષામાં “શીશી સૂંઘાડવા” તરીકે ઓળખાય છે.
શીશી સૂંઘાડવાની રીત ખૂબ જ દાયકાઓ જૂની હતી. હાલમાં એનેસ્થેશિયા માટે ઇન્જેક્શન દ્વારા નસમાં દવા અપાય છે અને બાળકને સેકંડોમાં બેભાન કરી શકાય છે.
એનેસ્થેશિયાના ખૂબ જ આધુનિક સાધનો દ્વારા નાનામાં નાના બાળકને (અધૂરા માસે જન્મેલા બાળકને પણ) બેભાન કરાય છે અને મશીન બંધ કરતાં, બાળકને તરત ભાનમાં લાવવામાં આવે છે. આ કાર્ય માટે બાળકના નિષ્ણાંત એનેસ્થેટીસ્ટ ડાક્ટર કામ કરે છે.
બાળકોમાં મોટે ભાગે લોકલ એનેસ્થેશિયા આપી શકાતો નથી કારણ કે બાળક આૅપરેશન થિએટરમાં ગભરાઈ જાય છે અને સર્જનને સહકાર આપતું નથી જેથી આૅપરેશન કરી શકાય નહીં. “જનરલ એનેસ્થેશિયા” હવે ખૂબ જ સલામત છે તેથી “લોકલ એનેસ્થેશિયાની” ચોઈસ ડાક્ટર તથા માતા-પિતા નથી લેતા. •
HINDI
पीडीऐट्रीक ऐनेस्थेशिया
अपने बच्चे का ऑपरेशन करवाने से पहले अधिकतर माता-पिता के मन में कई सवाल उठते हैं- जैसे कि क्या इतने छोटे बच्चे को बेहोश किया जा सकता है क्या बच्चे को लोकल ऐनेस्थेशिया दे सकते हैं कहीं बच्चा कोमा में तो नहीं चला जाएगा आदि।
आमतैर पर यह मानते है कि बच्चे को शीशी सुंघाकर बेहोश किया जाता है, जो कि बहुत पुरानी पद्धति थी। आज के समय में ऐनेस्थेशिया के लिए इन्जेक्शन से नस में दवा दी जाती है और बच्चा कुछ सेकण्डों में बेहोश हो जाता है।
ऐनेस्थेशिया द्वारा अत्याधुनिक उपकरणों से छोटे से छोटे बालक को बेहोश कर सकते हैं और मशीन बंद करके बच्चों को तुरंत होश में ला सकते हैं। यह कार्य बाल विशेषज्ञ ऐनेस्थेटीस्ट डॉक्टर द्वारा किया जाता है।
लोकल ऐनेस्थेशिया देकर बच्चे का ऑपरेशन करना संभव नहीं हो पाता। क्योंकि बच्चा ऑपरेशन थिएटर और अनजान लोगों को देखकर डर जाता है और ऑपरेशन के दौरान डॉक्टर को सहयोग नहीं करता।
जनरल ऐनेस्थेशिया द्वारा सर्जरी के दौरान अत्याधुनिक दवाओं और विशेष उपकरणों से बच्चे को बेहोश रखा जाता है, जो कि सुरक्षित तरीका है। •
Pediatric Surgery
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
PEDIATRIC SURGERY
Pediatric surgery is an age based surgical super-speciality and has developed for surgery of children from birth to 18 years of age. Pediatric Surgery in India is almost 50 years old. Since the last two decades, lots of efforts and research is done in the field of Fetal surgery where the unborn child with birth defects can be operated in the mother’s womb itself.
Why is pediatric surgery a super-speciality ?
- A child is not a small adult. Hence, the care, drug dosage, I.V. fluid management etc is not 1/2, 1/3rd or 1/4th of that of an adult. A child needs specialized care.
- Congenital defects seen in children are not seen in adults.
- Looking at the delicacy of neonatal and pediatric surgery, specialized operation theatres, instruments and anaesthesia equipments are required.
- Surgery of a neonate requires special care and expertise. If proper care is taken, children with major surgeries respond fantastically and recover very quickly.
- Minimally invasive surgery in children also requires specialized infrastructure and equipments. ●
GUJARATI
પીડીઆટ્રીક સર્જરી (બાળ-સર્જરી)
પીડીઆટ્રીક સર્જરી જન્મથી ૧૮ વર્ષ સુધીનાં બાળકો માટે સર્જરીની એક સુપર સ્પેશ્યાલીટી છે. આ સ્પેશ્યાલીટી ભારતમાં છેલ્લા ૫૦ વર્ષથી છે. છેલ્લાં બે દાયકામાં માતાના ગર્ભમાં રહેલ બાળકમાં જા કોઇ ખોડ-ખાંપણ જણાય તો તેનાં આૅપરેશન કરવા માટે પ્રયત્નો શરૂ થઇ ગયા છે (ફીટલ સર્જરી)
પીડીઆટ્રીક સર્જરી : સુપર સ્પેશ્યાલીટી શા માટે?
૧. નવજાત બાળકમાં જાવા મળતી બીમારીઓ અને ખોડ-ખાંપણ અન્ય ઉંમરમાં જાવામાં નથી આવતી.
૨. બાળક એ કોઈ નાનું વડીલ નથી. તેને જાઈતી દવાઓ, ગ્લુકોઝ, એન્ટીબાયોટીક વિગેરેની ચોક્કસ માત્રા એની ઉંમર અને વજન પ્રમાણે અપાય છે.
૩. નવજાત બાળકની સર્જરી સૌથી વધુ કાળજી માંગે છે. કાળજીપૂર્વક અને સમયસર આૅપરેશન કરવામાં આવે તો બાળકો ગમે તેટલાં મોટા આૅપરેશન પછી સારા થઈ જાય છે.
૪. બાળકનાં આૅપરેશનમાં તેની નાજુકતાને ધ્યાનમાં લઈ, આૅપરેશન થિયેટર, આૅપરેશનના સાધનો, એનેસ્થેશિયાનાં સાધનો સ્પેશ્યલ હોય છે.
૫. બાળકોમાં લેપ્રોસ્કોપી (દૂરબીનથી થતાં આૅપરેશનો) પણ સ્પેશ્યલ સાધનો અને કાળજી માંગી લે છે. •
HINDI
बाल चिकित्सा सर्जरी
बाल चिकित्सा सर्जरी जन्म से १८ वर्ष तक की आयु के बच्चे के लिए सर्जरी का एक सुपर-स्पेशियालीटी तरीका है, जो भारत में पिछले ५० वर्षों से प्रचलन में है। माँ के गर्भ में रहने वाले बालक में किसी जन्मजात रोग की पहचान होने पर माँ के गर्भ में ही उसका ऑपरेशन करने के कई प्रयास पिछले दो दशकों से किये जा रहे हैं, जिसे फीटल सर्जरी कहा जाता है।
बाल चिकित्सा सर्जरी बहुत विशिष्ट क्यों हैं?
१) नवजात बच्चे में दिखाई देनेवाली बीमारियाँ/दोष बड़ी उम्र में पहचान में नहीं आती।
२) बच्चा, कोई छोटा वयस्क नहीं होता। इसलिए उसके लिए जरूरी दवाएँ, ग्लूकोज, ऐन्टीबायोटिक आदि सही मात्रा में उसके वजन के अनुसार दिया जाता है, जिसके लिए विशेष ध्यान रखने की जरूरत है।
३) नवजात और छोटे बच्चे की सर्जरी में सबसे अधिक सावधानी रखने की आवश्यकता है। इसके लिए विशेष आधुनिक ऑपरेशन थिएटर, उपयुक्त उपकरण और बेहोश करने के साधनों की जरूरत पड़ती है।
४) नवजात की सर्जरी किसी विशेषज्ञ द्वारा विशेष देखभाल में की जानी चाहिए। यदि समय पर बच्चे की ठीक से सर्जरी की जाए तो जटील सर्जरी के बावजूद बच्चा जल्दी ठीक हो जाता है।
५)बच्चे की लेप्रोस्कोपी सर्जरी में विशेष साधनों के इस्तेमाल करने के साथ इसे कुशल सर्जन द्वारा किये जाने की आवश्यकता है।•
Polydactyly & Syndactyly (Joined fingers / toes)
INFORMATION AVAILABLE IN ENGLISH , GUJARATI AND HINDI
Syndactyly :
Syndactyly means ‘joined digits’ and may involve webbing of the skin, or include fusion of the underlying bones. This may be along part or the whole length of the finger. It is the second most common congenital hand problem and occurs in around 1 in 1000 births.
Hand development occurs in the early stages of pregnancy and the fingers separate in the ninth week. Syndactyly happens when two or more fingers fail to completely separate during development.
Sometimes syndactyly occurs by chance or it may be inherited. In rare circumstances, it may occur along with other signs as part of a syndrome (collection of signs).
Syndactyly can occur unilaterally (on one hand only) or bilaterally (affecting both hands), and can affect two or more fingers. Occasionally it may be associated with extra digits or other abnormalities in the hands.
Syndactyly can also affect the toes, involving webbing of the skin or fusion of the underlying bones along part or the whole length of the toe.
How is syndactyly treated?
It is treated surgically under a general anaesthetic. Surgery is usually only possible to one side of a finger at a time, as any damage to the blood supply on both sides could result in the loss of the finger. So, if your child has syndactyly of three or more digits next to each other, they will need more than one operation.
Are there any alternatives to surgery?
Surgery is the only option to separate the digits. The aim of the operation is to improve function (how well your child can use their hand) and sometimes appearance (how your child’s hand looks).
Occasionally, some children could manage without treatment. Correction of toe syndactyly is usually for cosmetic rather than functional reasons.
What does the operation involve?
The surgeon will recreate a new web with local flaps of skin from the sides of the digits. This usually involves making a series of zig-zag incisions along the digits, and wrapping the zig-zag pieces of skin to cover up the inside surface of the digits where they were previously joined.
In most cases, the surgeon will need to use a skin graft to cover up any gaps. This will be a different colour on the hand than the rest of the skin. Occasionally, a skin graft will not be needed.
Are there any risks?
There is a risk of infection as the skin is opened, but your child will be given antibiotics to reduce the risk of this. If an infection does occur, it is usually minor and easily treated with a course of antibiotics.There is a chance that the skin graft will not ‘take’, but looking after it carefully will help the operation site to heal as well as possible. Any infection or graft loss may affect the time the wounds take to heal and therefore the resulting scars.
The amount of scarring varies from child to child. If your child tends to scar easily from cuts and grazes, it is likely that they will have noticeable scars after the operation, but these will fade in time.
What happens after the operation?
Their hand or foot will be covered in a large bandage to protect the skin grafts while they heal. Your child will soon find a way to use their bandaged hand or foot in everyday activities. It is best to keep the limb operated on raised above the level of the heart as much as possible to reduce any swelling, which in turn reduces any pain.It also minimises any oozing under the flaps and skin grafts. Your child’s limb may be raised using pillows or soft toys, or the hand may be placed in a sling when sitting or walking around.If your child’s fingertips or toes are visible, check them on a regular basis for warmth, colour, sensation, movement and blood flow. These checks show that the blood is flowing properly.
What is the outlook for children with syndactyly?
This depends on the degree of syndactyly and whether it occurred by chance or as part of a syndrome. The outlook for children with simple syndactyly is usually excellent. If the syndactyly occurred as part of a syndrome, the outlook depends on the particular syndrome and associated features.
Polydactyly:
Polydactyly is a condition where the child has supernumary fingers or toes. It can present in either one or both hands and / or feet. Most of the times the extra digit is usually a piece of soft tissue on a tiny stalk. Sometimes, it may contain bone without joints and rarely it may be a complete functioning digit.
Surgery for polydactyly is recommended between 1 – 1 1/2 years of age. A rudimentary accesory digit may sometimes undergo torsion needing an emergency surgery. ●
GUJARATI
બાળકની આંગળીઓની ખોડ
બાળકનાં હાથ અને પગની આંગળીઓમાં ઘણી ખોડ જાવા મળે છે. જા એક-બે આંગળીઓની ખોડ હોય તો સર્જરીનાં રીઝલ્ટ સારા આવે છે પણ ઘણી વખત હાથ કે પગની આંગળીઓની સાથે તેમાં રહેલાં હાડકાં પણ ખોડ વાળા હોય તો બાળક આ ખોડ સાથે સારું કામ કરી શકે તેવી સર્જરી કરવામાં આવે છે. આમાં સંપૂર્ણ નોર્મલ દેખાય તેવાં હાથ નથી કરી શકાતા.
આ ખોડ ૧ ૧/૨ વર્ષની આસપાસ આૅપરેશન દ્વારા છૂટી કરી શકાય છે.
હાથ કે પગમાં પાંચ આંગળીઓ કરતાં વધુ હોય તો તેને પોલીડેક્ટલી કહેવામાં આવે છે. સામાન્ય રીતે એક્સ્ટ્રા આંગળીઓ કાઢવાની સર્જરી ૧ વર્ષ પછી કરાવવી, પણ જા એક્સ્ટ્રા આંગળી ફક્ત ચામડીથી જાડાયેલી હોય અને તેમાં વળ ખાઈ ગેંગરીન થાય છે તો તે માટે તાત્કાલિક આૅપરેશન કરાવવું પડે છે. •
HINDI
बच्चों की अंगुलियों की विसंगति
सींडेक्टली अर्थात ‘जुड़ी हुई अंगुलियाँ’ वह स्थिति है जब बच्चे के विकास के दौरान दो या दो से अधिक अंगुलिया पूरी तरह से अलग नहीं हो पाती है। कभी-कभी कुछ बच्चे बिना किसी उपचार के भी कार्य कर सकते है। पैर के अंगूठे के सिंडेक्टिली का उपचार आमतौर पर कार्यात्मक कारणों से अधिक कॉस्मेटिक कारणों से किया जाता है (ताकि बच्चा चप्पल/स्लीपर पहन सके)। सर्जरी के लिए कभी-कभी त्वचा निरोपन की आवश्यकता पड़ती है।
पॉलीडेक्टीलीमें बच्चे को अतिरिक्त अंगुलियाँ अथवा अंगूठे होते हैं। यह एक या दोनों हाथ अथवा पांव में हो सकती है। अधिकतर मामलों में ये अतिरिक्त अंगुलियाँ छोटे से डंठल पर नर्म मांस-तंतु के समान होती हैं। कभी-कभी इनमें बिना किसी जोड़ के हड्डी होती है; और यह शायद ही कभी पूर्णतया कार्यशील अंगुली के रूप में होती है। सींडेक्टली के लिए सर्जरी १भ वर्ष की आयु होने पर की जाती है। अतिरिक्त अंगुली केवल त्वचा से जुड़ी हो और इसमें मरोड़ उत्पन्न हो जाए तो यह एक आपात स्थिति पैदा कर सकती है। •
Palate (Cleft Palate)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Cleft Palate
A cleft palate is a defect or gap in the roof of the mouth. It can involve some or all of the part of the palate.
A cleft palate can occur separately or together with a cleft lip.
What causes a cleft palate?
A cleft palate occurs during the first weeks of development in the womb. The palate is initially formed in two halves, lying either side of the tongue. Around the seventh or eight week the palate joins. This joining process may fail completely or stop at any point, resulting in a defect (cleft).
In any unaffected family, the chance of cleft lip / palate is one in 700. If one parent or child has a cleft, the chance of cleft lip / palate in future children is one in 25 to one in 40.
What are the signs and symptoms of cleft palate?
The main symptoms are the effect the condition has on hearing, feeding and later speech.
If a baby has an isolated cleft palate, they might have difficulty feeding properly because they can’t suck very well. The baby is unable to create a seal enabling them to create suction to get milk from the breast or bottle.
Some special bottles are used to help babies with isolated cleft palates feed but difficulty with feeding can mean the baby gains weight more slowly than is meant to happen over the first few months.
Other symptoms can include hearing problems as children with the condition are more at risk of glue ear. This can also lead to ear infections. As the palate plays an important role in speech it is important the cleft is repaired with surgery to reduce speech problems when the child is older.
How is a cleft palate normally diagnosed?
A cleft palate will be seen once a baby is born and is usually diagnosed at the time of the routine newborn baby check.
How is a cleft palate treated?
Treatment involves surgery. Most children require just one operation, but sometimes other operations may be needed to ensure the best possible speech outcome.
An operation to repair a cleft palate usually takes place when a child is between nine and 12 months of age. The operation involves joining the tissues that have not joined before birth.
What happens next?
In the vast majority of cases, surgery is very successful. Most babies born with a cleft palate will lead totally normal lives.
Children with a cleft palate will be monitored closely as they grow and develop. This will include their hearing and speech.
Most children are able to develop good speech and language skills following surgery. But sometimes a repaired cleft palate can make it difficult for a child to pronounce some sounds clearly. This may affect speech quality making it sound a bit ‘nasal’. A speech and language therapist will be able to help. However, most children will be able to speak normally.


 Cleft Palate
Cleft Palate

 After Repair
After Repair
GUJARATI
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું
કપાયેલો હોંઠ અને ફાટેલુંં તાળવું દર છસો એ એક બાળકમાં જાવામાં આવે છે. ઘણીવાર બાળકનો ફક્ત હોંઠ જ કપાયેલો હોય છે. જ્યારે ઘણીવાર હોંઠ, તાળવું અને પેઢું ત્રણે કપાયેલા હોય છે. માતા અથવા પિતામાં જા કપાયેલો હોંઠ અને ફાટેલું તાળવું હોય તો તેમનાં બાળકોમાં પણ આ ખોડ આવવાની શક્યતા બીજા બાળકો કરતાં વધારે રહેલ છે. ફાટેલું તાળવું હોવાથી બાળક સ્તનપાન નથી કરી શકતું તેથી આવા બાળકોને એક વિશેષ પ્રકારની બોટલ અથવા વાટકી અને ચમચીથી દૂધ પીવડાવવું જાઈએ. સ્તનપાન કરાવવાથી અથવા સાદી દૂધની બાટલીઓથી ઘણીવાર બાળકને આંતરાશ જઈ બાળકની જિંદગીને જાખમ પણ ઊંભું થતું હોય છે. કપાયેલા હોંઠનું આૅપરેશન ત્રણ મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાનું આૅપરેશન નવ થી બાર મહિનાની ઉંમરમાં કરવામાં આવે છે. ફાટેલા તાળવાના આૅપરેશન પછી બાળકોને ઘણીવાર વાંકાચૂકા દાંતની સારાવાર કરવાની જરૂર પડે છે. સ્પીચ થેરાપીની પણ જરૂર પડી શકે છે. •
HINDI
कटा होंठ और फटा तालु
कटा होंठ और फटा तालु हर ६०० में से एक बच्चे में देखा गया है। कई बार बालक का केवल होंठ ही कटा हुआ होता है। जबकि कभी-कभी होंठ, तालु और मसूड़े तीनों ही फटे हुए होते हैं। यदि माता या पिता में से किसी को भी कटे होंठ या फटे हुए तालु की समस्या है तो, उनके बच्चों में अन्य बच्चों के अपेक्षा यह दोष होने की संभावना अधिक रहती है। कटे होंठ या फटे तालु के साथ जन्मे शिशु को स्तनपान करने में तकलीफ होती है। अतः ऐसे बालक को विशेष प्रकार की बोतल या कटोरी-चम्मच से दूध पिलाना पड़ता है। सामान्य स्तनपान अथवा दूध की बोतल से दूध पिलाने पर कई बार दूध बच्चे के फेफडे में जाने की संभावना है और बच्चे की जान को खतरा पैदा कर सकता है। कटे होंठ का ऑपरेशन तीन महीने की उम्र में किया जाता है। फटे तालु का ऑपरेशन नौ से बारह महीने की आयु में किया जाता है। फटे तालु के कारण कई बार दांतों का उपचार अर्थात टेढ़े-मेढ़े दांतों के उपचार की आवश्यकता होती है। स्पीच थेरापी की भी आवश्यकता हो सकती है।•
Paraumbilical hernia / Umbilical hernia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Umbilical and Paraumbilical Hernia
Umbilical hernia is seen in 5 % of children. The umbilical cord is attached to the area of the umbilicus in the intrauterine life. This area has a defect in the abdominal wall which closes after birth and forms the belly button. When this defect does not close spontaneously, the intestines may bulge through it when the child cries or strains and is called an umbilical hernia.
Umbilical hernias normally resolve spontaneously by the age of 2 years. If the size does not reduce after 2 years, then surgery is advisable. Application of coins or belts does not help in cure of umbilical hernias.
Many a times, the hernia may not be located at the umbilicus, but around it. These are called para umbilical hernias. Paraumbilical hernias do not resolve spontaneously. They also have a chance of the intestine getting blocked in the defect. Hence early surgery is advisable in cases of paraumbilical hernias unlike umbilical hernia. ●
 Umbilical Hernia
Umbilical Hernia

 Supra Umblical Hernia
Supra Umblical Hernia

 Application of Belts and Coins should be avoided
Application of Belts and Coins should be avoided
 Postoperative photo after Umbilical Hernia Repair
Postoperative photo after Umbilical Hernia Repair
GUJARATI
મોટો દૂંટો (દૂંટીની સારણગાંઠ)
દૂંટીની સારણગાંઠ ૫% બાળકમાં જાવા મળે છે. બાળક માઁ ના ગર્ભમાં હોય ત્યારે નાળ દૂંટીના ભાગમાં જાડાયેલી હોય છે. બાળકના જન્મ પછી નાળ ખરી જાય છે અને તે રસ્તો બંધ થઈ જાય છે. આ રસ્તો બંધ ન થવાથી પેટની દીવાલમાં કાણું રહી જાય છે, જેમાંથી આંતરડા બહાર નીકળી ને મોટો દૂંટો કે દૂંટીની સારણગાંઠ કરે છે. દૂંટીની સારણગાંઠ ૨ વર્ષની ઉંમર સુધીમાં જાતે મટી જાય છે. દૂંટીની સારણગાંઠમાં સિક્કા કે બૅલ્ટ બાંધવાથી કોઈ ફાયદો થતો નથી.
બાળક બે વર્ષનું થાય ત્યાં સુધીમાં દૂંટીની સારણગાંઠ મટી ન હોય તો તેના માટે આૅપરેશન કરવું જરૂરી બને છે. આૅપરેશન સામાન્ય અને જાખમ વગરનું હોય છે. આ આૅપરેશનમાં પેટની દીવાલમાં કાણું હોય તેને ટાંકા વડે બંધ કરી દેવામાં આવે છે. ઘણીવાર દૂંટીના આજુબાજુના સ્નાયુઓમાં જગ્યા હોવાથી પણ મોટો દૂંટો બનતો હોય છે. આ તકલીફને પેરાઅÂમ્બલીકલ હર્નિયા કહેવાય છે. આ ખોડ જાવામાં તો મોટા દૂંટા જેવી જ લાગતી હોય છે, પરંતુ બાળકોના સર્જનને બતાવ્યા પછી જ આ ખોડ પેરાઅÂમ્બલીકલ હર્નિયા છે કે નહીં તે ખબર પડે છે. પેરાઅÂમ્બલીકલ હર્નિયામાં આંતરડું ફસાવાની શક્યતા રહેલી છે. મોટા દૂંટાથી વિપરીત પેરાઅÂમ્બલીકલ હર્નિયામાં જેટલું બને તેટલું વહેલું આૅપરેશન કરવું જરૂરી છે. •
HINDI
नाभि तथा नाभि के पास हर्निया
नाभि हर्निया ५% बच्चों में पाया जाता है। अंतर्गर्भाशीय काल के दौरान गर्भनाल नाभि के क्षेत्र में नाभि से जुड़ा हुआ होता है। इस क्षेत्र में पेट की दीवार में एक दोष होता है जो जन्म के बाद बंद हो जाता है और पेट बटन का निर्माण करता है। जब यह दोष स्वतः बंद नहीं होता है, तब बच्चे के रोने पर अथवा तनाव लाने पर आंतो में उभार उत्पन्न होता है जिसे नाभि हर्निया कहा जाता है। नाभि हर्निया सामान्य रूप से २ वर्ष की आयु तक अपने आप ठीक हो जाता है। यदि २ वर्ष के बाद आकार में कमी नहीं आती है, तो शैल्यचिकित्सा उचित होगी। सिक्कों या बेल्टों का उपयोग नाभि हर्निया के इलाज में मदद नहीं करता है। कई बार, हर्निया नाभि पर स्थित नहीं होता है, लेकिन इसके आस-पास होता है। इन्हें नाभि के पास या परानाभि हर्निया कहते हैं। परानाभि हर्निया अपने आप नहीं मिटता। इस हर्निया में दोष क्षेत्र में आंत में रुकावट होने की भी संभावना है। इस वजह से नाभि हर्निया के विपरीत नाभि के पास वाले हर्निया में प्रारंभ में ही सर्जरी की सलाह दी जाती है। •
No categories available for this letter
Ranula / Sub glotic cyst
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
ENGLISH
Ranula / Subglotic Cyst
Ranula (Rana in Latin means frog) is a type of mucocele found on the floor of the mouth. It presents as a translucent blue swelling in the floor of the mouth. It may be small and asymptomatic, but can increase in size if not treated and interfere in swallowing.
It contains a viscous jelly like substance which is mucin from the ruptured salivary glands. A dermoid cyst may also present on the under surface of the tongue and unlike ranula, it is opaque. Surgery is curative for subglotic cyst. Incomplete removal may cause recurrence. ●
GUJARATI
જીભ નીચે ગાંઠ
બાળકનાં મોઢાંમાં તપાસ કરતાં નાની ગાંઠ જીભ નીચે જાવા મળે છે.
રેન્યુલા જીભ નીચે એક પારદર્શક ગાંઠ જેવી લાગે છે. અને તેનું થવાનું કારણ જીભ નીચે આવેલી થૂંકની ગ્રંથિનું મોઢું બંધ હોવાનું છે.
ડરમોઇડ સીસ્ટ પણ જીભ નીચે મધ્ય ભાગમાં થાય જે પારદર્શક નથી હોતી.
આવી ગાંઠોનાં કારણે બાળકને બોલવામાં અને ખાવા-પીવાની તકલીફ પડી શકે છે.
આૅપરેશન એ એક જ ઈલાજ છે અને આ આૅપરેશન જાખમ રહિત સીમ્પલ હોય છે. •
HINDI
जीभ के नीचे गांठ
रेन्युला (लेटीन भाषा में राना का अर्थ मेंढक होता है) मुँह के तल्ले पर पाया जाने वाला एक प्रकार का म्युकोसील (द्वह्वष््रूष्द्गद्यद्ग) है। यह मुँह के तल्ले पर एक पारदर्शी नीले रंग की गांठ को दर्शाता है। यह छोटा होता है, लेकिन उपचार न किए जाने पर इसका आकार बढ़ सकता है और इसके कारण खाने-पीने में परेशानी होती है।
इसमें एक चिपचिपा जेली जैसे पदार्थ होता है जो फूट पड़ने वाले लार ग्ा्रंथियों से श्लेष्मरस होता है । डर्मोइट सीस्ट भी जीभ के नीचे एक प्रकार की गांठ होती है, और यह पारदर्शी नहीं होती। सर्जरी इसका रोगनिवारक उपचार है। इसे पूरी तरह से न निकाला जाए तो यह दुबारा हो सकता है।•
Recurrent Abdominal Pain
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
RECURRENT ABDOMINAL PAIN & MESENTERIC LYMPHADENOPATHY
Recurrent abdominal pain is a common and vexing problem in children especially between 2 and 10 years. Abdominal pain which causes disturbance in sleep, school drop outs and hindrance in day to day activities of the child needs medical attention. It is mandatory to get the child checked up by a doctor and get an ultrasound scan done if necessary.
Ultrasound scan is a common and non invasive investigation which does not have any radiation exposure. It can pick up pathologies that are not visible on the outside or may not be apparent on clinical examination. One of the most common things that is picked up on ultrasound scan is enlarged mesenteric lymph nodes. The most common cause of this is intestinal infections or appendicitis. Rarely they can be due to tuberculosis or malignancy. In a well child, the size of these glands may be monitored by ultrasound scan on a monthly basis. If the size of the glands persist to 1.5 cm or larger and if there are multiple glands in the abdomen, a laparoscopic biopsy of the mesenteric lymph nodes may be helpful to arrive at a scientific diagnosis. ●
GUJARATI
પેટનો દુઃખાવો અને પેટની ગાંઠો
બાળકોમાં (ખાસ કરીને ૨ થી ૧૦ વર્ષની ઉંમરનાં બાળકોમાં) પેટનો દુઃખાવો વારંવાર થવો તે એક સામાન્ય પણ જટિલ પ્રોબ્લેમ છે.
અવારનવાર પેટમાં દુઃખાવો જેનાથી બાળકની ઊંઘ બગડતી હોય, સ્કૂલમાંથી પાછા આવવું પડતું હોય અથવા તેની રોજિંદી પ્રવૃત્તિમાં અડચણ આવે તો તેવા સંજાગોમાં બાળકની ડાક્ટરી તપાસ અનિવાર્ય બને છે. સામાન્ય તપાસમાં ચિન્હો ન જણાતાં લેબોરેટરી તપાસ અને રેડિયોલોજી ટેસ્ટ કરાવવા પડે છે.
સોનોગ્રાફી એક સામાન્ય અને હાનિરહિત તપાસ છે. પેટમાં દુઃખાવાની તપાસ દરમ્યાન આંતરડાની આજુબાજુમાં ગાંઠો હોવાનું નિદાન સોનોગ્રાફીમાં થતું હોય છે. આ થવાનું મુખ્ય કારણ આંતરડાનું ઇન્ફેક્શન અથવા એપેન્ડીક્સનો સોજા છે. ઘણીવાર ટી.બી. અને કેન્સરની શરૂઆત પણ આ ગાંઠોનું કારણ હોય છે. આવા સમયે આ ગાંઠોની સાઈઝ ૧ મહિનાનાં અંતરે બે-ત્રણ સોનોગ્રાફીની તપાસ કરાવી માપવામાં આવે છે. ૧.૫ સેમી. અથવા મોટી સાઈઝની એક થી વધુ ગાંઠો આવે તો લેપ્રોસ્કોપી દ્વારા આૅપરેશન કરી પેટની સંપૂર્ણ તપાસ થાય છે અને એક અથવા વધુ ગાંઠો કાઢી તેની બાયપ્સી દ્વારા સચોટ નિદાન કરાવવું પડે છે. ૯૦% ગાંઠો સામાન્ય ઇન્ફેક્શનના કારણે હોય છે અને તે ચિંતાનું કારણ હોતી નથી. •
HINDI
पेट दर्द एवं पेट में गाँठ
बच्चों में बार-बार पेट दर्द की शिकायत आम है, विशेष रूप से २ से १० वर्ष की आयु के बच्चों में यह समस्या रहती है। पेट दर्द के कारण बच्चे की नींद खराब होना, स्कूल से बार-बार छुट्टी लेना और बच्चे के दैनिक क्रियाकलापों में बाधा होना, इन स्थितियों में डॉक्टर से पामर्श लेना जरूरी है। आवश्यकता पड़ने पर सोनोग्राफी करानी चाहिए।
सोनोग्राफी एक समान्य और हानिरहित जाँच है जिसमें विकिरण का प्रभाव नहीं पड़ता। सोनोग्राफी करने से पेट के भीतर दर्द होने के कारण, आँतों के आसपास गाँठों के होने का पता लगाया जाता है। आँतों का इंफेक्शन या एपेन्डिक्स की सूजन इसका सबसे प्रमुख कारण है, जिसकी पहचान सोनोग्राफी से की जा सकती है। इन गाँठों के होने का कारण टी.बी या कैंसर के होने की शुरूआत भी हो सकती है। ऐसी स्थिति में एक महीने के अंतराल पर दो-तीन सोनोग्राफी से जाँच करके इन गाँठों के आकार को मापा जाता है। १.५ से.मी या उससे बड़ी आकार की एक या अधिक गाँठें होने पर लेप्रोस्कोपी करके पेट की संपूर्ण जाँच की जाती है। इसमें बायोप्सी से गाँठ के अंश को निकाल कर जाँच द्वारा रोग की पक्की पहचान की जाती है। ९०% गाँठें सामान्य इन्फेक्शन के कारण होती है, जो चिंता का विषय नहीं हैं। •
Stones (Kidney Stones)
Kidney (or renal) stones are clusters of tiny crystals that can form in the kidneys. Most clusters are too small to cause any problems and pass out of the body in the urine.
Sometimes, the clusters can clump together to form bigger clusters, which may eventually become big enough to block the filtering units in the kidney. Sometimes, they pass out of the kidney down the ureter and out in the urine without causing any problems, but if they are big they may block the ureter or lodge in the bladder.
Kidney stones are much more common in adults than in children. Children who have kidney stones will be checked thoroughly to rule out or confirm an underlying condition causing the problem. This could include a structural abnormality with the urinary system or a problem with the metabolism.
What causes kidney stones?
The urinary system consists of the kidneys, ureters, the bladder and urethra. The kidneys filter the blood to remove waste products and produce urine. The urine flows from the kidneys down through the ureters to the bladder, where it is stored until we go to the toilet. It passes through another tube called the urethra to the outside when urinating.
The kidneys contain millions of tiny filtering units called glomeruli. As blood passes through the tubes in the glomerulus, waste products pass through the walls of the tubes to form urine. Blood cells and other things such as protein cannot pass through the walls because they are too big.
The urine contains lots of different substances, which do not cause any problems when the urine is weak and the amount of each substance is balanced.
However, when the urine becomes too concentrated, often due to dehydration, the proportion of these substances in the urine increases, which can make crystals form. They can also form if the amount of these substances increases because the body is making more of them than it should or not removing them normally.
In rare situations, kidney stones can develop after urinary infections. Some children are more at risk of kidney stones, for instance, children who were born prematurely or those who have very limited mobility, such as those confined to wheelchair..
What are the signs and symptoms of kidney stones?
Some kidney stones do not cause any symptoms at all, particularly if they are very small and not causing a blockage. However, kidney stones can be painful and cause blood in the urine (haematuria) and generally feelings of being unwell, such as a high temperature and vomiting. If the stone passes out of the kidney into the ureter, it can cause severe pain.
Kidney stones can cause an infection. Signs of an infection include a high temperature, vomiting and/or diarrhoea and urine that is pink or cloudy. Studies have shown that pain is not experienced in approximately half of young children with stones.
How are kidney stones normally diagnosed?
Apart from the history which is derived from asking you questions about the problem, various imaging scans may be needed to confirm the diagnosis, see where the kidney stones are located and their size. Anultrasound scan is usually the first test to help make the diagnosis, although other scans may be needed as well. Urine tests will be needed to show whether there is an infection and to measure the chemicals that cause stones. Blood tests will show how well the kidneys are working.
How are kidney stones normally treated?
This depends on their size and location. Smaller stones can be broken up using sound waves (lithotripsy). Some stones that are stuck in the ureter can be removed using an endoscope, a tube containing a small camera, a light and a laser device to break up the stone. Most other stones are removed using surgery through a small cut. The final decision as to how to remove the stone will vary from child to child and the number and size of stone and whether there are other problems related to the kidney or its drainage system that has caused the stone to form.
Children with lots of stones or stones in both kidneys usually need several procedures to clear the stones. It is important to drink plenty of fluids to stop them forming again. Some children may need to reduce their salt intake and, rarely, other medicines or measures may be necessary.
Skull Fracture
A skull fracture is when bone in the skull has been broken by an injury or trauma. As the skull is very strong, it takes a lot of force to damage it. This might be from falling from a height, a car accident or a direct blow to the head.
What causes a skull fracture?
A skull fracture is caused by an injury or trauma to the head. A child may have fallen from a height, such as in a playground, and hit their head. Most skull fractures in children are caused when children are playing. Anyone can get a skull fracture.
There are four main types of skull fracture:
- Linear fractures are the most common. They are generally straight-forward breaks in the skull.
- Depressed fractures are where the skull has been pushed in. Surgery may be needed to lift the bone if it is putting pressure on the brain.
- Diastatic fractures are when a break occurs in more than one of the bones in the skull that are connected together. This causes the join to widen. This is usually found in young children because the bones in the skull have not fused together properly yet.
- Basilar fractures are the most uncommon and appear at the base of the skull and can risk damage to the spinal cord.
What are the signs and symptoms of a skull fracture?
If a child has hit their head, signs of a fracture include:
- a lump or dent on the head
- bruising or swelling on the head
- headache
- confusion or disorientation
- dizziness
- nausea or vomiting
- loss of consciousness
- clear fluid or blood running from the nose or ears
- bruising around the eyes (panda eyes)
How is a skull fracture normally diagnosed?
If a child has hit their head it is vital they are checked by a doctor. A head injury or skull fracture can be very serious, even if the child initially seems fine. As the skull protects the brain, a skull fracture can also cause a brain injury.
An x-ray will check for broken bones or fractures in the skull. A CT Scan looks inside the body to check the child’s brain for any signs of injury.
How is a skull fracture normally treated?
Treatment will depend on the type of skull fracture the child has and how severe it is. It can take months for a skull fracture to heal, but the younger the child is, the faster it will heal.
If the child has an open wound on their head, it will need to be cleaned to avoid infection. Medicine can be given to treat the symptoms, such as nausea and pain.
Surgery may be needed for a serious fracture if the bones have moved or if there are any fragments.
What happens next?
It is vital that all head injuries should be checked out at hospital. Most children with a simple, straightforward fracture will make a full recovery. More serious skull fractures will require treatment and maybe surgery
Small bowel atresia
The intestines form early in pregnancy as a long straight tube. Before the tenth week of pregnancy, they develop into the separate organs making up the digestive system. Occasionally, the intestines are not completely connected or blocked (atresia). Sometimes there is a partial blockage (web) inside the intestine.
Any part of the intestines can be affected by atresia or stenosis. Duodenal Atresia is one type. This occurs in around one in 6,000 births where the duodenum is closed off rather than being a tube. If the jejunum or ileum are affected, this is called ‘small bowel atresia’.
Small bowel atresia is more common than duodenal atresia. We do not know how exactly how many babies are born with small bowel atresia each year but we do know that it affects boys and girls equally. It is more common in twins or multiple births and babies born prematurely or with low birthweight.
Colonic atresia, affecting the large bowel, is very rare.
Small bowel atresia affects two areas of the small bowel – the jejunum and the ileum. The jejunum is the section of small bowel after the duodenum and is where the majority of nutrients are absorbed. The ileum is the main part of the small bowel, making up over half of its entire length, and connects to the large bowel. The blockage can affect any part of the ileum or jejunum.
What causes small bowel atresia?
More research is needed into the causes of small bowel atresia but currently doctors think that it is caused by reduced blood supply to sections of the bowel as the baby is developing in the womb. It is unlikely that it is caused by anything you did or did not do during pregnancy.
What are the signs and symptoms of small bowel atresia?
Many babies born with small bowel atresia appear well at birth but when they start to feed, they start to have nausea and vomiting and their vomit may be green. Their abdomen may appear swollen but soft and their skin may develop a yellow tinge (jaundice).
All newborn babies have meconium in their bowel. This is the dark green stool passed in the first day of life. Babies born with small bowel atresia may not pass any meconium at all or only a small amount. Not passing meconium does not prove that a baby has small bowel atresia but it may suggest it. Some babies with small bowel atresia pass meconium as expected.
How is small bowel atresia diagnosed?
When a baby with small bowel atresia is developing in the womb, they are may be surrounded by much more amniotic fluid than usual (polyhydramnios). Small bowel atresia can sometimes be suggested during pregnancy using an ultrasound scan.
After the baby is born, small bowel atresia is usually diagnosed when there are signs of an obstruction, such as vomiting, green bile and a swollen abdomen. An x-ray scan may show a blockage. Occasionally, doctors may suggest using a contrast scan and/or enema instead or as well as an x-ray.
Contrast scans and enemas use a thick, white liquid called barium or a clear liquid (contrast), both of which show up well on x-rays. The contrast cannot pass through the atresia suggests that atresia can be a cause.
How can small bowel atresia be treated?
Small bowel atresia is repaired in an operation under general anaesthetic. The operation to repair the atresia can is usually carried out using open surgery. Sometimes a laparoscopic surgery (key hole procedure) may help diagnose the problem so that it can be repaired using open surgery.
Are there any alternatives?
No. Small bowel atresia always requires surgical treatment to allow your baby to feed.
What happens before the operation?
Your baby will be transferred to the hospital soon after birth.
If your child is dehydrated, they will need a ‘drip’ of fluids for a while before the operation. Your child will also need a nasogastric tube, which is passed up the nose, down the foodpipe and into the stomach. This will drain off the stomach and bowel contents and ‘vent’ any air that has built up, which will make your child more comfortable.
When your child is stable, the surgeon will explain about the operation in more detail. Sometimes the atresia is suspected but may not be the only possible cause of the blockage. The surgeon will explain this to you.
What does the operation involve?
The surgeon will look at the bowel to determine the level of the blockage. If it is an atresia, this section is removed and the cut ends are joined together (anastomosis). This provides a clear passage for food and fluid to travel through your child’s intestine. The remainder of the small intestine will be checked for further atresias and treated if identified.
If it is not possible or safe to join the two ends together during the same procedure, the surgeon may bring the end of the intestine to an artificial opening (stoma) in the abdomen to form an ileostomy.
Are there any risks?
All surgery carries a small risk of bleeding during or after the operation. There is a chance that the area where the two ends of bowel were joined could start to leak, allowing bowel contents to escape into the abdomen. This is usually treated with antibiotics, but a second operation may be needed to check the leaking portion.
All abdominal surgery carries the risk of strictures forming. These are areas of scar tissue that can narrow the intestines, leading to obstruction. If your child vomits green bile and has a swollen abdomen, they should be reviewed urgently by a doctor.
It can take a while after the operation for the bowel to start working properly so your child may need to be fed intravenously using total parenteral nutrition (TPN) for a while. This affects many children.
What happens after the operation?
While your child’s intestines recover and start to work, they may be fed through a tube into their veins (total parenteral nutrition or TPN). This will gradually be replaced by breast or bottled milk, given through the naso-gastric tube when your child is able to tolerate this. As your baby recovers, you will be able to feed them from the breast or bottle. Over time, the drips and monitors will be removed one by one.Most children stay in hospital for one to two weeks, but occasionally a longer stay is needed.
What happens next?
The outlook depends on the amount of damage to the bowel. Adhesions can form after any abdominal surgery and can cause further problems such as blockage or pain. This however is quite rare and may sometimes require another operation to separate the adhesions.
Syndactyly (Joined fingers / toes) & Polydactyly
INFORMATION AVAILABLE IN ENGLISH , GUJARATI AND HINDI
Syndactyly :
Syndactyly means ‘joined digits’ and may involve webbing of the skin, or include fusion of the underlying bones. This may be along part or the whole length of the finger. It is the second most common congenital hand problem and occurs in around 1 in 1000 births.
Hand development occurs in the early stages of pregnancy and the fingers separate in the ninth week. Syndactyly happens when two or more fingers fail to completely separate during development.
Sometimes syndactyly occurs by chance or it may be inherited. In rare circumstances, it may occur along with other signs as part of a syndrome (collection of signs).
Syndactyly can occur unilaterally (on one hand only) or bilaterally (affecting both hands), and can affect two or more fingers. Occasionally it may be associated with extra digits or other abnormalities in the hands.
Syndactyly can also affect the toes, involving webbing of the skin or fusion of the underlying bones along part or the whole length of the toe.
How is syndactyly treated?
It is treated surgically under a general anaesthetic. Surgery is usually only possible to one side of a finger at a time, as any damage to the blood supply on both sides could result in the loss of the finger. So, if your child has syndactyly of three or more digits next to each other, they will need more than one operation.
Are there any alternatives to surgery?
Surgery is the only option to separate the digits. The aim of the operation is to improve function (how well your child can use their hand) and sometimes appearance (how your child’s hand looks).
Occasionally, some children could manage without treatment. Correction of toe syndactyly is usually for cosmetic rather than functional reasons.
What does the operation involve?
The surgeon will recreate a new web with local flaps of skin from the sides of the digits. This usually involves making a series of zig-zag incisions along the digits, and wrapping the zig-zag pieces of skin to cover up the inside surface of the digits where they were previously joined.
In most cases, the surgeon will need to use a skin graft to cover up any gaps. This will be a different colour on the hand than the rest of the skin. Occasionally, a skin graft will not be needed.
Are there any risks?
There is a risk of infection as the skin is opened, but your child will be given antibiotics to reduce the risk of this. If an infection does occur, it is usually minor and easily treated with a course of antibiotics.There is a chance that the skin graft will not ‘take’, but looking after it carefully will help the operation site to heal as well as possible. Any infection or graft loss may affect the time the wounds take to heal and therefore the resulting scars.
The amount of scarring varies from child to child. If your child tends to scar easily from cuts and grazes, it is likely that they will have noticeable scars after the operation, but these will fade in time.
What happens after the operation?
Their hand or foot will be covered in a large bandage to protect the skin grafts while they heal. Your child will soon find a way to use their bandaged hand or foot in everyday activities. It is best to keep the limb operated on raised above the level of the heart as much as possible to reduce any swelling, which in turn reduces any pain.It also minimises any oozing under the flaps and skin grafts. Your child’s limb may be raised using pillows or soft toys, or the hand may be placed in a sling when sitting or walking around.If your child’s fingertips or toes are visible, check them on a regular basis for warmth, colour, sensation, movement and blood flow. These checks show that the blood is flowing properly.
What is the outlook for children with syndactyly?
This depends on the degree of syndactyly and whether it occurred by chance or as part of a syndrome. The outlook for children with simple syndactyly is usually excellent. If the syndactyly occurred as part of a syndrome, the outlook depends on the particular syndrome and associated features.
Polydactyly:
Polydactyly is a condition where the child has supernumary fingers or toes. It can present in either one or both hands and / or feet. Most of the times the extra digit is usually a piece of soft tissue on a tiny stalk. Sometimes, it may contain bone without joints and rarely it may be a complete functioning digit.
Surgery for polydactyly is recommended between 1 – 1 1/2 years of age. A rudimentary accesory digit may sometimes undergo torsion needing an emergency surgery. ●
GUJARATI
બાળકની આંગળીઓની ખોડ
બાળકનાં હાથ અને પગની આંગળીઓમાં ઘણી ખોડ જાવા મળે છે. જા એક-બે આંગળીઓની ખોડ હોય તો સર્જરીનાં રીઝલ્ટ સારા આવે છે પણ ઘણી વખત હાથ કે પગની આંગળીઓની સાથે તેમાં રહેલાં હાડકાં પણ ખોડ વાળા હોય તો બાળક આ ખોડ સાથે સારું કામ કરી શકે તેવી સર્જરી કરવામાં આવે છે. આમાં સંપૂર્ણ નોર્મલ દેખાય તેવાં હાથ નથી કરી શકાતા.
આ ખોડ ૧ ૧/૨ વર્ષની આસપાસ આૅપરેશન દ્વારા છૂટી કરી શકાય છે.
હાથ કે પગમાં પાંચ આંગળીઓ કરતાં વધુ હોય તો તેને પોલીડેક્ટલી કહેવામાં આવે છે. સામાન્ય રીતે એક્સ્ટ્રા આંગળીઓ કાઢવાની સર્જરી ૧ વર્ષ પછી કરાવવી, પણ જા એક્સ્ટ્રા આંગળી ફક્ત ચામડીથી જાડાયેલી હોય અને તેમાં વળ ખાઈ ગેંગરીન થાય છે તો તે માટે તાત્કાલિક આૅપરેશન કરાવવું પડે છે. •
HINDI
बच्चों की अंगुलियों की विसंगति
सींडेक्टली अर्थात ‘जुड़ी हुई अंगुलियाँ’ वह स्थिति है जब बच्चे के विकास के दौरान दो या दो से अधिक अंगुलिया पूरी तरह से अलग नहीं हो पाती है। कभी-कभी कुछ बच्चे बिना किसी उपचार के भी कार्य कर सकते है। पैर के अंगूठे के सिंडेक्टिली का उपचार आमतौर पर कार्यात्मक कारणों से अधिक कॉस्मेटिक कारणों से किया जाता है (ताकि बच्चा चप्पल/स्लीपर पहन सके)। सर्जरी के लिए कभी-कभी त्वचा निरोपन की आवश्यकता पड़ती है।
पॉलीडेक्टीलीमें बच्चे को अतिरिक्त अंगुलियाँ अथवा अंगूठे होते हैं। यह एक या दोनों हाथ अथवा पांव में हो सकती है। अधिकतर मामलों में ये अतिरिक्त अंगुलियाँ छोटे से डंठल पर नर्म मांस-तंतु के समान होती हैं। कभी-कभी इनमें बिना किसी जोड़ के हड्डी होती है; और यह शायद ही कभी पूर्णतया कार्यशील अंगुली के रूप में होती है। सींडेक्टली के लिए सर्जरी १भ वर्ष की आयु होने पर की जाती है। अतिरिक्त अंगुली केवल त्वचा से जुड़ी हो और इसमें मरोड़ उत्पन्न हो जाए तो यह एक आपात स्थिति पैदा कर सकती है। •
Sacrococcygeal Teratoma
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
SACROCOCCYGEAL TERATOMA
Sacrococcygeal teratoma (SCT) is a tumor that develops at the base of the coccyx (tail bone). It is seen in 1 in 35000 live births. Almost 75 % of SCT’s are benign, especially before the age of 5 months. These can be picked up on prenatal ultrasound scans. It can be of a small size like an orange but can grow to almost the size of a small water melon. They can be partly external and party internal.
The treatment for SCT is surgical removal. This is commonly done through the back. However, for large tumors or tumors with pelvic extension, opening the abdomen may be required. ●
GUJARATI
સેક્રોકોક્સીજિયલ ટેરાટોમા
આ એક જન્મજાત ખોડ છે. બાળકનાં જન્મ પહેલાં માતાની સોનોગ્રાફી કરાવવાથી ડિલિવરી પહેલા તેનુંં નિદાન થઈ શકે છે.
આવી ગાંઠ સંડાસની જગ્યાથી પાછળ અને પૂંછડીનાં છેલ્લાં હાડકાં સાથે જાડાયેલી હોય છે. તેનો આકાર નાની નારંગી જેવો અથવા મોટા તડબૂચ જેવો હોઈ શકે છે. ગાંઠ વધુ મોટી હોય તો નોર્મલ ડિલિવરી કરાવવા કરતાં સિઝેરિયન કરાવવું વધુ સારું છે.
આ ગાંઠ મોટી દેખાય છે પણ ૯૦% ઉપરનાં બાળકોમાં તે તદ્દન નિર્દોષ (કેન્સર નહીં) હોય છે. આ ગાંઠ સહેલાઈથી આૅપરેશન દ્વારા કાઢી શકાય છે અને બાળકોને કોઈ ખોડ-ખાંપણ રહેતી નથી. બાયોપ્સી અચૂક કરાવવી હિતાવહ છે.
આૅપરેશન બાળક ૧ મહિનાનું થાય ત્યાર પહેલાં કરાવવું, જેથી તેમાં કોઇ કોમ્પ્લીકેશન થાય નહીં. •
HINDI
पीठ के नीचे जन्मजात गांठ ( Sacrococcygeal टेराटोमा)
पीठ के नीचे गांठ (Sacrococcygeal टेराटोमा) का होना एक जन्मजात दोष है जिसकी पहचान प्रसूति से पहले माता की सोनोग्राफी कराने से की जा सकती है। यह गांठ पीठ के सबसे नीचे की हड्डी के साथ जुड़ी हुई होती है और ३५००० में से १ बच्चे में यह दोष देखा जाता है। शुरूआत में यह गांठ नारंगी के आकार की और धीरे-धीरे बढ़कर छोटे तरबूज के आकार की हो सकती है, जो आधी शरीर के भीतर और आधी बाहर होती है।
यह गांठ भले ही बड़ी दिखाई देती है, लेकिन इस समस्या वाले ९०% बच्चों में कैंसर नहीं होता और कुशलतापूर्वक ऑपरेशन से इस गांठ को निकाला जा सकता है। नवजात बच्चे के एक महीने का होने से पहले यह ऑपरेशन करा लेना चाहिए, जिससे बालक को आगे कोई तकलीफ न हो। •
Sub Glotic Cyst / Ranula
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
ENGLISH
Ranula / Subglotic Cyst
Ranula (Rana in Latin means frog) is a type of mucocele found on the floor of the mouth. It presents as a translucent blue swelling in the floor of the mouth. It may be small and asymptomatic, but can increase in size if not treated and interfere in swallowing.
It contains a viscous jelly like substance which is mucin from the ruptured salivary glands. A dermoid cyst may also present on the under surface of the tongue and unlike ranula, it is opaque. Surgery is curative for subglotic cyst. Incomplete removal may cause recurrence. ●
GUJARATI
જીભ નીચે ગાંઠ
બાળકનાં મોઢાંમાં તપાસ કરતાં નાની ગાંઠ જીભ નીચે જાવા મળે છે.
રેન્યુલા જીભ નીચે એક પારદર્શક ગાંઠ જેવી લાગે છે. અને તેનું થવાનું કારણ જીભ નીચે આવેલી થૂંકની ગ્રંથિનું મોઢું બંધ હોવાનું છે.
ડરમોઇડ સીસ્ટ પણ જીભ નીચે મધ્ય ભાગમાં થાય જે પારદર્શક નથી હોતી.
આવી ગાંઠોનાં કારણે બાળકને બોલવામાં અને ખાવા-પીવાની તકલીફ પડી શકે છે.
આૅપરેશન એ એક જ ઈલાજ છે અને આ આૅપરેશન જાખમ રહિત સીમ્પલ હોય છે. •
HINDI
जीभ के नीचे गांठ
रेन्युला (लेटीन भाषा में राना का अर्थ मेंढक होता है) मुँह के तल्ले पर पाया जाने वाला एक प्रकार का म्युकोसील (द्वह्वष््रूष्द्गद्यद्ग) है। यह मुँह के तल्ले पर एक पारदर्शी नीले रंग की गांठ को दर्शाता है। यह छोटा होता है, लेकिन उपचार न किए जाने पर इसका आकार बढ़ सकता है और इसके कारण खाने-पीने में परेशानी होती है।
इसमें एक चिपचिपा जेली जैसे पदार्थ होता है जो फूट पड़ने वाले लार ग्ा्रंथियों से श्लेष्मरस होता है । डर्मोइट सीस्ट भी जीभ के नीचे एक प्रकार की गांठ होती है, और यह पारदर्शी नहीं होती। सर्जरी इसका रोगनिवारक उपचार है। इसे पूरी तरह से न निकाला जाए तो यह दुबारा हो सकता है।•
Swellings in Neck / Neck Swellings
INFORMATION ALSO AVAILABLE IN ENGLISH, GUJARATI AND HINDI
There are two types of swellings in the neck:
Congenital Swellings (Since Birth):
a) Tyroglossal Cyst: This swelling occurs in the midline of the neck and is due to a developmental defect during the formation of the thyroid gland. Surgery is a must for this swelling.
 Thyroglossal Cyst
Thyroglossal Cyst
b) Dermoid Cyst: This swelling also happens in the midline of the neck. They are also seen at many other sites in the body. Surgery is also required for these swellings.
 Dermoid Cyst
Dermoid Cyst
c) Cystic Hygroma: These swellings occur as a result of a developmental anomaly of the lymphatics. They look like cysts filled with water and are commonly seen in any part of the neck. They can vary from being very small to massive in size. Surgery is curative for these swellings.
 Cystic Hygroma in the neck
Cystic Hygroma in the neck
d) Branchial cyst: These swellings are found on the side of the neck. They are sometimes also seen like a small punctum which is called a Branchial Sinus
 Branchial Cyst in the neck
Branchial Cyst in the neck
e) Cervical Meningocele: These swellings are seen behind the neck in the midline. They are present since birth and surgery is curative.
 Cervical Meningomyelocele
Cervical Meningomyelocele
Acquired Swellings (After Birth) :
a) Lymph nodes: They can be single or multiple. They may be seen over different sites in the neck. Common cause of lymph node enlargement is secondary to an infective process in the head and neck region.


b) Tuberculous nodes (Koch’s nodes): Tuberculous nodes are not uncommon. A confirmed diagnosis can be acheived by biopsy of the node. Regular medications can almost always cure this problem.

c) Malignant nodes (Cancers): The most commonly seen malignant nodes in the neck in children are lymphomas. Confirmation of diagnosis can be done by biopsy of the nodes. Regular chemotherapy can be curative in most of these cases.
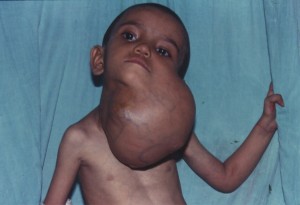
Lymph Glands in the Neck:
Everyone has lymph glands. They are in many areas of the body, including the neck, under the arms and in the groin (at the top of each leg). There are also lymph glands in the abdomen, chest and pelvis. Lymph glands are also known as lymph nodes.
Lymph glands become enlarged when the body is fighting an infection, such as a cold. Enlarged lymph glands are particularly common in children as their body takes time to build up immunity to infection.
What causes swollen lymph glands?
Lymph glands swell as part of the body’s response to infection.
Lymph glands are connected by vessels with branches right through the body, similar to the blood circulation system. Rather than carrying blood, these vessels carry a clear liquid called lymph, which contains a high number of white blood cells.
Together with other organs (the spleen, tonsils, adenoids and thymus gland), they form what’s known as the lymphatic system. It has several functions but one of its key roles is fighting infection.
When the body is fighting an infection, the number of white blood cells multiplies rapidly. Some of these cells will go to the lymph gland nearest the infection, which produces enlargement of the lymph glands.
Children often have infections as it takes time for them to build immunity to the viruses and bacteria in the environment. Children who have recently started playgroup or nursery are especially prone because they are coming into contact with a large group of children of the first time.
What are the signs and symptoms of enlarged lymph glands?
The lymph glands will appear swollen. They will also be uncomfortable.
Children frequently get upper respiratory tract infections, such as an ear or throat infection. This means that swollen glands in the neck are particularly common.
How are enlarged lymph glands normally diagnosed?
A child’s doctor will feel their glands to check if they are swollen.
How are enlarged lymph glands treated?
Most cases of enlarged lymph glands are from infection. Once the infection is gone, the glands will get smaller and less tender over time.
If the glands are particularly large, the doctor will check the child for any other symptoms or an underlying cause.
What happens next?
In most cases, enlarged lymph glands are not serious and the condition is common. Following an infection, it is normal for them to take some time for the swelling to go down.
Enlarged lymph glands rarely indicate a more serious problem. Sometimes it is a sign of cancer, such as lymphoma, but this is rare.
GUJARATI
ગળામાં થતી ગાંઠો
ગળામાં થતી ગાંઠો બે પ્રકારની હોય છેઃ
૧. જન્મ જાત ગાંઠઃ
૧) થાઇરોગ્લોસલ સીસ્ટ : ગળાનાં મધ્ય ભાગમાં થતી ગાંઠ થાયરોઇડ ગ્રંથિની ડેવલપમેન્ટની ક્ષતિના કારણે થાય છે. આૅપરેશન કરવાથી જ મટે છે.
૨) ડરમોઈડ સીસ્ટ : આ પણ ગળાનાં મધ્યભાગમાં થતી ગાંઠ છે. જે ઓપરેશનથી મટે છે.
૩) સીસ્ટીક હાઇગ્રોમા : લીમ્ફેટીક નળીઓની બનાવટની ખામીના કારણે, પાણી ભરેલી ગાંઠ ગળામાં ગમે તે જગ્યાએ થાય છે. આવી ગાંઠ સાઈઝમાં નાની અથવા આત્યંત મોટી હોય છે. યોગ્ય સમયે ઓપરેશન કરાવવું જરૂરી છે.
૪) બ્રેન્કયલ સીસ્ટ : આ ગાંઠ ગળાની સાઈડમાં જાવા મળતી હોય છે. ધણીવાર તે નાના છિદ્રનાં રૂપમાં હોય છે. (જેને સાઇનસ કહે છે.)
૫) સરવાઇકલ મેનીન્ગોમાઇલોસીલ : ગળાની પાછળ બરાબર કરોડના મણકા પર થતી જન્મજાત ગાંઠ છે અને આૅપરેશન કરવાથી સંપૂર્ણ સા૨ું થઈ જાય છે.
૨. જન્મ પછી થતી ગળાની ગાંઠો :
૧) લીમ્ફનોડની ગાંઠ : આ ગાંઠ ગળામાં જાવા મળે છે અને તે એક કરતા વધુની સંખ્યામાં અને જુદી જુદી જગ્યાએ પણ હોય છે.
લીમ્ફગ્લેન્ડ – માથા, નાક, કાન, ગળામાં થતા ઇન્ફેક્શનની વેડ ઘાલવાથી થાય છે અને બરાબર દવા કરવાથી મટે છે.
૨) ટી.બી.ની ગાંઠ : ગળામાં ટી.બી.ની ગાંઠ ૧/૨ણી સામાન્ય બીમારી છે. ચોક્કસ નિદાન બાયોપ્સી દ્બા૨ા કરાવી યોગ્ય દવાઓ આપવાથી મટી જાય છે.
૩) કેન્સરની ગાંઠ : બાળકોમાં ગળામાં લીમ્ફોમા નામના કેન્સરને લીધે ગાંઠ થતી હોય છે. તેનું જરૂરી નિદાન બાયોપ્સી વડે કરાવી, દવાઓથી મટાડી શકાય છે. •
HINDI
गले की गांठे
१. जन्मजात गांठ
१) थाइरोग्लोसल सीस्टः गले के मध्य भाग में होनेवाली यह गांठ थाइरोइड ग्ा्रंथी के दोषपूर्ण विकास के कारण होती है और यह केवल ऑपरेशन के द्वारा ही ठीक की जा सकती है।
२) डरमोइड सीस्टः यह भी गले के मध्य भाग में होनेवाली एक गांठ है जो ऑपरेशन के द्वारा ही ठीक की जा सकती है।
३) सीस्टिक हाइग्ा्रोमाः लीम्फेटिक नलिकाओं की बनावट में दोष के कारण, पानी भरी एक गांठ गले के भीतर कहीं भी हो सकती है। यह गांठ आकार में या तो अत्यंत छोटी होती है या अत्यंत बड़ी होती है। उचित समय पर इसका ऑपरेशन कराना आवश्यक है।
४) ब्रेंकीयल सीस्टः यह गले के एक ओर दिखाई देनेबाली गांठ है। कई बार यह एक छोटे से छेद के रूप में होती है (जिसे साइनस कहते हैं)।
५) सरवाइकल मेनींगोमाइलोसीलः गरदन के पिछले हिस्से में ठीक रीढ़ पर होनेवाली जन्मजात गांठ होती है और ऑपरेशन के द्वारा पूर्णरूप से ठीक हो जाती है।
२. जन्म के बाद होनेवाली गले की गांठ
१) लीम्फनोड की गांठः इस प्रकार की गांठ गले के एक ओर देखी जा सकती है।
२) टी.बी. की गांठः गले में टी.बी. की गांठ होना एक सामान्य बीमारी है। सही निदान, बायोप्सी के उपरांत उचित दवाइयों से ठीक हो जाती है।
३) कैंसर की गांठः यह बच्चों के गले में लीम्फोमा नामक कैंसर के कारण होनेवाली गांठ है। इसे आवश्यक निदान, बायोप्सी तथा उचित दवाइयों से ठीक किया जा सकता है।•
Tonsils and Adenoids
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
The tonsils are areas of tissue on both sides of the throat, at the back of the mouth. Your child’s tonsils help them to build up immunity and fight infection. In many children, the tonsils become repeatedly infected with bacteria and viruses, which make them swell and become painful. This is called tonsillitis.
What causes tonsillitis?
Tonsillitis is the word used when the tonsils are infected so swell and become painful. Both bacteria and viruses can cause an infection – these are usually picked up as part of everyday life so there is little you can do to prevent them although good hygiene including hand washing is important.
What are the signs and symptoms of tonsillitis?
The main symptom of tonsillitis is a sore throat, which is particularly painful when swallowing. Your child may complain of earache as well.
The tonsils may also have a white covering or spots, which are a sign that the body is fighting off the infection. Your child’s neck may look a little swollen as well, and they may have a temperature.
How is tonsillitis diagnosed?
Tonsillitis can be diagnosed by looking closely in the mouth, sometimes using a small torch to look at the back of the mouth.

 Acute Tonsillitis with pus
Acute Tonsillitis with pus
How is tonsillitis treated?
Pain relief medicines, such as paracetamol and ibuprofen can help reduce the pain and also bring down a temperature. If the infection was caused by a bacteria, the child will require antibiotics. Most cases of tonsillitis disappear within a few days.
If your child has repeated bouts of tonsillitis, we may suggest an operation to remove the tonsils.
SURGERY FOR TONSILLS AND ADENOIDS
The tonsils and adenoids are areas of tissue at the back of the throat. The tonsils are on both sides of the throat, at the back of the mouth, and are clearly visible. Adenoids are not visible, as they are high in the throat behind the nose.
Your child’s tonsils and adenoids help him or her to build up immunity and fight infection. Adenoids and tonsils seem to grow during childhood and then shrink around the age of four. By the time your child reaches adulthood, his or her adenoids and tonsils will have disappeared almost completely. This is because they are no longer needed, as your child’s body will have other defence mechanisms to fight against infection.
Why do tonsils have to be removed?
In many children, the tonsils become repeatedly infected with bacteria and viruses, which make them swell and become painful. Removing your child’s tonsils and adenoids will solve these problems.
Your child may have larger than average tonsils and adenoids, which partially block his or her airway. This can make it difficult for them to breathe through their nose. As a result, your child may breathe through their mouth and snore loudly when asleep. This can lead to a condition called sleep apnoea, where your child stops breathing for a couple of seconds while asleep and then starts again. This can severely disturb their sleep.
There is also a link between large tonsils and adenoids and a condition called glue ear. This happens when the middle ear becomes blocked by a sticky substance which affects your child’s hearing.
What are the risks of this operation?
Every operation carries some risk of infection but we will often give your child antibiotics as a precaution.
The risk of bleeding is usually greatest in the first few days after this operation. It is rarely serious.
Are there any alternatives to this operation?
If your child is having difficulties in breathing or has developed glue ear, it is probably better to have his or her tonsils and adenoids removed.
When your child gets home
Your child will probably feel uncomfortable for a week after the operation and may find swallowing difficult. They may also be reluctant to eat certain foods or brush their teeth.
GUJARATI
ટોન્સીલ :
ગળામાં જીભની પાછળ ડાબી અને જમણી બાજુ ટોન્સીલ(કાકડાં) આવેલાં હોય છે. બાળકોમાં ટોન્સીલનું ઇન્ફેક્શન સામાન્ય છે અને યોગ્ય એÂન્ટબાયોટીકથી મટાડી શકાય છે. વારંવાર ટોન્સીલમાં ઇન્ફેક્શનથી બાળકોની તંદુરસ્તી જાખમાતી હોય તો આૅપરેશન કરવાવું જરૂરી થાય છે, જે સામાન્ય રીતે બાળક ૪ વર્ષનું થાય પછી કરાવવું.
એડીનોઇડસ :
એડીનોઇડસ(નાકની પાછળના મસા) પણ નાના-નાના ટોન્સીલ જ છે જે નાકની પાછળમાં થતા હોય છે. તેમાં વારંવાર ઇન્ફેક્શન થવાથી તે મોટા થાય છે, જેથી બાળકને નાકથી શ્વાસ લેવાતો નથી. બાળક મોઢું ખુલ્લું રાખી શ્વાસ લે છે અને રાત્રે ઊંઘમાં નસકોરાં બોલાવે છે. આથી બાળકને મોઢાંમાંથી વાસ પણ આવે. એડીનોઇડ્સનું આૅપરેશન ૨ વર્ષ પછી કરાવી શકાય. ઘણીવાર આ આૅપરેશન કાકડા સાથે પણ કરવામાં આવે છે. •
HINDI
टॉन्सिल और एडीनोइड्स
टॉन्सिल, गले के भीतर जीभ के पीछे दाई और बाई ओर होता हैं। बच्चों में टॉन्सिल का संक्रमण एक आम बात है और उचित एंटीबायोटिक से इसे ठीक किया जा सकता है। लेकिन बार-बार टॉन्सिल के संक्रमण के कारण यदि बच्चे के स्वास्थ में जोखिम हो तो ऑपरेशन कराना आवश्यक हो जाता है। सामान्यतः यह ऑपरेशन बच्चे के ४ वर्ष का हो जाने के बाद किया जाना चाहिए।
एडीनोइड्स – नाक के पीछे छोटे-छोटे टॉन्सिल या एक प्रकार का मसा है। इनमें बार-बार संक्रमण होने पर यह बड़े हो जाते है। इस कारण बच्चा नाक के द्वारा श्वास नहीं ले सकता है। बच्चा मुँह खोलकर श्वास लेता है और रात में नींद में खर्राटें भरता है। इस कारण बच्चे के मुँह से दुर्गंध भी आती है। एडीनोइड्स का ऑपरेशन २ वर्ष की आयु के बाद किया जा सकता है। कई बार यह ऑपरेशन टॉन्सिल के साथ किया जाता है। •
Tongue Tie
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
TONGUE TIE
Tongue tie is a common problem seen in many children where the tongue is tied by a band to the floor of the oral cavity. This causes the tongue to fork (like that of a frog) when the child protrudes its tongue. Tongue tie may cause problems in pronunciation of certain letters which need the tongue to touch the palate.
Release of tongue tie is a simple procedure which involves division of the band under the tongue. This is a short procedure and the child is discharged from the hospital in a few hours. The surgery does not have any implications in the child’s food habits. ●



 Tongue Tie
Tongue Tie
GUJARATI
જીભ નીચે તાર
ઘણાં બાળકોમાં જીભ નીચે તાર જાવા મળે છે. આ એક જન્મજાત ખોડ છે જેમાં જીભ જડબાનાં નીચેનાં ભાગ સાથે બંધાયેલી રહે છે. આ ખોડના કારણે બાળક જ્યારે જીભ બહાર કાઢે ત્યારે દેડકાની જેમ જીભ ફંટાયેલી જાવા મળે છે જેને અંગ્રેજીમાં ફોરકીંગ આૅફ ટંગ કહેવામાં આવે છે. આ ખોડથી બાળકને ‘થ’, ‘ટ’,‘ડ’, ‘ર’ અને ‘ત’ ના અક્ષરો બોલવામાં તકલીફ પડતી હોય છે. આ ખોડના કારણે ઘણીવાર બાળકને ઝડપથી બોલવામાં પણ તકલીફ પડતી હોય છે. આ ખોડનું નિવારણ કરવા માટે લેસરથી જીભ નીચે બંધાયેલો તાર છૂટો કરવામાં આવે છે. આ એક ખૂબ જ સામાન્ય આૅપરેશન છે અને બાળકને ત્રણ થી ચાર કલાકમાં હાÂસ્પટલમાંથી રજા આપી દેવામાં આવે છે. બાળક આૅપરેશનના દિવસથી જ ખાતું-પીતું થઈ જાય છે અને પોતાની સામાન્ય ક્રિયાઓ કરી શકે છે. આૅપરેશન બાળક નાનું હોય ત્યારે કરાવવું જાઇએ. •
HINDI
जीभ टाई/जिह्वा बद्धता
जीभ टाई बच्चों में पाई जानेवाली एक सामान्य समस्या है, जिसमें यह देखा गया है कि जीभ मौखिक गुहा के तल पर एक तार से बंधी हुई होती है। इस कारण जब बच्चा अपनी जीभ फैलाता है तब वह एक काँटे (मेंढक की तरह) की भांति दिखाई देती है। जीभ टाई के कारण ऐसे कुछ शब्दों के उच्चारण में समस्याएं पैदा हो सकती है जिनमें जीभ्ा तालु को स्पर्श करती है।
जीभ टाई को खोलना एक सरल प्रक्रिया है जिसमें जीभ को नीचे के तार से अलग किया जाता है। यह एक अल्पकालीन प्रक्रिया है, जिसके बाद बच्चे को अस्पताल से कुछ ही घंटो में छुट्टी दी जाती है। इस सर्जरी से बच्चे के भोजन की आदतों में कोई प्रभाव नहीं पड़ता। •
Thyroglossal Cyst & Thyroglossal Sinus
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Thyroglossal Cyst and Thyroglossal Sinus
Thyroglossal Cyst occurs in the midline of the neck due to a developmental defect during the formation of the thyroid gland. Diagnosis is easy. However, ultrasound scan is required to document the presence of a normal thyroid gland. Surgery is a must for this swelling. However, inadequately excised swellings may cause recurrence.
Sometimes, the child may present with just a tiny hole in the midline of the neck with watery or whitish discharge. This is called a thyroglossal sinus which like the thyroglossal cyst is also an embryological remnant. Surgery is the cure for a thyroglossal sinus. ●


 Thyroglossal Cyst
Thyroglossal Cyst

 Thyroglossal Sinus
Thyroglossal Sinus
 Thyroglossal Sinus (operative photo)
Thyroglossal Sinus (operative photo)
GUJARATI
થાઈરોગ્લોસલ સીસ્ટ અને થાઈરોગ્લોસલ સાયનસ
થાઈરોગ્લોસલ સીસ્ટ બાળકના ગળાની વચ્ચોવચ જાવામાં આવતી ગાંઠ છે. આ ગાંઠને કંઠમાળની નોર્મલ ગાંઠ સમજીને ઘણીવાર સારવારમાં વિલંબ થતો હોય છે. બાળક જ્યારે માના ગર્ભમાં હોય ત્યારે ગળામાં આવેલી થાઇરોડ ગ્રંથિ જીભની નીચેથી ઉદ્ભવીને ગળામાં તેની યોગ્ય જગ્યાએ જતી હોય છે. આ પ્રક્રિયા દરમિયાન થાઇરોડ ગ્રંથિના અમુક કોષ પાછળ છૂટી જતાં હોય છે. આ કોષ આગળ જતાં થાઈરોગ્લોસલ સીસ્ટ બનાવતા હોય છે. આ ગાંઠનું નિદાન ખૂબ જ સરળ હોય છે, અને સોનોગ્રાફીમાં પણ આ ગાંઠ તરતજ દેખાઈ જતી હોય છે. સારવાર માટે આ ગાંઠનું આૅપરેશન કરી સંપૂર્ણપણે કાઢી નાખવી જરૂરી છે. જા આ ગાંઠ અને તેની સાથે રહેલા વધારાના કોષ કે માર્ગને આૅપરેશન દરમ્યાન દૂર કરવામાં ન આવે તો આ ગાંઠ ફરી થવાની શક્યતા રહે છે. ઘણીવીર થાઇરોડના આ રહી ગયેલા કોષ ગાંઠ ન બનાવતા ગળાની બરોબર વચ્ચે નાનું કાણું/છીદ્રની ખોડ કરે છે. આ ખોડને થાઈરોગ્લોસલ સાયનસ તરીકે ઓળખવામાં આવે છે. થાઈરોગ્લોસલ સાયનસમાંથી થોડા થોડા સમયે સફેદ ચીકાણું પ્રવાહી નીકળે છે. જા ઇન્ફેક્શન થાય તો આ સાયનસ અને ગાંઠ બંનેમાં પરૂ થવાની શક્યતા પણ રહેલી છે. થાઈરોગ્લોસલ સાયનસની સારવાર પણ થાઈરોગ્લોસલ સીસ્ટની જેમ જ આૅપરેશન દ્વારા કરવામાં આવે છે. થાઈરોગ્લોસલ સીસ્ટની માફક જ અધૂરા કે અપૂરતા આૅપરેશનથી થાઈરોગ્લોસલ સાયનસ ફરી થવાની શક્યતા રહે છે. •
HINDI
थाइरोग्लोसल सिस्ट और थाइरोग्लोसल सायनस
थाइरोग्लोसल सिस्ट बच्चे के गले के बीचोबीच पाई जाने वाली एक गांठ है। इस गांठ को कई बार कंठमाला की गांठ समझकर उपचार में देरी हो जाती है। बच्चा जब गर्भ में होता है तब गले में स्थित थाइरोड ग्ा्रंथी जीभ के नीचे से होकर उचित स्थान पर चली जाती है। इस प्रक्रिया के दौरान थाइरोड ग्ा्रंथी की कुछ कोशिकाएं पीछे छूट जाती है। ये कोशिकाएं आगे चलकर थाइरोग्लोसल सीस्ट में परिवर्तित हो जाती है। इस गांठ का निदान बहुत ही सरल है और सोनोग्ा्राफी के माध्यम से इसका पता लगाया जा सकता है। ऑपरेशन के द्वारा इस गांठ को पूरी तरह से हटा देना आवश्यक है। अगर इस गांठ को और उसके साथ की कोशिकाओं एवं उसके मार्ग को ऑपरेशन के द्वारा हटाया नहीं जाता तो फिर से उभर आने की संभावना बनी रहती है। कई बार शेष रह गए थाइरोड की ये कोशिकाएं गांठ में परिवर्तित न हो कर गले के बीचोबीच छोटा सा छेद बना देती हैं। इसे थाइरोग्लोसल सायनस कहते हैं। थाइरोग्लोसल सायनस से समय-समय पर सफेद चिकना स्त्राव होता है। अगर इसमें संक्रमण लग जाता है तो गांठ तथा सायनस दोनों में ही रसी हो जाने की सम्भावना होती है। थाइरोग्लोसल सायनस का उपचार भी थाइरोग्लोसल सीस्ट की भांति ऑपरेशन के द्वारा किया जाता है। थाइरोग्लोसल सीस्ट की ही भांति अधूरे अथवा अपर्याप्त उपचार के कारण थाइरोग्लोसल सायनस के दुबारा उभर आने की संभावना होती है। •
Thoracoscopy / Video Assisted Thoracic Surgery (VATS)
INFORMATION AVAILABLE IN ENGLISH / GUJARATI AND HINDI
VIDEO ASSISTED THORACIC SURGERY (VATS)
VATS is a technique which involves surgery for various pathologies in the chest using key hole surgery. This is commonly known as thoracoscopy. Thoracic surgeries used to be done using large incisions. However, with technical advances and surgical expertise, these can now be done using 3 and 5 mm instruments.
Throacoscopy is commonly performed for the following pathologies in children :
- Empyema (Pus in the chest)
- Lobectomies – Removal of the part of the lung
- Cysts in the lung ( e.g. hydatid cysts, bronchogenic cysts)
- Cysts of the oesophagus (e.g. duplication cysts)
- Tumors in the chest (Tuberculosis, malignant tumors)
- Thymic tumors
- Diaphragmatic hernias
- Oesophageal atresias with tracheo-esophageal fistulas
GUJARATI
થોરેકોસ્કોપી
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો ( ડૂપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
थोरेकोस्कोपी
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३द्वद्व और ५द्वद्व के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (Empyema)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की Hydatid सीस्ट)
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
Torsion Testis / Acute Scrotum
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Acute Scrotum / Torsion Testis
Acute scrotum is sudden onset of redness and swelling over the scrotum. This is associated with severe pain over the scrotum and sometimes lower abdomen and may be accompanied with nausea and vomiting.
Of the many causes of acute scrotum, the most common and important is Torsion of Testis. The testis is supplied by a single blood vessel and any torsion on this vessel may impede the blood supply to the testis. If urgent medical attention and intervention is not done, this may result in testicular gangrene and orchidectomy ( removal of the dead testis) may be needed.
The commonly misleading history given by the parents is that the child may have had a trivial trauma or an insect bite. However, for the clinician the golden rule should be ‘Any acute scrotum is testicular torsion unless proved otherwise’. Investigations like ultrasound and color doppler may be done to help in the diagnosis. However, in the event of any doubt, it is safest to do a surgical exploration of the scrotum. The other uncommon causes of acute scrotum are acute epidydymo orchitis, scrotal abscess, idiopathic scrotal oedema and torsion of appendix of the testis. ●
 Acute Scrotum (Right scrotal Abscess)
Acute Scrotum (Right scrotal Abscess)

 Torsion of Left Undescended Testis (Pre operative and Operative Photo)
Torsion of Left Undescended Testis (Pre operative and Operative Photo)
 Acute Scrotum
Acute Scrotum

 Torsion Testis (Pre and Per operative photo)
Torsion Testis (Pre and Per operative photo)
GUJARATI
એક્યુટ સ્ક્રોટમ બાળકોમાં જાવામાં આવતી એક ગંભીર તકલીફ છે. આ બીમારી દર ચાર હજારે એક બાળકમાં જાવા મળે છે. નિદાનમાં મોડું થવાથી બાળક પોતાની વૃષણની ગોળી ખોઈ શકે છે. આ બીમારીમાં બાળકને વૃષણની કોથળી ઉપર લાલાશ અને સોજા જાવામાં આવે છે. આ સાથે બાળકને સખત દુઃખાવો અને ઉલટીઓ પણ થાય છે, જ્યારે બાળક ડાક્ટર પાસે લાવવામાં આવે ત્યારે તેના મા-બાપ અચૂક કહે છે કે, ‘બાળકને કદાચ સૂતી વખતે કોઈ જીવડું કરડી ગયું છે’ અથવા ‘કોઈ વસ્તુની ઍલર્જી થઈ છે’ અથવા તો ‘કંઈક વાગ્યું હશે’ તેના કારણે આ લાલાશ અને સોજા થયો છે. પરંતુ, આ વૃષણની ગોળી વળ ખાવાનાં કારણે થાય છે. જેને અંગ્રેજીમાં ‘ટોરઝન ટૅસ્ટીસ’ કહેવામાં આવે છે. વૃષણની ગોળી એક જ લોહીની નળી ઉપર લટકતી હોય છે. ગોળી વળ ખાઈ જવાથી તેને લોહી મળતું બંધ થઈ જાય છે. આ તકલીફનાં છ થી આઠ કલાકમાં આૅપરેશન કરવામાં ન આવે તો લોહી નહીં મળવાનાં કારણે ગોળી મરી જાય છે. આવા કેસમાં બાળકની વૃષણની ગોળી કાઢી નાખવી પડે છે. આથી જ્યારે પણ બાળકને ગોળી ઉપર લાલાશ કે સોજા હોય અને તેની સાથે દુખાવો પણ હોય તો તાત્કાલિક બાળકોના સર્જન ડાક્ટરનો સંપર્ક કરવો જાઈએ. •
HINDI
टॉर्शन वृषण/तीव्र अन्तग्ा्र्रथन (एक्यूट स्क्रोटम)
एक्यूट स्क्रोटम में वृषण पर अचानक लवण की शुरुआत होती है और सूजन होती है। इसके साथ ही अंडकोश की थैली में और कभी-कभी पेट के नीचले हिस्से में असहनीय दर्द के साथ मतली और उलटी होती है। अक्यूट स्क्रोटम के कई कारणों में सबसे सामान्य और मुख्य कारण है टेस्टिस में मरोड़ होना। एक ही खून की नली से टेस्टिस की आपूर्ति की जाती है और इस नली में कोई मरोड़ होने पर टेस्टिस को खून पहुँचाने में बाधा उत्पन्न हो सकती है। यदि तत्काल चिकित्सा और बचाव नहीं किया गया तो परिणाम स्वरूप टेस्टीकुलर गैंग्ा्रीन हो सकता है और ऑर्किडेक्टोमी करने की आवश्यकता पड़ सकती है।
आमतौर पर माता-पिता द्वारा यह भ्रामक विवरण दिया जाता है कि बच्चे को कदाचित हल्की चोट लगी होगी या किसी कीड़े ने काटा होगा। हालांकि, चिकित्सक के लिए स्वर्णिम नियम यह होना चाहिए कि ‘कोई भी एक्यूट स्क्रोटम वृषण टॉर्शन है जब तक कि अन्यथा साबित नहीं हो जाता है’। निदान में सहायता हेतु अल्ट्रासाउण्ड तथा कलर डॉप्लर जैसी जांच की जानी चाहिए। हालांकि, किसी भी संदेह की स्थिति में, अंडकोश की शल्य चिकित्सीय जांच पड़ताल करना सबसे सुरक्षित होगा। तीव्र अन्तग्ा्र्रथन के अन्य असामान्य कारणों में तीव्र एपिडायडिमूरचाइटिस, अंडकोषीय फोड़ा, इडियोपैथिक स्क्रोटल एडिमा और वृषण की पुच्छ के मरोड़ होते हैं। •
Testis (Undescended Testis)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What are undescended testicles?
This is when the child’s testicles are not in their usual place in the scrotum. While your child is in the womb, the testicles are developing inside his abdomen. Towards the end of pregnancy, the testicles travel through a passage into the scrotum. Both testicles should be in the scrotum by the time the child is one year old. Generally, only one of the testicles is affected, but on rare occasions, both testicles fail to travel to the scrotum.
In some children, the testicles may be in the scrotum for much of the time but cannot be felt there because they naturally rise back into the body through fear or cold temperatures. This is called retractile testis. You can usually find this out by putting your child in a warm bath and checking whether you can feel both testicles. If this is the case, there is no cause for concern.
What are the symptoms of undescended testicles?
Usually, there will not be any symptoms at all, other than not being able to feel the testicles in the scrotum. Your child will not be in pain, and the undescended testicles will not interfere with any bodily function.
However, if one of the testicles becomes twisted (testicular torsion), this will be painful, either in the groin area or the abdomen, depending on the location of the testicle at the time.
 Right Undescended Testis
Right Undescended Testis
 Bilateral Undescended Testis (Hypoplastic Scrotum)
Bilateral Undescended Testis (Hypoplastic Scrotum)
 Left Undescended Testis
Left Undescended Testis
 Ectopic Testis (Pre Penile Testis)
Ectopic Testis (Pre Penile Testis)
Testicular Torsion
How are undescended testicles diagnosed?
The doctor will need to determine whether the testicles are truly undescended or whether they have slid back into the body temporarily. This is usually done by feeling the abdomen and the scrotum.
No investigations like ultrasound scan or CT Scan or MRI can determine the presence / absence or exact location of the testis. These investigations should be sparingly used for determination of the site of an undescended testicle.
Laparoscopic view of undescended testis
What causes them?
On rare occasions, the testicle does not descend due to other problems with the testicles themselves or with the male hormones.
We do not know exactly why this happens, but it is not due to anything that happened during pregnancy.
How common are they?
This condition is more common in premature babies. 33 % of premature and 3 % of term children are born with undescended testis. The incidence of undescended testis at the age of 1 year is 1 %. Hence only 2 % of testicles descend up to the age of 1 year. The incidence of undescended testis in the adult population is 0.8%. These figures show that after the age of 1 year, there is hardly any decrease in the incidence of undescended testis.
How undescended testicles are treated and are there any alternatives?
The method of treatment depends on the suspected cause. However, whatever the cause, undescended testicles are best treated in early childhood latest by the first birthday of the child. Your child’s testicles will need treatment as they do not seem to mature properly if left in the abdomen. The amount of sperm and fertility levels seem lower in men who have had undescended testicles, and even lower if they were not treated early in childhood. This is because the testicles need to be a few degrees cooler than the rest of the body to produce sperm. It is also impossible for men with undescended testicles to check for testicular cancer, as the testicles cannot be felt in the abdomen. If the testicles remain in the abdomen, this also increases the risk of testicular torsion.
What is an orchidopexy?
This is an operation to bring the testicles down from the abdomen to their usual place in the scrotum. This is a short operation under general anaesthetic, lasting about 45 minutes. Occasionally, a child will need to stay in hospital overnight.
What does the operation involve?
Operation involves moving the testicle down into the scrotum, and close up the passage through which the testicle should have travelled, to stop the testicle moving back into your child’s abdomen. The testis is secured in the scrotum to ensure that it remains in place and develops in the normal way.
Operation can be done by the traditional open technique when the testis is palpable in the groins i.e. it has come out of the abdomen but not reached the scrotum. In cases where the testis has failed to come out of the abdomen key hole surgery or laparoscopy is used to determine the exact location of the testis in the abdomen along the course of its descent.
What happens afterwards?
The child will be reviewed a week after surgery. Follow up visits would be scheduled after 3, 6 and 12 months respectively.
What is the outlook for children with undescended testicles?
When the undescended testicles are treated in early childhood, the outlook is good. Your child will have normal fertility levels unless there were problems with the testicles themselves. In the event of the undescended testis being damaged prior to your realizing it / procuring treatment for the same, the child is left with on testicle. This however, should not affect your child’s fertility levels in later life to any great degree.
Operative videos of laparoscopy in undescended testis:
GUJARATI
વૃષણની ગોળી નીચે ન હોવી
અનડીસેન્ડેડ testis ત્રણ ટકા બાળકોમાં જાવા મળે છે. જા બાળક અધૂરા મહિને જન્મેલું હોય તો તેને અનડીસેન્ડેડ testis ની સંભાવના ૩૩% જેટલી વધારે હોય છે. બાળક એક વર્ષનું થાય ત્યાં સુધીમાં આ આંકડો ઘટીને ૧% જેટલો થઈ જાય છે. બાળક જ્યારે માઁ ના ગર્ભમાં હોય ત્યારે વૃષણની ગોળી બાળકના પેટમાં વિકાસ પામતી હોય છે. આ ગોળી ગર્ભનાં સાત થી નવ મહિના દરમિયાન બાળકના પેટમાંથી નીકળી અને વૃષણ કોથળીમાં આવી જાય છે, પરંતુ આ ગોળી બહાર આવવાના પ્રવાસ દરમિયાન અટકી જાય તો બાળકને જન્મ વખતે અનડીસેન્ડેડ ટેÂસ્ટસની ખોડ થાય છે. બાળકનો જન્મ થાય ત્યારે જ ડાક્ટર બંને ગોળી વૃષણ કોથળીમાં છે કે નહીં તેની તપાસ કરી લેતાં હોય છે.
સોનોગ્રાફી અથવા એમ.આર.આઈ. પણ ઘણીવાર ગોળી ક્યાં છે તેની સચોટ માહિતી આપવામાં નિષ્ફળ જતાં હોય છે.
વૃષણની ગોળીનું આૅપરેશન સામાન્ય રીતે બાળક છ મહિનાથી એક વર્ષની ઉંમરનું થાય એ દરમિયાન થઈ જવું જાઈએ. આ આૅપરેશનમાં જા મોડું થાય તો પેટની ગરમીથી વૃષણની ગોળીને નુકસાન થવાનો ભય રહે છે. જા ગોળીનું આૅપરેશન સચોટ અને સારી રીતે કરવામાં આવે તો બાળકને લગ્ન જીવનમાં કે બાળકો થવામાં બીજા બાળકોની સરખામણીમાં કોઈ જ તકલીફ પડતી નથી. વૃષણની ગોળી પેટની અંદર ફસાઈ ગઈ હોય તો તેવા કેસમાં બાળકને લેપ્રોસ્કોપી દ્વારા આૅપરેશન કરવાની જરૂર પડે છે. લેપ્રોસ્કોપીમાં ગોળી કઈ જગ્યાએ છે તે જાઈ શકાય છે અને સાથેજ લેપ્રોસ્કોપી દ્વારા તે ગોળી નીચે લાવી વૃષણ કોથળીમાં મૂકી શકાય છે. •
HINDI
अनवतीर्ण वृषण/अंडिसेंडेड टेस्टिस
टेस्टिस का विकास अंतःगर्भाशय काल में पेट की गुहा के भीतर होता है और बाद में ७वें और ९वे महीने के बीच अंतर्गर्भाशीय काल में वे अंडकोश में गिर जाते हैं। समय पर पैदा हुए ३% बालकों में और समयपूर्व पैदा हुए ३३% बालकों में अनडिसेंडेड टेस्टिस की समस्या पाई गई है। १ वर्ष की आयु तक इन बालकों में इस समस्या में १% तक की कमी पाई गई है। शिशु के जन्म के समय अंडकोश में दोनों टेस्टिस की जांच की जानी चाहिए।
अंडिसेंडेड टेस्टिस ९-१२ महीनों की आयु में स्वतः ही अंडकोश में गि्ार जाने के लिए जाने जाते है। हालाँकि, तब तक अगर वे अंडकोश में नहीं गि्ारते तो सर्जिकल हस्तक्षेप आवश्यक है। अनवतीर्ण वृषण का उपचार न किए जाने पर आगे चल कर आघात, मरोड़, ट्यूमर तथा शुक्राणुओं के कार्य में कमी जैसी जटिलताएं उœपन्न हो सकती है। अनवतीर्ण वृषण या तो पेट या अतिरिक्त पेट में हो सकते हैं। कोई भी जांच १००% सटीकता के साथ अंतर पेट के वृषण की उपस्थिति या अनुपस्थिति की पहचान नहीं कर सकता है। अतिरिक्त पेट वृषण के लिए, खुली सर्जरी की आवश्यकता होती है और अंतःप्राय वृषण के लिए, टेस्टिस की सटीक साइट और आकार की पहचान करने और अंडकोश में इसे लाने के लिए लैपरोस्कोपी अनिवार्य है। अंडिसेंडेड टेस्टिस की समस्या से ग्ा्रसित यदि कोई बालक बालचिकित्सा सर्जन के पास देरी से आता है तो टेस्टिस निकालना नहीं चाहिए, क्योंकि ऐसा करना बच्चे के लिए हानिकारक होगा। •
Teratoma (Sacrococcygeal teratoma)
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
SACROCOCCYGEAL TERATOMA
Sacrococcygeal teratoma (SCT) is a tumor that develops at the base of the coccyx (tail bone). It is seen in 1 in 35000 live births. Almost 75 % of SCT’s are benign, especially before the age of 5 months. These can be picked up on prenatal ultrasound scans. It can be of a small size like an orange but can grow to almost the size of a small water melon. They can be partly external and party internal.
The treatment for SCT is surgical removal. This is commonly done through the back. However, for large tumors or tumors with pelvic extension, opening the abdomen may be required. ●
GUJARATI
સેક્રોકોક્સીજિયલ ટેરાટોમા
આ એક જન્મજાત ખોડ છે. બાળકનાં જન્મ પહેલાં માતાની સોનોગ્રાફી કરાવવાથી ડિલિવરી પહેલા તેનુંં નિદાન થઈ શકે છે.
આવી ગાંઠ સંડાસની જગ્યાથી પાછળ અને પૂંછડીનાં છેલ્લાં હાડકાં સાથે જાડાયેલી હોય છે. તેનો આકાર નાની નારંગી જેવો અથવા મોટા તડબૂચ જેવો હોઈ શકે છે. ગાંઠ વધુ મોટી હોય તો નોર્મલ ડિલિવરી કરાવવા કરતાં સિઝેરિયન કરાવવું વધુ સારું છે.
આ ગાંઠ મોટી દેખાય છે પણ ૯૦% ઉપરનાં બાળકોમાં તે તદ્દન નિર્દોષ (કેન્સર નહીં) હોય છે. આ ગાંઠ સહેલાઈથી આૅપરેશન દ્વારા કાઢી શકાય છે અને બાળકોને કોઈ ખોડ-ખાંપણ રહેતી નથી. બાયોપ્સી અચૂક કરાવવી હિતાવહ છે.
આૅપરેશન બાળક ૧ મહિનાનું થાય ત્યાર પહેલાં કરાવવું, જેથી તેમાં કોઇ કોમ્પ્લીકેશન થાય નહીં. •
HINDI
पीठ के नीचे जन्मजात गांठ ( Sacrococcygeal टेराटोमा)
पीठ के नीचे गांठ (Sacrococcygeal टेराटोमा) का होना एक जन्मजात दोष है जिसकी पहचान प्रसूति से पहले माता की सोनोग्राफी कराने से की जा सकती है। यह गांठ पीठ के सबसे नीचे की हड्डी के साथ जुड़ी हुई होती है और ३५००० में से १ बच्चे में यह दोष देखा जाता है। शुरूआत में यह गांठ नारंगी के आकार की और धीरे-धीरे बढ़कर छोटे तरबूज के आकार की हो सकती है, जो आधी शरीर के भीतर और आधी बाहर होती है।
यह गांठ भले ही बड़ी दिखाई देती है, लेकिन इस समस्या वाले ९०% बच्चों में कैंसर नहीं होता और कुशलतापूर्वक ऑपरेशन से इस गांठ को निकाला जा सकता है। नवजात बच्चे के एक महीने का होने से पहले यह ऑपरेशन करा लेना चाहिए, जिससे बालक को आगे कोई तकलीफ न हो। •
Ureteric Re-Implantation
What is the ureteric re-implantation operation and why might my child need it?
As shown in the diagram, the ureters are two tubes which carry urine from the kidneys to the bladder. In some children, the ureters do not join the bladder in the correct place and this can cause a condition called vesicoureteral reflux (VUR). Normally, valves between the ureters and the bladder prevent urine ‘backing up’ and flowing towards the kidneys. If the ureters do not join the bladder in the correct place, these valves can fail, allowing urine to flow backwards from bladder to kidney. This can damage the kidney and eventually lead to kidney failure.
What does the operation involve?
At surgery, an incision (cut) is made in the lower abdomen. The ureters are disconnected from their attachment to the bladder. The ureters are then reattached to the bladder in the correct place. The end of the ureters joining the bladder will then be surrounded by muscle, which will strengthen the valves, reducing the chances of urine flowing back to the kidneys. The operation takes between 1and a half and 2 hours. The usual hospital stay is 5 – 7 days.
Surgery for Ureteric Reimplant
What are the risks of this operation?
The operation risk is minimum. There is sometimes bleeding when the surgeon disconnects the ureters during the operation. This is usually only slight, but if a lot of blood is lost your child may need to be given a blood transfusion.
Are there any alternatives to the operation?
If your child has VUR and needs their valve to be repaired, there is one alternative to surgery. STING is an injection which is given into the valve in the bladder, with the help of cystoscopy (a tube with a camera on the end which is inserted into the bladder). STING is quicker and enables an early discharge from the hospital. More details about the pros and cons and whether your child is suitable for the treatment can be obtained at the time of consultation.
Click here Movies for Deflux Injection

Deflux seen on ultrasound after injection
When you get home
The child should be encouraged to drink lots of water / liquids.
Antibiotics will be given to your child at discharge to be continued for 6 weeks. A regular urine check needs to be done on a monthly basis for 6 months after surgery. We will monitor the postoperative changes with an ultrasound scan and if needed a nuclear scan. Advise regarding the same will be given to you at the time of discharge.
Undescended Testes
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
What are undescended testicles?
This is when the child’s testicles are not in their usual place in the scrotum. While your child is in the womb, the testicles are developing inside his abdomen. Towards the end of pregnancy, the testicles travel through a passage into the scrotum. Both testicles should be in the scrotum by the time the child is one year old. Generally, only one of the testicles is affected, but on rare occasions, both testicles fail to travel to the scrotum.
In some children, the testicles may be in the scrotum for much of the time but cannot be felt there because they naturally rise back into the body through fear or cold temperatures. This is called retractile testis. You can usually find this out by putting your child in a warm bath and checking whether you can feel both testicles. If this is the case, there is no cause for concern.
What are the symptoms of undescended testicles?
Usually, there will not be any symptoms at all, other than not being able to feel the testicles in the scrotum. Your child will not be in pain, and the undescended testicles will not interfere with any bodily function.
However, if one of the testicles becomes twisted (testicular torsion), this will be painful, either in the groin area or the abdomen, depending on the location of the testicle at the time.
 Right Undescended Testis
Right Undescended Testis
 Bilateral Undescended Testis (Hypoplastic Scrotum)
Bilateral Undescended Testis (Hypoplastic Scrotum)
 Left Undescended Testis
Left Undescended Testis
 Ectopic Testis (Pre Penile Testis)
Ectopic Testis (Pre Penile Testis)
Testicular Torsion
How are undescended testicles diagnosed?
The doctor will need to determine whether the testicles are truly undescended or whether they have slid back into the body temporarily. This is usually done by feeling the abdomen and the scrotum.
No investigations like ultrasound scan or CT Scan or MRI can determine the presence / absence or exact location of the testis. These investigations should be sparingly used for determination of the site of an undescended testicle.
Laparoscopic view of undescended testis
What causes them?
On rare occasions, the testicle does not descend due to other problems with the testicles themselves or with the male hormones.
We do not know exactly why this happens, but it is not due to anything that happened during pregnancy.
How common are they?
This condition is more common in premature babies. 33 % of premature and 3 % of term children are born with undescended testis. The incidence of undescended testis at the age of 1 year is 1 %. Hence only 2 % of testicles descend up to the age of 1 year. The incidence of undescended testis in the adult population is 0.8%. These figures show that after the age of 1 year, there is hardly any decrease in the incidence of undescended testis.
How undescended testicles are treated and are there any alternatives?
The method of treatment depends on the suspected cause. However, whatever the cause, undescended testicles are best treated in early childhood latest by the first birthday of the child. Your child’s testicles will need treatment as they do not seem to mature properly if left in the abdomen. The amount of sperm and fertility levels seem lower in men who have had undescended testicles, and even lower if they were not treated early in childhood. This is because the testicles need to be a few degrees cooler than the rest of the body to produce sperm. It is also impossible for men with undescended testicles to check for testicular cancer, as the testicles cannot be felt in the abdomen. If the testicles remain in the abdomen, this also increases the risk of testicular torsion.
What is an orchidopexy?
This is an operation to bring the testicles down from the abdomen to their usual place in the scrotum. This is a short operation under general anaesthetic, lasting about 45 minutes. Occasionally, a child will need to stay in hospital overnight.
What does the operation involve?
Operation involves moving the testicle down into the scrotum, and close up the passage through which the testicle should have travelled, to stop the testicle moving back into your child’s abdomen. The testis is secured in the scrotum to ensure that it remains in place and develops in the normal way.
Operation can be done by the traditional open technique when the testis is palpable in the groins i.e. it has come out of the abdomen but not reached the scrotum. In cases where the testis has failed to come out of the abdomen key hole surgery or laparoscopy is used to determine the exact location of the testis in the abdomen along the course of its descent.
What happens afterwards?
The child will be reviewed a week after surgery. Follow up visits would be scheduled after 3, 6 and 12 months respectively.
What is the outlook for children with undescended testicles?
When the undescended testicles are treated in early childhood, the outlook is good. Your child will have normal fertility levels unless there were problems with the testicles themselves. In the event of the undescended testis being damaged prior to your realizing it / procuring treatment for the same, the child is left with on testicle. This however, should not affect your child’s fertility levels in later life to any great degree.
Operative videos of laparoscopy in undescended testis:
GUJARATI
વૃષણની ગોળી નીચે ન હોવી
અનડીસેન્ડેડ testis ત્રણ ટકા બાળકોમાં જાવા મળે છે. જા બાળક અધૂરા મહિને જન્મેલું હોય તો તેને અનડીસેન્ડેડ testis ની સંભાવના ૩૩% જેટલી વધારે હોય છે. બાળક એક વર્ષનું થાય ત્યાં સુધીમાં આ આંકડો ઘટીને ૧% જેટલો થઈ જાય છે. બાળક જ્યારે માઁ ના ગર્ભમાં હોય ત્યારે વૃષણની ગોળી બાળકના પેટમાં વિકાસ પામતી હોય છે. આ ગોળી ગર્ભનાં સાત થી નવ મહિના દરમિયાન બાળકના પેટમાંથી નીકળી અને વૃષણ કોથળીમાં આવી જાય છે, પરંતુ આ ગોળી બહાર આવવાના પ્રવાસ દરમિયાન અટકી જાય તો બાળકને જન્મ વખતે અનડીસેન્ડેડ ટેÂસ્ટસની ખોડ થાય છે. બાળકનો જન્મ થાય ત્યારે જ ડાક્ટર બંને ગોળી વૃષણ કોથળીમાં છે કે નહીં તેની તપાસ કરી લેતાં હોય છે.
સોનોગ્રાફી અથવા એમ.આર.આઈ. પણ ઘણીવાર ગોળી ક્યાં છે તેની સચોટ માહિતી આપવામાં નિષ્ફળ જતાં હોય છે.
વૃષણની ગોળીનું આૅપરેશન સામાન્ય રીતે બાળક છ મહિનાથી એક વર્ષની ઉંમરનું થાય એ દરમિયાન થઈ જવું જાઈએ. આ આૅપરેશનમાં જા મોડું થાય તો પેટની ગરમીથી વૃષણની ગોળીને નુકસાન થવાનો ભય રહે છે. જા ગોળીનું આૅપરેશન સચોટ અને સારી રીતે કરવામાં આવે તો બાળકને લગ્ન જીવનમાં કે બાળકો થવામાં બીજા બાળકોની સરખામણીમાં કોઈ જ તકલીફ પડતી નથી. વૃષણની ગોળી પેટની અંદર ફસાઈ ગઈ હોય તો તેવા કેસમાં બાળકને લેપ્રોસ્કોપી દ્વારા આૅપરેશન કરવાની જરૂર પડે છે. લેપ્રોસ્કોપીમાં ગોળી કઈ જગ્યાએ છે તે જાઈ શકાય છે અને સાથેજ લેપ્રોસ્કોપી દ્વારા તે ગોળી નીચે લાવી વૃષણ કોથળીમાં મૂકી શકાય છે. •
HINDI
अनवतीर्ण वृषण/अंडिसेंडेड टेस्टिस
टेस्टिस का विकास अंतःगर्भाशय काल में पेट की गुहा के भीतर होता है और बाद में ७वें और ९वे महीने के बीच अंतर्गर्भाशीय काल में वे अंडकोश में गिर जाते हैं। समय पर पैदा हुए ३% बालकों में और समयपूर्व पैदा हुए ३३% बालकों में अनडिसेंडेड टेस्टिस की समस्या पाई गई है। १ वर्ष की आयु तक इन बालकों में इस समस्या में १% तक की कमी पाई गई है। शिशु के जन्म के समय अंडकोश में दोनों टेस्टिस की जांच की जानी चाहिए।
अंडिसेंडेड टेस्टिस ९-१२ महीनों की आयु में स्वतः ही अंडकोश में गि्ार जाने के लिए जाने जाते है। हालाँकि, तब तक अगर वे अंडकोश में नहीं गि्ारते तो सर्जिकल हस्तक्षेप आवश्यक है। अनवतीर्ण वृषण का उपचार न किए जाने पर आगे चल कर आघात, मरोड़, ट्यूमर तथा शुक्राणुओं के कार्य में कमी जैसी जटिलताएं उœपन्न हो सकती है। अनवतीर्ण वृषण या तो पेट या अतिरिक्त पेट में हो सकते हैं। कोई भी जांच १००% सटीकता के साथ अंतर पेट के वृषण की उपस्थिति या अनुपस्थिति की पहचान नहीं कर सकता है। अतिरिक्त पेट वृषण के लिए, खुली सर्जरी की आवश्यकता होती है और अंतःप्राय वृषण के लिए, टेस्टिस की सटीक साइट और आकार की पहचान करने और अंडकोश में इसे लाने के लिए लैपरोस्कोपी अनिवार्य है। अंडिसेंडेड टेस्टिस की समस्या से ग्ा्रसित यदि कोई बालक बालचिकित्सा सर्जन के पास देरी से आता है तो टेस्टिस निकालना नहीं चाहिए, क्योंकि ऐसा करना बच्चे के लिए हानिकारक होगा। •
Urinary tract infection
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Urinary tract infections in children with abnormal urinary tracts
It is an infection affecting one of the various parts of the urinary system. Doctors often call it a urinary tract infection or UTI for short.
The urinary system consists of the kidneys, ureters, the bladder and urethra. The kidneys filter the blood to remove waste products and produce urine.
The urine flows from the kidneys down through the ureters to the bladder, where it is stored until we go to the toilet. It passes through another tube called the urethra to the outside when urinating (passing urine).
What is different about UTI in children with known problems with the urinary tract?
Some children are born with a problem with the urinary tract. There can be different malformations, such as posterior urethral valves, hydronephsosis and hydrometers or vesico-ureteric reflux.
All these malformations have one thing in common, that is, the urine flow is not normal. It can be slow due to an obstruction or narrowing of the ureter for instance. There can also be ‘residual urine’, which means that the bladder is not emptied totally when passing urine, leaving some urine behind.
These problems increase the risk of developing a UTI. A UTI has more impact on children with a known problem with the urinary tract, as they have kidney problems present from birth (congenital). If this is the case with both kidneys, or the child only has one kidney, then there is a risk that he or she has impaired kidney function.
What kinds of UTI are there?
There are three kinds of UTI, each with different symptoms, but all of which can be very important for a child with a known problem with the urinary tract.
Acute pyelonephritis
This means ‘infection of the kidneys’. This is the most important infection as it can cause kidney damage. It is therefore very important to diagnose and treat pyelonephritis rapidly.
The main sign of a kidney infection is a very high temperature. A child will also have symptoms of being generally unwell, such as vomiting, drowsiness or pain affecting the stomach or sides.
If your child develops an unexplained fever or any of these symptoms, you should always make sure that his or her urine is tested for infection. If there are signs of infection, the doctor will prescribe a course of antibiotics, which can prevent kidney damage.
You should always ensure that your child completes the course of antibiotics, even if he or she seems to be getting better. If your child does not complete the course of antibiotics, then this could allow the infection to come back and possibly not respond so well to antibiotics the next time.
Acute cystitis
This means ‘infection of the bladder’. This often gives a lot of pain in the stomach and discomfort when passing urine. The urine can also contain blood and so look a red or pink colour.
Generally, a child with a bladder infection will not have as high a temperature as a kidney infection. The infection needs treatment to take away the pain but it does not cause kidney damage.
Asymptomatic bacteriuria (ABU)
This means that bacteria is growing in the urine but is not producing any symptoms. Children with normal urinary tracts sometimes get ABU and it is very common in children any kind of problem with urine flow.
It is not dangerous as it does not have any symptoms and does not lead to kidney damage. It is also very difficult to treat. Even if antibiotics treat the bacteria, it will often come back after a few days. Treatment with antibiotics is therefore reserved for when symptoms are present.
How can UTI be investigated?
The doctor will advise you depending upon the child’s age and symptoms as to what investigations need to be done.
A urine routine examination will necessary and a urine culture will also be required to see what germs are growing in the urine and what antibiotics are effective against those germs.
An ultrasound scan may be required to see if there is any structural problem with the urinary tract like blockage or abnormal swelling of the kidneys, ureters or the bladder. In some children an investigation called MCUG / VCUG (micturating / voiding cystourethrogram) may be required. In some children advanced investigations like a CT scan or a nuclear scan may also be required. Your doctor will explain you about the investigations and their need if required for your child.
How can recurrent UTI be treated?
The most important thing is to create a good flow of urine. Encouraging drinking of plenty of fluids combined with regular urination and avoidance of constipation are extremely important ways of preventing infections.
This might mean an operation to remove any obstruction..
Remember
- Children with known urinary tract problems are very prone to developing urinary tract infections (UTI).
- Only some types of UTI cause kidney damage, and these normally cause a very high temperature and symptoms of being generally unwell.
- These types of UTI need to be diagnosed and treated as early as possible to prevent kidney damage.
- If your child has a very high temperature or is generally unwell with no obvious cause, ask your doctor to test your child’s urine.
 Non Functioning Double (Duplex) Kidneys
Non Functioning Double (Duplex) Kidneys
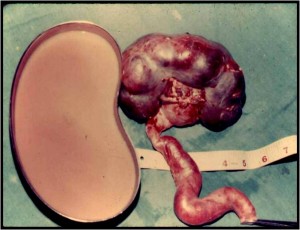 Infected Kidney withe Pus in it
Infected Kidney withe Pus in it
 Multicystic Dysplastic kidney
Multicystic Dysplastic kidney
GUJARATI
પેશાબમાં ઇન્ફેક્શન
પેશાબમાં ઇન્ફેક્શન બાળકોમાં ખૂબ જ સામાન્ય બીમારી છે અને નિદાન ન થતાં બાળક ઘણીવાર કીડની ડેમેજ અથવા ઊંચા બ્લડપ્રેશરનો શીકાર બને છે. ૩ વર્ષની નીચેની ઉંમરના બાળકને આ બીમારીમાં પેશાબની તકલીફ કરતાં વારંવાર તાવ આવે, ભૂખ ન લાગે અને વજન ઘટતું હોય છે. નિદાન કર્યા વગર એન્ટિબાયોટિક લેતાં ઘણું નુકસાન થાય છે.
૩ વર્ષ થી મોટા બાળકમાં પેશાબની બળતરા, વારંવાર પેશાબ થવો અને તાવ સાથે જનરલ હેલ્થ બગડતી જાવા મળે છે.
સચોટ નિદાન : પેશાબમાં ઇન્ફેક્શનનું સચોટ નિદાન કોઈ પણ બાળકને વારંવાર તાવ આવે તો કરાવવું જરૂરી છે. પેશાબની તપાસ અને સોનોગ્રાફીની પ્રાથમિક તપાસ કરાવ્યા પછી જ ટ્રીટમેન્ટ અને જરૂર પડે આગળ તપાસ કરાવવી જાઈએ. •
HINDI
पेशाब मार्ग में संक्रमण
पेशाब मार्ग का संक्रमण बच्चों में एक आम बात है। इसका निदान न होने पर कई बार बच्चे की किडनी कराब हो सकती है तथा बच्चा उच्च रक्तचाप का शिकार हो सकता है। ३ वर्ष से नीचे की आयु वाले बच्चे में पेशाब की तकलीफ के अलावा बार-बार बुखार आना, भूख न लगना और वजन का घटना आदि समस्याएं होती हैं। बिना निदान किए एंटीबायोटिक्स देने से अधिक नुक्सान हो सकता है।
३ वर्ष से अधिक आयु के बच्चे को पेशाब में जलन, बार-बार पेशाब करना और बुखार के साथ स्वास्थ्य का बिगड़ना जैसी समस्याएं होती हैं।
सटीक निदान: किसी भी बच्चे को यदि बार-बार बुखार आता है तो पेशाब मार्ग का सटीक निदान कराना आवश्यक है। सोनोग्ा्राफी द्वारा जाँच के उपरांत ही उपचार करना चाहिए और आवश्यक होने पर आगे की जाँच करानी चाहिए। •
Umbilical Hernia / Para Umbilical Hernia
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Umbilical and Paraumbilical Hernia
Umbilical hernia is seen in 5 % of children. The umbilical cord is attached to the area of the umbilicus in the intrauterine life. This area has a defect in the abdominal wall which closes after birth and forms the belly button. When this defect does not close spontaneously, the intestines may bulge through it when the child cries or strains and is called an umbilical hernia.
Umbilical hernias normally resolve spontaneously by the age of 2 years. If the size does not reduce after 2 years, then surgery is advisable. Application of coins or belts does not help in cure of umbilical hernias.
Many a times, the hernia may not be located at the umbilicus, but around it. These are called para umbilical hernias. Paraumbilical hernias do not resolve spontaneously. They also have a chance of the intestine getting blocked in the defect. Hence early surgery is advisable in cases of paraumbilical hernias unlike umbilical hernia. ●
 Umbilical Hernia
Umbilical Hernia

 Supra Umblical Hernia
Supra Umblical Hernia

 Application of Belts and Coins should be avoided
Application of Belts and Coins should be avoided
 Postoperative photo after Umbilical Hernia Repair
Postoperative photo after Umbilical Hernia Repair
GUJARATI
મોટો દૂંટો (દૂંટીની સારણગાંઠ)
દૂંટીની સારણગાંઠ ૫% બાળકમાં જાવા મળે છે. બાળક માઁ ના ગર્ભમાં હોય ત્યારે નાળ દૂંટીના ભાગમાં જાડાયેલી હોય છે. બાળકના જન્મ પછી નાળ ખરી જાય છે અને તે રસ્તો બંધ થઈ જાય છે. આ રસ્તો બંધ ન થવાથી પેટની દીવાલમાં કાણું રહી જાય છે, જેમાંથી આંતરડા બહાર નીકળી ને મોટો દૂંટો કે દૂંટીની સારણગાંઠ કરે છે. દૂંટીની સારણગાંઠ ૨ વર્ષની ઉંમર સુધીમાં જાતે મટી જાય છે. દૂંટીની સારણગાંઠમાં સિક્કા કે બૅલ્ટ બાંધવાથી કોઈ ફાયદો થતો નથી.
બાળક બે વર્ષનું થાય ત્યાં સુધીમાં દૂંટીની સારણગાંઠ મટી ન હોય તો તેના માટે આૅપરેશન કરવું જરૂરી બને છે. આૅપરેશન સામાન્ય અને જાખમ વગરનું હોય છે. આ આૅપરેશનમાં પેટની દીવાલમાં કાણું હોય તેને ટાંકા વડે બંધ કરી દેવામાં આવે છે. ઘણીવાર દૂંટીના આજુબાજુના સ્નાયુઓમાં જગ્યા હોવાથી પણ મોટો દૂંટો બનતો હોય છે. આ તકલીફને પેરાઅÂમ્બલીકલ હર્નિયા કહેવાય છે. આ ખોડ જાવામાં તો મોટા દૂંટા જેવી જ લાગતી હોય છે, પરંતુ બાળકોના સર્જનને બતાવ્યા પછી જ આ ખોડ પેરાઅÂમ્બલીકલ હર્નિયા છે કે નહીં તે ખબર પડે છે. પેરાઅÂમ્બલીકલ હર્નિયામાં આંતરડું ફસાવાની શક્યતા રહેલી છે. મોટા દૂંટાથી વિપરીત પેરાઅÂમ્બલીકલ હર્નિયામાં જેટલું બને તેટલું વહેલું આૅપરેશન કરવું જરૂરી છે. •
HINDI
नाभि तथा नाभि के पास हर्निया
नाभि हर्निया ५% बच्चों में पाया जाता है। अंतर्गर्भाशीय काल के दौरान गर्भनाल नाभि के क्षेत्र में नाभि से जुड़ा हुआ होता है। इस क्षेत्र में पेट की दीवार में एक दोष होता है जो जन्म के बाद बंद हो जाता है और पेट बटन का निर्माण करता है। जब यह दोष स्वतः बंद नहीं होता है, तब बच्चे के रोने पर अथवा तनाव लाने पर आंतो में उभार उत्पन्न होता है जिसे नाभि हर्निया कहा जाता है। नाभि हर्निया सामान्य रूप से २ वर्ष की आयु तक अपने आप ठीक हो जाता है। यदि २ वर्ष के बाद आकार में कमी नहीं आती है, तो शैल्यचिकित्सा उचित होगी। सिक्कों या बेल्टों का उपयोग नाभि हर्निया के इलाज में मदद नहीं करता है। कई बार, हर्निया नाभि पर स्थित नहीं होता है, लेकिन इसके आस-पास होता है। इन्हें नाभि के पास या परानाभि हर्निया कहते हैं। परानाभि हर्निया अपने आप नहीं मिटता। इस हर्निया में दोष क्षेत्र में आंत में रुकावट होने की भी संभावना है। इस वजह से नाभि हर्निया के विपरीत नाभि के पास वाले हर्निया में प्रारंभ में ही सर्जरी की सलाह दी जाती है। •
Umbilical Granuloma / Umbilical Polyp
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Umbilical Granuloma and Polyp
Umbilical granuloma is a small red lesion located in the umbilicus. It is a remnant of the umbilical cord that detaches within days after birth. This may cause recurrent whitish or watery discharge and occasional bleeding on friction. This can be normally treated with application of antibiotic powder or even common salt. However, if it persists, medical attention is necessary. The granuloma requires to be burnt using either electrocautery or chemically with nitric oxide sticks.




 Umbilical Granumola / Polyp
Umbilical Granumola / Polyp
GUJARATI
દૂંટીનો મસો
દૂંટીનો મસો સામાન્ય બીમારી છે. બાળક જ્યારે જન્મે ત્યારે નાળ દૂંટી સાથે જાડાયેલી હોય છે. આ નાળ દસ દિવસમાં ખરી જાય છે. નાળ ખર્યા પછી અમુક કોષ રહી જવાના કારણે દૂંટીનો મસો થાય છે.દૂંટીના મસામાં નાની ચણોઠી જેવા આકારની લાલ ગાંઠ દૂંટીમાં જાવા મળે છે જેમાંથી પાણી અથવા ચીકણો પદાર્થ નીકળે છે. ઘસારો થવાથી આ ગાંઠમાંથી લોહી પણ નીકળે છે. દૂંટીના મસામાં સામાન્ય સંજાગોમાં કોઈ એÂક્ટવ ટ્રિટમેન્ટ આપવામાં આવતી નથી. સામાન્ય ઍÂન્ટબાયાટીક પાવડર છાંટવાથી અને ચોખ્ખાઈ રાખવાથી આ મસો મટી જાય છે. ઘણીવાર સહેજ મીઠાંનું પાણી લગાવવાથી પણ દૂંટીનો મસો તેની મેળે ઓગળી જાય છે. અલબત્ત, આ રીતની ટ્રિટમેન્ટ કરવા છતાં દૂંટીનો મસો જેમ નો તેમ રહેતો હોય તો એક નાનું આૅપરેશન કરી લેસર વડે દૂંટીનો મસો બાળી નાખવો પડે. આથી વિપરીત દૂંટીમાં દ્રાંક્ષ જેવી ગાંઠ કે જેને અÂમ્બલીકલ પાલીપ કહેવામાં આવે છે તે પણ જાવામાં આવતી હોય છે. આ રીતની ગાંઠમાં ઘણીવાર આંતરડું દૂંટીના અંદરના ભાગમાં જાડાયેલું હોય છે. આવા કેસમાં બહારની ગાંઠ કાઢી નાખવાથી ટ્રિટમેન્ટ અધૂરી રહે છે. લેપ્રોસ્કોપી કરી પેટની અંદર આંતરડા સાથે જાડાણ નથી તે જાણ્યા પછી જ બાહ્ય ગાંઠનું આૅપરેશન કરવું એ સંપૂર્ણ ટ્રિટમેન્ટ છે. •
HINDI
नाभिकीय ग्रेन्युलोमा एवं पोलिप
नाभिकीय ग्रेन्युलोमा नाभि में स्थित एक प्रकार का छोटा लाल घाव होता है। यह गर्भनाल का एक अवशेष होता है जो जन्म के बाद नाभी अलग हो जाने पर रह जाता है। इसके कारण बार-बार सफेद स्त्राव या पानी जैसा स्त्राव और कभी-कभार घर्षण होने पर रक्त स्राव हो सकता है। इसका उपचार सामान्य रूप से एंटीबायोटिक पाउडर के उपयोग से या यहां तक कि साधारण नमक से भी किया जा सकता है। हालांकि, अगर समस्या बनी रहती है तो चिकित्सीय देखभाल आवश्यक हो जाती है। नाइट्रिक ऑक्साइड छड़ों का उपयोग करके विद्युतचुंबकीय अथवा रासायनिक से ग्रेन्युलोमा को जला देने की आवश्यकता होती है।
कभी-कभी बच्चे की नाभि के पास बड़ा सा लाल अंगूर जैसा घाव बन सकता है। इसे नाभीय पोलीप कहा जाता है और इसकी अधिकतर आंत के आंतरिक जुड़ाव की संभावना होती है (विटेलो-आंतों की वाहिनी)। ऐसी स्थिति में, नाभिकीय पोलीप को काटना पर्यात उपचार नहीं है। ऐसे में बच्चे में इसके लक्षण बने रहने की संभावना रहती है। ऐसे मामलों में लेप्रोस्कोपी के द्वारा पेट के अंदर आंतों के आपसी जोड़ नहीं होने का पता लगाने के बाद बाहरी गांठ का ऑपरेशन किया जाता है। •
Umbilical Discharge
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
UMBILICAL DISCHARGE
Children sometimes have a discharge coming from the umbilicus. This could be watery, purulent or foul smelling. Chronic discharge may also cause excoriation of the skin around the umbilicus. This could be the result of either a local umbilical infection or an abnormal connection of a part of the intestine (Patent vitello intestinal duct) or urinary bladder (patent urachus) to the under surface of the umbilicus. The diagnosis of this problem needed open operation in yesteryears. However, with the advent of laparoscopy, these lesions can be diagnosed and treated without open surgery. ●

 Umbilical Discharge causing a persistently wet umbilicus
Umbilical Discharge causing a persistently wet umbilicus
GUJARATI
દૂંટીમાંથી પાણી અથવા બગાડ નીકળવો :
ઘણા બાળકોમાં જન્મ પછી દૂંટીના ભાગેથી પ્રવાહી, ચીકાશ અથવા મળ જેવું પ્રવાહી નીકળતું હોય છે. પ્રવાહી વધુ પ્રમાણમાં નિકળવાથી દૂંટીની આજુબાજુની ચામડી ફદફદી જાય છે. આ તકલીફને અÂમ્બલીકલ ડીસચાર્જ કહેવામાં આવે છે. આ ખોડમાં પેશાબની કોથળીનો અમુક ભાગ અથવાતો આંતરડાનો અમુક ભાગ દૂંટીના અંદરના ભાગ સાથે જાડાયેલો હોવાથી આંતરડામાં બનતા ચીકાશ અથવા મળ દૂંટી વાટેથી બહાર નીકળે છે. જા પેશાબની કોથળી જાડાયેલી હોય તો પેશાબ પણ આ રીતે બહાર નીકળે છે. પહેલા જમાનામાં આ ખોડ માટે પેટ ખોલીને આૅપરેશન કરવામાં આવતું હતું, પરંતુ હવે લેપ્રોસ્કોપીના આગમન પછી આ આૅપરેશન સંપૂર્ણ રીતે દૂરબીનથી જ થઈ શકે છે. લેપ્રોસ્કોપીથી આ ખોડનું સચોટ નિદાન અને નિવારણ થઈ શકે છે. •
HINDI
नाभिकीय स्त्राव :
बच्चों की गर्भनाल से कभी-कभी एक स्त्राव होता है। यह पानी जैसा, मवादयुक्तU अथवा बदबूदार हो सकता है। लंबे समय तक स्त्राव होने से यह नाभी के चारों ओर त्वचा को नुकसान पहुंचा सकता है। इसका कारण स्थानीय नाभिक संक्रमण अथवा आंतों के किसी हिस्से (पेटेंट क्द्बह्लद्गद्यद्य्रू आंत्र वाहिनी) का या मूत्राशय (पेटेंट यूरैचस) का नाभि की नीचे की सतह से असामान्य रूप से जुड़ा होना हो सकता है। पूर्वकाल में इस समस्या के निदान के लिए खुले आपरेशन की आवश्यकता होती थी। हालांकि, लैप्रोस्कोपी के आने के बाद इन घावों का निदान एवं उपचार बिना खुली सर्जरी के संभव हो गया है। •
Vesicoureteric Reflux
Vesicoureteric Reflux
The urinary system consists of the kidneys, the bladder and ureters. The kidneys filter the blood to remove waste products and form urine. The urine flows from the kidneys down through the ureters to the bladder in a one way direction.
The ureters tunnel through the wall of the bladder at an angle to form a flap that acts as a valve. The valves between the ureters and bladder prevent urine flowing backwards into the ureters, so that all the urine in the bladder is passed in one go, as the urine cannot travel anywhere else. As the urine leaves the bladder at a high pressure, the valves stop this high pressure being passed on to the kidneys.
What is vesico-ureteric reflux (VUR)?
Vesico-ureteric reflux (VUR) occurs when the valve between the ureters and the bladder is not working properly, allowing urine to flow backwards into the ureters. Depending on the severity of the VUR, sometimes the urine can flow backwards as far as the kidneys. If infected urine flows into the kidneys, this can damage them.
What are the symptoms of VUR?
Sometimes VUR can be diagnosed before birth when an ultrasound scan shows that one or both of a baby’s kidneys look swollen and larger than usual (hydronephrosis). VUR is one of the conditions that cause hydronephrosis.
When VUR is diagnosed after birth, it is usually suspected if a child has repeated urine infections. Symptoms of a urine infection can include: burning sensation during urination, urinating more often than usual, abdominal pain, a high temperature, vomiting, reduced appetite or foul smelling urine. Some children also present with recurrent diarrohea or with poor weight gain. If a child has VUR, urine infections can damage the kidneys, as the urine flowing backwards towards them contains bacteria. Kidney damage can cause high blood pressure in later life or if untreated, may lead to kidney failure.
How is VUR diagnosed?
VUR is diagnosed and monitored using two particular scans:
- Ultrasound scans are used to diagnose hydronephrosis before birth and to check the structure of the bladder, ureters and kidneys after birth.
- The other test is called a micturating / voiding cysto-urethrogram (MCUG / VCUG). This uses a liquid that shows up on x-rays, which is put inside the bladder through a catheter (thin, plastic tube) inserted into the urethra. Once the bladder is full of this liquid, the child urinates while being scanned. This shows whether all the liquid is being passed through the urethra, or whether any of it is flowing backwards through the ureters towards the kidneys.
The MCUG / VCUG test is also used to ‘grade’ the degree of reflux, according to its severity; grade 1 is the least severe form of VUR, where urine is flowing back up the ureters but is not reaching the kidneys and grade 5 is the most severe, where a great deal of urine is reaching the kidneys, making the ureter and kidney swollen. VUR is also described as ‘unilateral’ or ‘bilateral’ depending on whether one kidney (unilateral) is affected or both (bilateral).
Grades of Vesicoureteric Reflux

Bilateral Vesico ureteric reflux seen on MCU
What causes VUR?
In many children, the tunnel through the bladder wall is not long enough, so the valve does not work properly, but this can improve as the child grows. In some children, the ureters enter the bladder in a higher position than normal, which also means that the valve does not work properly; this is less likely to improve as the child grows. Other children, particularly boys, may have a blockage in the urethra (posterior urethral valves) causing VUR.
How common is VUR?
VUR occurs in about one in every 100 children. If one child in a family has VUR, there is a chance that the other children could have VUR too, so monitoring might be suggested for brothers and sisters. VUR is usually diagnosed in under fives; it is much less common in older children, who may have outgrown the problem.
How can VUR be treated?
We treat VUR using medicines at first. Usually, a low dose of antibiotics is given on a long-term basis. This prevents urinary tract infections, which in turn, prevents any damage to the kidney caused by infected urine flowing backwards into them. Treatment with antibiotics gives many children the opportunity to outgrow VUR.
Children with VUR who are taking antibiotics will need to give regular urine samples, to be checked for any urine infections, particularly at an early stage. Ultrasound scans are often used to check that the kidneys are growing properly. Nuclear scans also are done to see how much damage is caused to the kidneys by the reflux.
Children who continue to have urinary tract infections despite the antibiotics, or still have severe reflux after the age of five years old might need an operation to correct the problem causing VUR. In this operation, called ureteric reimplantation, the ureters are disconnected from the bladder and re-attached at an angle to create a valve. Now a day, this surgery can also be done endoscopically.
Consequences of VUR?
Untreated VUR may lead to problems like poor weight gain, poor appetite, urinary tract infections and late onset hypertension or end stage renal failure.
Vomiting
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
VOMITING
Vomiting is quite commonly seen in children and may not be an indication of any disease. However, recurrent vomiting associated with weight loss would warrant a consultation by a child specialist. It is important to note the quantity, frequency and color of vomiting. Vomiting associated with loose stools (diarrhea) is a sign of intestinal infection.
White Vomits: Recurrent white vomiting can be because of two main surgical problems:
a) Gastroesophageal reflux (GER): This is retrograde flow of stomach contents back into the oesophagus.
b) Pyloric Stenosis: Commonly seen at the age of 1 month, where the child has large and projectile vomits.
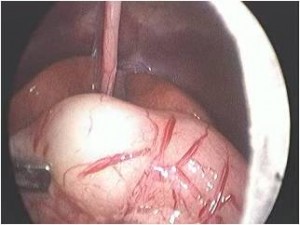 Pyloric Stenosis
Pyloric Stenosis 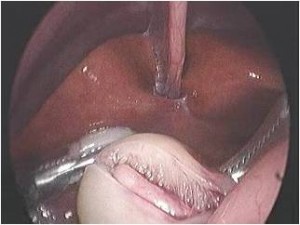 At Surgery
At Surgery
Green Vomits: Green vomiting is the sign of a serious problem and medical attention needs to be sought urgently. Green vomiting in a newborn child is almost invariably a cause of intestinal obstruction. ●
 Malrotation of intestine (A very common cause of green vomiting in neonates and infants)
Malrotation of intestine (A very common cause of green vomiting in neonates and infants)
GUJARATI
ઉલ્ટી
ઉલ્ટી બાળકોમાં સર્વસામાન્ય છે અને ઘણીવાર તે કોઈ બીમારીનું કારણ નથી હોતું. પરંતુ ઉલ્ટી વારંવાર થવાનાં કારણે બાળકનું વજન વધતું અટકે અથવા ઘટવા માંડે તો અચૂક ડાક્ટરી તપાસ જરૂરી છે.
ઉલ્ટીનું પ્રમાણ અને નંબર ઉપરાંત તેનો રંગ જાણવો જરૂરી છે. ઉલ્ટી સાથે પાતળા ઝાડા થવા એ આંતરડાનાં ઇન્ફેક્શનનું કારણ છે.
૧. સફેદ કલરની ઉલ્ટી ઃ મુખ્ય બે કારણો
– ગેસ્ટ્રો ઇસોફેઝીયલ રીફલકસ ઃ ખોરાક/દૂધ હોજરીમાં ગયા બાદ અન્નનળીમાં પરત આવે/બેક મારે.
– પાયલોરીક સ્ટેનોસીસ ઃ હોજરીના આગળના ભાગમાં અવરોધના કારણે ઉલ્ટી થાય. સામાન્ય રીતે ૧ માસના બાળકમાં આ બીમારી થાય છે અને તે માટે આૅપરેશન કરવું પડે છે.
૨. લીલા કલરની ઉલ્ટી ઃ આ એક ગંભીર બીમારીની નિશાની છે અને જલ્દી ડાક્ટરની સલાહ લેવી જરૂરી છે. નવજાત શિશુમાં લીલી ઉલ્ટી આંતરડામાં જન્મજાત અવરોધના કારણે હોય છે, માટે યોગ્ય તપાસ અને ટ્રીટમેન્ટ કરાવવી જરૂરી છે. •
HINDI
उल्टी
बच्चों में उल्टी की शिकायत एक आम बात है और यह किसी प्रकार की बीमारी का लक्षण नहीं दर्शाता। लेकिन बार-बार उल्टी होने के कारण बच्चे का वजन घटने से बचाने के लिए डॉक्टर से जरूर संपर्क करना चाहिए। उल्टी की मात्रा के अतिरिक्त उसके रंग के बारे में जानना भी आवश्यक है। उल्टी के साथ दस्त होना आंतो में संक्रमण के कारण हो सकता है।
१)सफेद रंग की उल्टी होने का कारणः मुख्य दो कारण
गेस्ट्रो इसोफेझीयल रीफ्लक्सः खुराक/दूध पेट में जाने के बाद अन्ननली में वापस आता है।
पायलोरीक स्टेनोसीसः आंतों के अगले भाग में अवरोध के कारण उल्टी होती है। सामान्यतः यह बीमारी एक माह की आयु के बच्चे में होती है और इसके लिए ऑपरेशन करना पड़ता है।
२) हरे रंग की उल्टी : यह एक गंभीर बीमारी का लक्षण है और तुरंत डॉक्टर से परामर्श करना आवश्यक है। नवजात शिशु के मामले में हरे रंग की उल्टी होना आंतों में जन्मजात अवरोध के कारण होती है। अतः उचित जांच एवं उपचार करने की आवश्यकता होती है।•
Vitello Intestinal Duct / Omphalomesenteric Duct
INFORMATION AVAILABLE IN ENGLISH, GUJARATI AND HINDI
Vitello Intestinal Duct / Omphalomesenteric Duct
In the human embryo, the vitelline duct also known as the omphalomesenteric duct is a long narrow tube that joins the yolk sac to the midgut of the developing fetus. Generally, the duct narrows and disappears by the 9th week of intrauterine life. However, failure of the duct to close is termed as patent vitellointestinal duct or vitellointestinal fistula. This results in discharge of intestinal contents from the umbilicus. Sometimes it may emit foul smelling fluid discharge keeping the umbilicus persistently wet.
It is very difficult to pick up a patent vitello intestinal duct on ultrasound or by any other form of imaging. The only way to diagnose and treat this problem is laparoscopy. If need be, the native segment of the intestine connecting with the vitello-intestinal duct needs to be resected. ●
દૂંટી સાથે જાડાયેલું આંતરડું
આ પણ એક જન્મજાત ખોડ છે, જેમાં બાળકની નાળ કપાયા પછી દૂંટીની રૂઝ આવતી નથી અને દૂંટીમાંથી ચીકાશ, પાણી અને ઘણીવાર મળ જેવું વાસ મારતું પ્રવાહી આવે છે. જ્વલ્લેજ પાતળો સંડાસ પણ દૂંટી વાટે આવે છે.
આ ખોડનું કારણ નાનું આંતરડું દૂંટી સાથે જાડાયેલું રહેવાથી અથવા આંતરડાનો નાનો ભાગ દૂંટીમાં રહી જવાથી થાય છે.
દૂંટીનો મસો છે તેમ માની નિદાનમાં સમય ન બગાડતાં જરૂર પડે બાળકોનાં સર્જનની સલાહ લેવી જરૂરી છે. સોનોગ્રાફી તથા એક્ષ-રે આ પ્રકારની ખોડનાં નિદાનમાં મદદરૂપ થતાં નથી.
આધુનિક બાળસર્જરીની શોધને લીધે આ પ્રકારની ખોડની સારવાર લપ્રોસ્કોપીથી (દૂરબીન વડે ) કરવામાં આવે છે. જરૂર પડે આંતરડાનાં ભાગને પણ કાપીને જાઇન્ટ કરવો પડે છે. •
नाभि के साथ आंत का जुडा होना
मानव भ्रूण में, पीतक वाहिनी, जिसे ओम्फेलोमीसेंट्रीक डक्ट भी कहते हैं, एक लम्बी संकरी नलिका होती है जो अंडे की जर्दी की थैली को विकसित हो रहे भ्रूण के आद्यमध्यांत्र के साथ जोड़ती है। सामन्यतः यह नलिका संकरी होकर अंतर्गर्भाशयी काल के नौवे सप्ताह तक अदृश्य हो जाती है। तथापि, नलिका के बंद न हो सकने की स्थिति को पेटेंट विटीलोइंटेस्टीनल डक्ट अथवा विटीलोइंटेस्टीनल फिस्चुला कहते हैं। इसके परिणाम स्वरूप आंत्र सामग्री का नाभि से रिसाव हो सकता है। कभी-कभी इसमें से दुर्गंधयुक्त रसों का रिसाव हो सकता है, जिस कारण नाभि हमेशा गीली रहेगी।
अल्ट्रासाउंड या अन्य किसी अन्य प्रकार की इमेजिंग के द्वारा पेटेंट विटीलोइंटेस्टीनल डक्ट का पता लगाना कठीन है। लेप्रोस्कोपी ही इस समस्या के निदान और उपचार का एक मात्र तरीका है। यदि आवश्यक हो, विटीलोइंटेस्टनल डक्ट के साथ जुड़े आंत के जन्मज भाग को विभाजित कर दिया जाता है। •
Video Assisted Thoracic Surgery (VATS) / Thoracoscopy
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout. The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making it look like readable English. Many desktop publishing packages and web page editors now use Lorem Ipsum as their default model text, and a search for ‘lorem ipsum’ will uncover many web sites still in their infancy. Various versions have evolved over the years, sometimes by accident, sometimes on purpose (injected humour and the like).
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout. The point of using Lorem Ipsum is that it has a more-or-less normal distribution of letters, as opposed to using ‘Content here, content here’, making it look like readable English. Many desktop publishing packages and web page editors now use Lorem Ipsum as their default model text, and a search for ‘lorem ipsum’ will uncover many web sites still in their infancy. Various versions have evolved over the years, sometimes by accident, sometimes on purpose (injected humour and the like).
INFORMATION AVAILABLE IN ENGLISH / GUJARATI AND HINDI
VIDEO ASSISTED THORACIC SURGERY (VATS)
VATS is a technique which involves surgery for various pathologies in the chest using key hole surgery. This is commonly known as thoracoscopy. Thoracic surgeries used to be done using large incisions. However, with technical advances and surgical expertise, these can now be done using 3 and 5 mm instruments.
Throacoscopy is commonly performed for the following pathologies in children :
- Empyema (Pus in the chest)
- Lobectomies – Removal of the part of the lung
- Cysts in the lung ( e.g. hydatid cysts, bronchogenic cysts)
- Cysts of the oesophagus (e.g. duplication cysts)
- Tumors in the chest (Tuberculosis, malignant tumors)
- Thymic tumors
- Diaphragmatic hernias
- Oesophageal atresias with tracheo-esophageal fistulas
GUJARATI
થોરેકોસ્કોપી
થોરેકોસ્કોપી નાના છિદ્રો દ્વારા છાતીનાં રોગો માટે દૂરબીનથી આૅપરેશન કરવાની ટેકનિક છે. ‘લેપ્રોસ્કોપી’ પેટનાં આૅપરેશન માટે છે. ‘થોરેકોસ્કોપી’ છાતીના આૅપરેશન માટે છે.
છાતીનાં આૅપરેશન પહેલાં ખૂબ મોટા કાપા પાડી કરવામાં આવતાં હતાં. પણ આધુનિક ટેકનોલોજી અને સર્જનની કુશળતા થી હવે ૩ મીમી અથવા ૫ મીમી નાં નાના નાના છિદ્ર દ્વારા જટિલ છાતીનાં આૅપરેશન કરવામાં આવે છે.
થોરેકોસ્કોપી દ્વારા થતાં મુખ્ય આૅપરેશનો :
૧) બાળકની છાતીમાં પરૂ થવું (ઍમ્પાઈમા)
૨) ફેફસાંનો અમુક ભાગ ખરાબ હોય તો તે કાઢવાના આૅપરેશન
૩) ફેફસાંમાં સીસ્ટ હોય (દા.ત. હાયડેટીડ સીસ્ટ )
૪) અન્નનળીની ગાંઠો ( ડૂપ્લિકેશન સીસ્ટ)
૫) છાતીમાં ટી.બી. અથવા કેન્સરની ગાંઠ.
૬) નવજાત બાળકમાં શ્વાસનળી અને અન્નનળી જાઇન્ટ હોય.
૭) થાયમસ ગ્રંથિની ગાંઠનું આૅપરેશન.
આમ, અનેક પ્રકારનાં બાળકોના છાતીનાં રોગોનું આૅપરેશન થોરેકોસ્કોપી દ્વારા સર્જન સહેલાઈથી કરી શકે. આૅપરેશન બાદ દુઃખાવો પણ ખૂબ ઓછો થાય છે અને બાળકને હાÂસ્પટલમાંથી પણ વહેલી રજા મળી શકે છે.
આ આૅપરેશન ઓપન આૅપરેશનથી વધુ ખર્ચાવાળા નથી હોતાં. •
HINDI
थोरेकोस्कोपी
यह सर्जरी छाती के विभिन्न रोगों के लिए छोटे छिद्र करके दूरबीन से ऑपरेशन करने की तकनीक है। इसे सामान्य तौर पर थोरेकोस्कोपी कहा जाता है।
छाती के रोगों के लिए पहले के समय में बहुत बड़ा चीरा करके ऑपरेशन किया जाता था। लेकिन आधुनिकी उन्नत तकनीकों और सर्जन की विशेषज्ञाता से अब ३द्वद्व और ५द्वद्व के छोटे छेद करके इतने ही आकार के उपकरणों से छाती के जटिल ऑपरेशन किये जाते हैं।
मुख्य रूप से यह ऑपरेशन बच्चों में नीचे दिये गये रोगों के लिए किया जाता हैः
१) बच्चे की छाती में मवाद (Empyema)
२) फेफडों के किसी खराब हिस्से को ऑपरेशन से निकालना
३) फेफडों में सिस्ट (जैसे की Hydatid सीस्ट)
४) आहारनली की गांठे (डुप्लीकेशन सीस्ट)
५) छाती में टी.बी. या कैंसर की गांठ
६) नवजात शिशु की श्वासनली और अन्ननली जॉइन्ट होने पर
७) थाइमस ग्रंथि की गांठ
इस प्रकार बच्चों की छाती के रोगों के कई ऑपरेशन थोरेकोस्कोपी द्वारा सर्जन बहुत ही कुशलता से करते हैं। इस ऑपरेशन से बच्चे को बहुत कम दर्द होता है और अस्पताल से जल्दी छुट्टी मिल जाती है। ये ऑपरेशन ओपन ऑपरेशन से अधिक खर्चीले नहीं होते। •
No categories available for this letter
No categories available for this letter
No categories available for this letter